Bruising at the injection site is a recognised, though uncommon, reaction to Ozempic (semaglutide), a once-weekly subcutaneous treatment for type 2 diabetes. This occurs when the needle inadvertently damages small blood vessels beneath the skin, causing localised bleeding into surrounding tissues. Whilst typically benign and self-limiting, bruising can be distressing and may be more pronounced in patients taking anticoagulants or with fragile skin. Understanding why bruising occurs, how to minimise it through correct injection technique, and when to seek medical advice can help patients manage this side effect confidently and maintain treatment adherence.
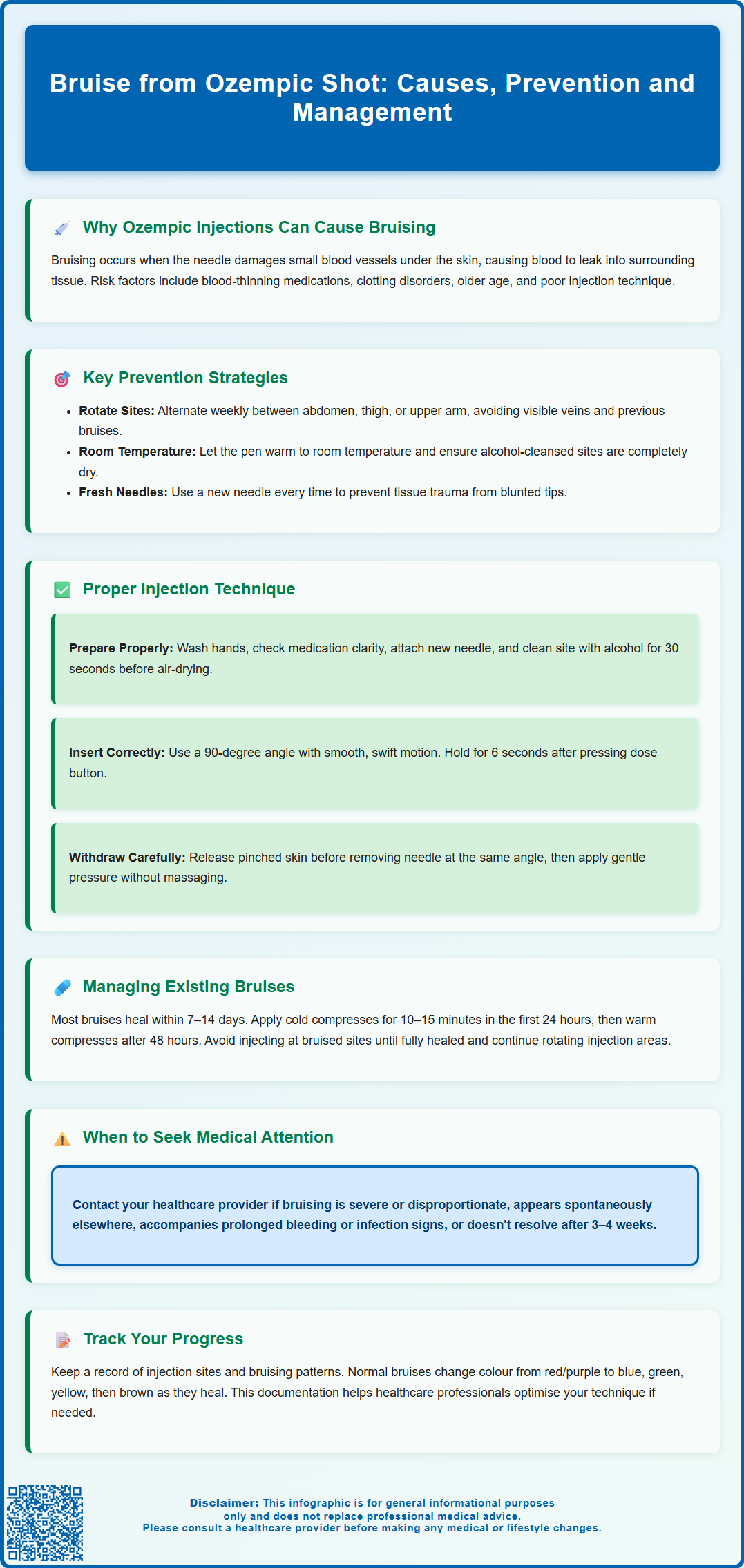
Summary: Bruising from Ozempic injections occurs when the needle damages small blood vessels beneath the skin, causing localised bleeding that typically resolves within 7–14 days without treatment.
- Ozempic (semaglutide) is a GLP-1 receptor agonist administered as a once-weekly subcutaneous injection for type 2 diabetes.
- Bruising risk increases with anticoagulant or antiplatelet use, incorrect injection technique, and skin fragility.
- Rotating injection sites, using proper 90-degree needle insertion, and applying post-injection pressure reduce bruising.
- Most bruises resolve spontaneously; seek medical review if bruising is severe, recurrent, or accompanied by unusual bleeding elsewhere.
- Report suspected adverse reactions to the MHRA Yellow Card Scheme for pharmacovigilance monitoring.
Table of Contents
Why Ozempic Injections Can Cause Bruising
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, Ozempic works by enhancing insulin secretion in response to elevated blood glucose, suppressing glucagon release, and slowing gastric emptying. While injection-site reactions are classified as uncommon in the official product information, bruising can occur at the injection site.
Bruising occurs when small blood vessels (capillaries) beneath the skin are damaged during needle insertion, causing blood to leak into surrounding tissues. The subcutaneous layer—where Ozempic is injected—contains a network of capillaries that can be inadvertently punctured. Factors that increase bruising risk include:
-
Needle trauma: Even with fine-gauge needles, capillary damage can occur, particularly if the needle strikes a vessel directly.
-
Injection technique: Rapid needle insertion, incorrect angle, or failure to release pinched skin before withdrawing the needle may exacerbate tissue trauma.
-
Individual susceptibility: Patients taking anticoagulants (e.g., warfarin, apixaban) or antiplatelet agents (e.g., aspirin, clopidogrel) are at heightened risk. Conditions affecting clotting, such as thrombocytopenia or von Willebrand disease, also predispose to bruising.
-
Skin fragility: Older adults or those on long-term corticosteroids may have thinner, more fragile skin.
It is important to note that bruising from Ozempic injections is typically a benign, self-limiting reaction and does not indicate treatment failure or serious adverse effects. However, persistent or severe bruising, particularly if accompanied by unusual bleeding elsewhere, warrants medical review to exclude underlying haematological disorders.
How to Reduce Bruising from Ozempic Shots
Minimising bruising from Ozempic injections involves a combination of careful site selection, pre-injection preparation, and post-injection care. Evidence-based strategies to reduce bruising include:
Site rotation and selection: Ozempic should be injected into areas with adequate subcutaneous fat—the abdomen (avoiding a 5 cm radius around the navel), thigh, or upper arm. Note that upper-arm injections should generally be administered by another person, as recommended in the Patient Information Leaflet. Rotating injection sites weekly prevents repeated trauma to the same area. Avoid injecting into areas with visible veins, bruises, scars, or skin abnormalities.
Pre-injection preparation: Allow the Ozempic pen to reach room temperature before injecting, as cold medication can cause discomfort. Cleanse the injection site with an alcohol wipe and allow it to dry completely—injecting through wet alcohol can cause stinging and tissue irritation.
Timing considerations for anticoagulated patients: Patients on anticoagulants or antiplatelets should not stop their medication before Ozempic injections unless specifically advised by their healthcare professional. Instead, apply firm pressure to the injection site for at least 2 minutes after injection and be particularly meticulous with technique. Discuss any concerns with your GP or diabetes specialist nurse.
Post-injection care: After withdrawing the needle, apply gentle pressure with a clean cotton wool ball or gauze for 5–10 seconds (longer if on blood-thinning medication). Avoid rubbing the site, as this can disperse medication and worsen bruising. If minor bleeding occurs, maintain pressure until it stops.
Needle quality: Use a new needle for each injection as recommended in the Ozempic Patient Information Leaflet. Reusing needles causes blunting, which increases tissue trauma and infection risk. Never share pens or needles with others.
These measures, when applied consistently, can significantly reduce the frequency and severity of injection-site bruising.
Proper Injection Technique to Minimise Bruising
Correct injection technique is fundamental to minimising bruising and ensuring optimal drug delivery. The following step-by-step approach aligns with the manufacturer's instructions and UK injection technique recommendations:
1. Preparation: Wash hands thoroughly and gather supplies—Ozempic pen, new needle, alcohol wipe, and cotton wool. Check the medication is clear and colourless; do not use if cloudy or discoloured.
2. Attach the needle: Remove the pen cap and attach a new needle securely. Remove both the outer and inner needle caps. Prime the pen as per manufacturer instructions to ensure proper flow.
3. Select and prepare the site: Choose an injection site with adequate subcutaneous tissue. Cleanse with an alcohol wipe using a circular motion and allow to air-dry for at least 30 seconds.
4. Pinch technique: This is primarily needed for very lean individuals or when using longer needles. If required, gently pinch a fold of skin between thumb and forefinger to lift the subcutaneous layer away from underlying muscle. Avoid pinching too tightly, as excessive pressure can damage capillaries.
5. Needle insertion: Hold the pen at a 90-degree angle to the skin (or 45 degrees if very lean). Insert the needle with a smooth, swift motion—hesitation can increase discomfort and trauma. Press the dose button fully and hold for 6 seconds to ensure complete delivery, as directed in the Ozempic Patient Information Leaflet.
6. Withdrawal: Release the pinched skin before withdrawing the needle. This prevents medication leakage and reduces tissue trauma. Withdraw the needle at the same angle it was inserted, using a smooth, steady motion.
7. Post-injection: Apply gentle pressure if needed, but do not massage. Dispose of the needle immediately in a sharps container. Sharps bins can be obtained from your GP surgery, pharmacy, or local council, and should be returned when three-quarters full.
Patients uncertain about technique should request a demonstration from their practice nurse or diabetes specialist. Many NHS trusts offer injection technique reviews as part of routine diabetes care.
Managing and Treating Bruises from Ozempic
Most bruises from Ozempic injections are minor and resolve spontaneously within 7–14 days without specific treatment. However, appropriate management can accelerate healing and provide symptomatic relief:
Immediate care: If bruising develops, avoid further injections at that site until fully healed. Apply a cold compress (wrapped ice pack or frozen peas in a towel) for 10–15 minutes within the first 24 hours to reduce blood flow and limit bruise size. Do not apply ice directly to skin.
Subsequent care: After 24–48 hours, gentle warmth (warm compress) may help disperse accumulated blood and promote healing. Over-the-counter arnica cream is sometimes used, though evidence for its efficacy is limited. Consult your healthcare professional before starting any additional over-the-counter pain relievers if you are already taking anticoagulants or antiplatelets.
Monitoring: Bruises typically progress through colour changes—red/purple initially, then blue, green, yellow, and finally brown before fading. This is normal haemoglobin breakdown. Seek medical attention if:
-
Bruising is severe, extensive, or disproportionate to the injection
-
New bruises appear spontaneously at non-injection sites
-
Bruising is accompanied by prolonged bleeding, petechiae (pinpoint red spots), or mucosal bleeding (nosebleeds, gum bleeding)
-
Signs of infection develop (increasing pain, warmth, redness, swelling, or discharge)
-
Bruises fail to resolve after 3–4 weeks
Documentation: Keep a record of injection sites and any bruising patterns. This information is valuable for healthcare professionals in optimising your injection technique or investigating potential underlying causes.
Patients experiencing recurrent, problematic bruising should discuss this with their GP or diabetes team. Semaglutide is not known to affect clotting function, but persistent bruising may warrant investigation, particularly in patients with additional risk factors. Your healthcare team can provide individualised advice and, if necessary, refer you to haematology services for specialist assessment.
If you suspect an adverse reaction to Ozempic, report it to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Is bruising from Ozempic injections dangerous?
Bruising from Ozempic is typically benign and self-limiting, resolving within 7–14 days. However, severe, recurrent, or widespread bruising warrants medical review to exclude underlying clotting disorders.
Should I stop taking blood thinners before my Ozempic injection?
No, do not stop anticoagulants or antiplatelets unless specifically advised by your healthcare professional. Instead, apply firm pressure for at least 2 minutes after injection and use meticulous technique.
How can I prevent bruising when injecting Ozempic?
Rotate injection sites weekly, use a 90-degree needle angle, allow the pen to reach room temperature, let alcohol dry completely before injecting, and apply gentle pressure post-injection without rubbing the site.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










