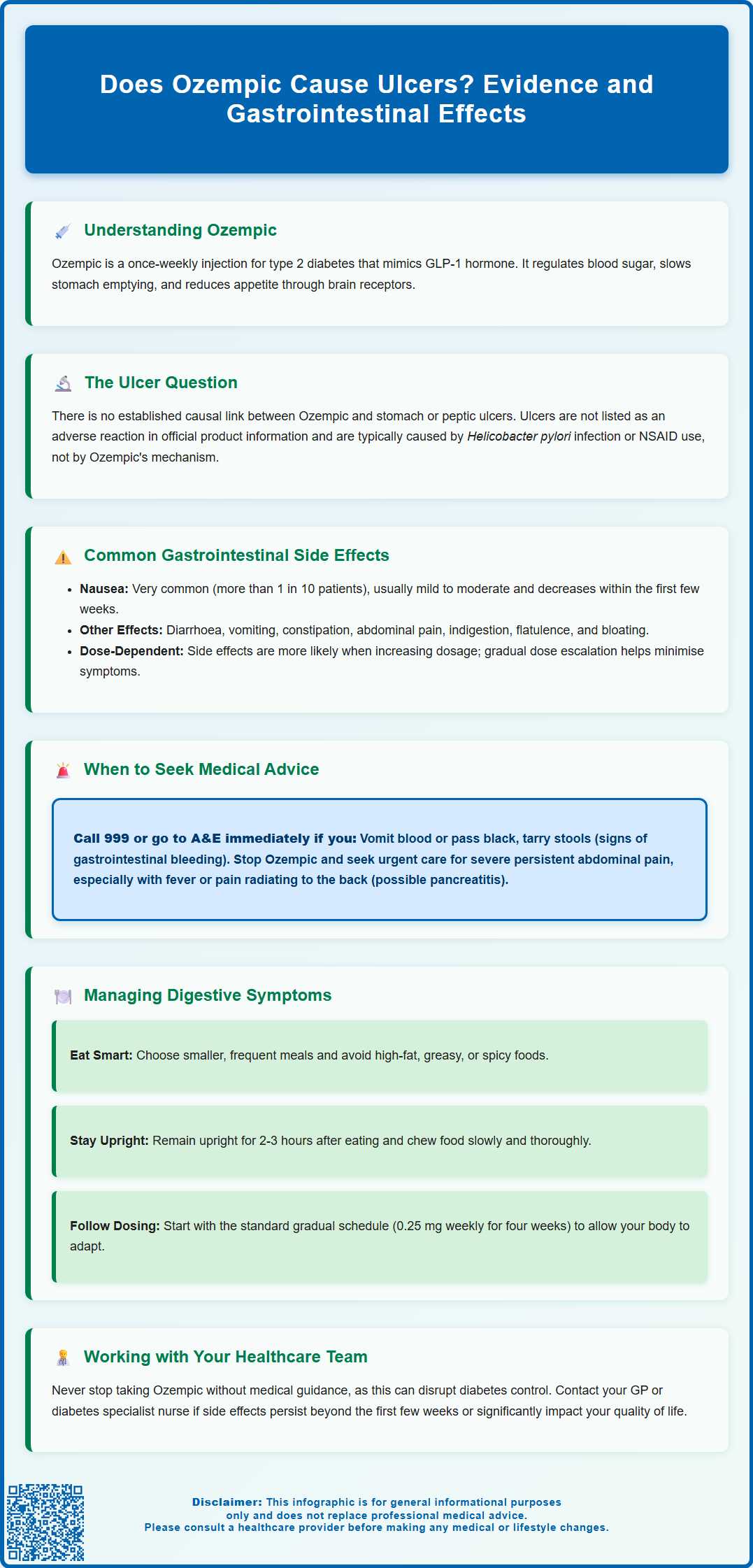
Does Ozempic cause ulcers? This is a common concern amongst patients prescribed this type 2 diabetes medication. Ozempic (semaglutide) is a GLP-1 receptor agonist that affects the digestive system, leading to frequent gastrointestinal side effects. Whilst nausea, vomiting, and abdominal discomfort are well-documented, there is currently no established causal link between Ozempic and the development of gastric or peptic ulcers. Understanding the distinction between common digestive side effects and serious complications is essential for patients and healthcare professionals. This article examines the evidence regarding Ozempic and ulcer risk, explores gastrointestinal effects, and provides guidance on when to seek medical advice.
Summary: There is currently no established causal link between Ozempic (semaglutide) and the development of gastric or peptic ulcers.
- Ozempic is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus, administered as a once-weekly subcutaneous injection.
- The medication slows gastric emptying and commonly causes gastrointestinal side effects including nausea, vomiting, diarrhoea, and abdominal pain, particularly during treatment initiation.
- Peptic ulcers are not listed as an adverse reaction in the UK Summary of Product Characteristics for Ozempic.
- Patients experiencing persistent upper abdominal pain, black tarry stools, or vomiting blood should seek urgent medical attention regardless of Ozempic use.
- Rare but serious gastrointestinal complications include pancreatitis and cholecystitis, which require immediate discontinuation and urgent medical assessment.
Table of Contents
Understanding Ozempic and Its Gastrointestinal Effects
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, it works by mimicking the action of the naturally occurring hormone GLP-1, which plays a crucial role in glucose regulation and appetite control.
The mechanism of action of semaglutide involves several pathways that affect the gastrointestinal system. It stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, and slows gastric emptying. This delayed gastric emptying is particularly relevant when considering gastrointestinal side effects, as it means food remains in the stomach for longer periods. This effect is most pronounced during initial treatment and tends to lessen with continued use. Additionally, semaglutide acts on receptors in the brain to reduce appetite and promote satiety, contributing to its weight loss effects.
Given semaglutide's effects on the digestive system via GLP-1 receptors and neural pathways, it is unsurprising that digestive side effects are among the most commonly reported adverse reactions to Ozempic. The MHRA's Summary of Product Characteristics highlights that gastrointestinal disorders occur frequently, particularly during the initial weeks of treatment or following dose escalation. Understanding how Ozempic interacts with the digestive system is essential for both patients and healthcare professionals to distinguish between expected side effects and more serious complications.
Patients prescribed Ozempic should be informed that whilst gastrointestinal symptoms are common, they typically improve over time as the body adjusts to the medication. However, awareness of the full spectrum of potential digestive effects enables appropriate monitoring and timely intervention when necessary.
Can Ozempic Cause Stomach or Peptic Ulcers?
There is currently no established causal link between Ozempic and the development of gastric (stomach) or peptic ulcers. Peptic ulcers are not listed as an adverse reaction in the UK Ozempic Summary of Product Characteristics. Peptic ulcers are localised areas of erosion in the lining of the stomach or duodenum, typically caused by infection with Helicobacter pylori bacteria or the use of non-steroidal anti-inflammatory drugs (NSAIDs). The pathophysiology of ulcer formation involves an imbalance between protective factors (mucus, bicarbonate) and aggressive factors (acid, pepsin) in the gastric environment.
Semaglutide's mechanism of action does not directly compromise the protective mucosal barrier or increase gastric acid secretion in ways known to promote ulcer formation. Clinical trials conducted during the drug's development and post-marketing surveillance have not identified a significant association between semaglutide use and increased ulcer incidence.
However, it is important to note that delayed gastric emptying caused by Ozempic could theoretically affect the presentation or symptoms of pre-existing gastrointestinal conditions. Patients with undiagnosed ulcers might experience altered symptom patterns. Clinical pharmacology studies have shown no clinically relevant effect on the absorption of oral medications, though monitoring of INR is advised for patients taking warfarin or other coumarin anticoagulants.
If you are taking Ozempic and experience symptoms suggestive of an ulcer—such as persistent upper abdominal pain, particularly when the stomach is empty, pain that improves with eating or antacids, or signs of bleeding such as black, tarry stools or vomiting blood—you should seek urgent medical attention. For signs of gastrointestinal bleeding (vomiting blood or passing black, tarry stools), call 999 or go to A&E immediately. These symptoms warrant investigation regardless of Ozempic use, as peptic ulcers require appropriate diagnosis and treatment to prevent complications such as bleeding or perforation.
Gastrointestinal Side Effects Associated with Ozempic
The most frequently reported adverse effects of Ozempic involve the gastrointestinal system, affecting a substantial proportion of patients, particularly during treatment initiation. According to the MHRA-approved product information, nausea is very common, occurring in more than 1 in 10 patients. This is typically mild to moderate in severity and tends to diminish over the first few weeks of therapy.
Other common gastrointestinal side effects (affecting between 1 in 10 and 1 in 100 patients) include:
-
Diarrhoea
-
Vomiting
-
Constipation
-
Abdominal pain or discomfort
-
Dyspepsia (indigestion)
-
Flatulence and bloating
These effects are generally dose-dependent, meaning they are more likely to occur or worsen when the dose is increased. The standard titration schedule for Ozempic, which starts at 0.25 mg weekly and gradually increases, is specifically designed to minimise gastrointestinal intolerance by allowing the body time to adapt.
In rare cases, more serious gastrointestinal complications have been reported with GLP-1 receptor agonists. Pancreatitis (inflammation of the pancreas) is an uncommon but recognised adverse effect. If pancreatitis is suspected, Ozempic should be discontinued immediately and urgent medical attention sought. Cholelithiasis (gallstones) and cholecystitis (gallbladder inflammation) have also been reported. There have been post-marketing case reports of severe delayed gastric emptying, though this is not listed as an established adverse reaction in the UK Ozempic SmPC.
Symptoms of pancreatitis include severe, persistent abdominal pain that may radiate to the back, often accompanied by nausea and vomiting. Gallbladder problems may present with right upper abdominal pain, particularly after fatty meals.
NICE guidance (NG28) on type 2 diabetes management emphasises the importance of patient education regarding expected side effects and the need for appropriate monitoring, particularly in the early stages of treatment.
Risk Factors and When to Seek Medical Advice
Certain patient characteristics may increase the likelihood or severity of gastrointestinal side effects when taking Ozempic. Understanding these risk factors helps healthcare professionals identify patients who may require closer monitoring or additional support during treatment.
Pre-existing gastrointestinal conditions represent an important consideration. According to the Ozempic SmPC, use is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis. Patients with a history of gastroparesis or other chronic digestive disorders may experience exacerbation of symptoms due to Ozempic's effect on gastric motility. Those with previous pancreatitis should be prescribed GLP-1 receptor agonists with caution, as there have been post-marketing reports of pancreatitis in patients taking semaglutide, though a definitive causal relationship remains uncertain.
Concurrent medications can also influence gastrointestinal tolerability. While clinical studies have shown no clinically relevant effect on the absorption of oral medications, monitoring of INR is advised for patients taking warfarin or other coumarin anticoagulants. Dose adjustments of concomitant medications are usually not required.
You should seek medical advice promptly if you experience:
-
Severe or persistent abdominal pain, especially if accompanied by fever or vomiting – seek urgent medical attention if severe and persistent
-
Signs of gastrointestinal bleeding – black, tarry stools, blood in vomit, or vomit resembling coffee grounds – call 999 or go to A&E immediately
-
Severe, persistent nausea or vomiting that prevents adequate fluid or food intake, risking dehydration and potential kidney problems
-
Symptoms of pancreatitis – severe upper abdominal pain radiating to the back – stop taking Ozempic and seek urgent medical attention
-
Jaundice (yellowing of skin or eyes) or pale stools, which may indicate gallbladder or liver problems
-
Unexplained, rapid weight loss or inability to maintain adequate nutrition
Patients should contact their GP or diabetes specialist nurse if gastrointestinal side effects persist beyond the first few weeks of treatment or significantly impact quality of life. In some cases, dose adjustment, temporary treatment interruption, or switching to an alternative medication may be appropriate. Never stop taking Ozempic without consulting your healthcare provider, as abrupt discontinuation can affect diabetes control.
If you suspect you're experiencing side effects from Ozempic, you can report these through the MHRA Yellow Card Scheme, which helps monitor the safety of medicines.
Managing Digestive Symptoms While Taking Ozempic
Effective management of gastrointestinal side effects can significantly improve treatment adherence and patient experience with Ozempic. Most digestive symptoms are self-limiting and respond well to conservative measures, particularly during the initial adjustment period.
Dietary modifications represent the first-line approach to managing nausea and other digestive symptoms:
-
Eat smaller, more frequent meals rather than large portions, which can overwhelm the already-slowed digestive system
-
Avoid high-fat, greasy, or spicy foods, as these are more difficult to digest and may exacerbate nausea
-
Stay well hydrated, sipping water throughout the day rather than drinking large amounts at once
-
Eat slowly and chew thoroughly to aid digestion and reduce bloating
-
Avoid lying down immediately after eating; remain upright for at least 2–3 hours after meals
-
Identify and avoid personal trigger foods that worsen symptoms
According to the SmPC, Ozempic can be administered at any time of day, with or without meals. The long half-life of semaglutide means that the timing of the injection is unlikely to significantly affect the occurrence of gastrointestinal symptoms.
Before taking over-the-counter medications for symptom relief, always consult your pharmacist or GP to check for potential interactions. For patients with significant nausea, prescription antiemetics may occasionally be warranted during the initial treatment phase.
Gradual dose titration is crucial. The standard Ozempic dosing schedule begins at 0.25 mg weekly for four weeks, increasing to 0.5 mg weekly, with further increases to 1 mg or 2 mg if needed for glycaemic control. This gradual escalation allows the gastrointestinal system to adapt. If side effects are problematic, your healthcare provider may recommend remaining at a lower dose for a longer period before increasing, or temporarily reducing the dose until symptoms improve.
Regular follow-up with your diabetes care team ensures appropriate monitoring of both treatment efficacy and tolerability. The NHS provides diabetes specialist nurses and dietitians who can offer tailored advice on managing side effects whilst maintaining good diabetes control and nutritional status. Remember that whilst gastrointestinal side effects are common, they should not be dismissed if they significantly impact your wellbeing or ability to maintain adequate nutrition.
Frequently Asked Questions
Can Ozempic cause stomach ulcers?
There is no established causal link between Ozempic and stomach or peptic ulcers. Peptic ulcers are not listed as an adverse reaction in the UK Summary of Product Characteristics for Ozempic.
What are the most common gastrointestinal side effects of Ozempic?
The most common gastrointestinal side effects include nausea (affecting more than 1 in 10 patients), diarrhoea, vomiting, constipation, abdominal pain, and dyspepsia. These effects typically improve over the first few weeks of treatment.
When should I seek urgent medical attention whilst taking Ozempic?
Seek immediate medical attention if you experience signs of gastrointestinal bleeding (black, tarry stools or vomiting blood), severe persistent abdominal pain radiating to the back (possible pancreatitis), or jaundice. Call 999 or go to A&E for bleeding symptoms.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript