Which GLP-1 has less nausea is a common concern for patients and clinicians selecting glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes or weight management. Nausea is one of the most frequently reported adverse effects of this medication class, occurring because GLP-1 agonists slow gastric emptying—a mechanism that improves glycaemic control but can cause gastrointestinal discomfort. Current evidence suggests that dulaglutide and extended-release formulations generally demonstrate lower nausea rates compared to twice-daily exenatide or higher-dose semaglutide and liraglutide. However, individual responses vary considerably, and gradual dose titration alongside dietary modifications can significantly improve tolerability across all GLP-1 preparations.
Summary: Dulaglutide and extended-release GLP-1 formulations generally demonstrate lower nausea rates compared to twice-daily exenatide or higher-dose semaglutide and liraglutide, though individual responses vary considerably.
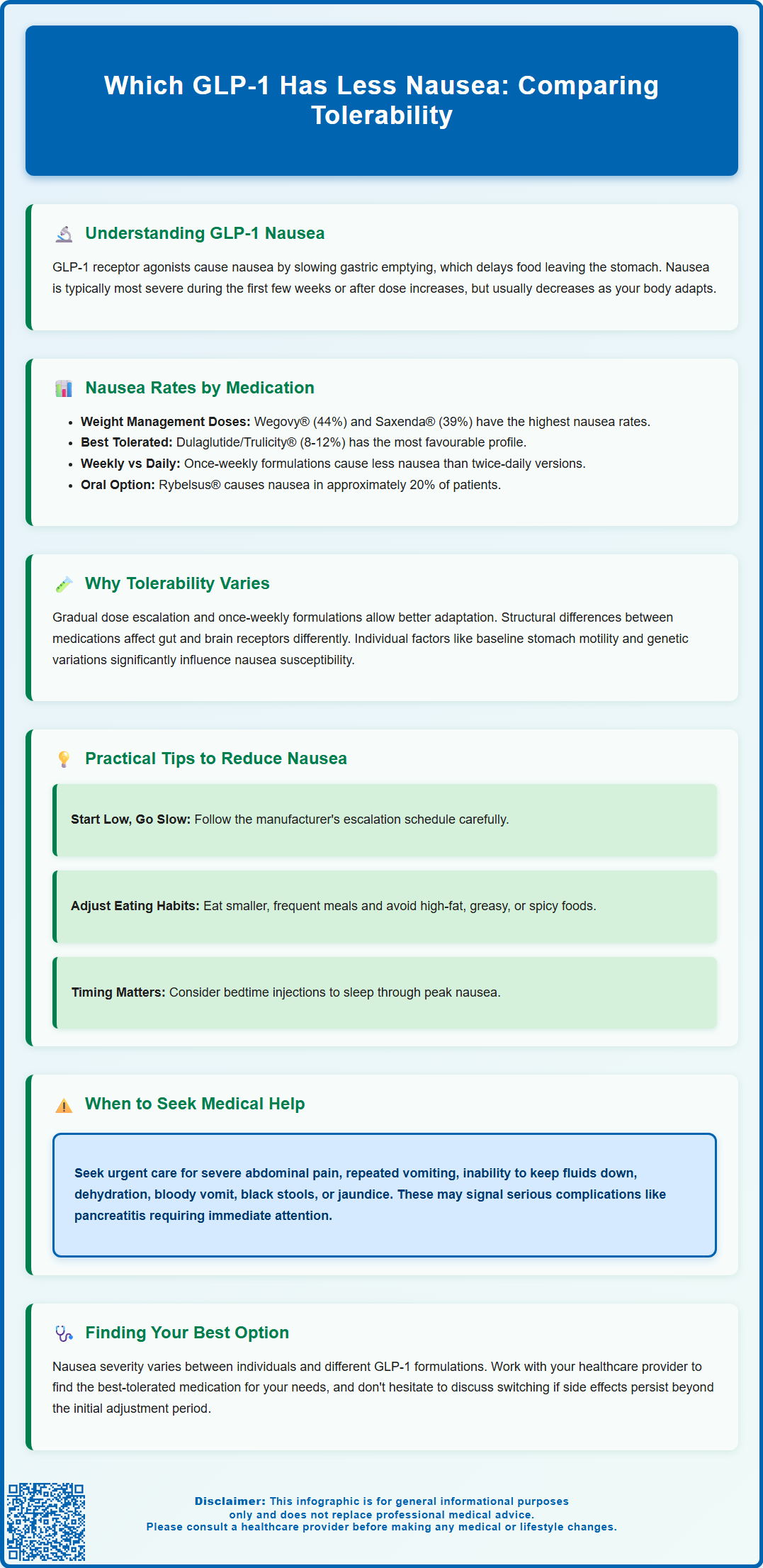
- GLP-1 receptor agonists cause nausea by delaying gastric emptying, with rates varying from 8% to 44% depending on the specific medication and dose.
- Dulaglutide shows nausea rates of approximately 8-12% at lower doses, whilst semaglutide (Wegovy) demonstrates rates around 44% in weight management trials.
- Once-weekly formulations typically provide more stable plasma concentrations with lower peak levels, potentially reducing gastrointestinal side effects compared to shorter-acting preparations.
- Gradual dose titration, smaller frequent meals, avoiding high-fat foods, and staying well hydrated can significantly reduce nausea with GLP-1 therapy.
- Patients should seek urgent medical attention for severe abdominal pain, persistent vomiting, dehydration, or jaundice, as these may indicate pancreatitis or gallbladder disease.
Table of Contents
Understanding Nausea with GLP-1 Receptor Agonists
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, for weight management in specific patient populations. These medications work by mimicking the action of the naturally occurring GLP-1 hormone, which stimulates insulin secretion, suppresses glucagon release, and slows gastric emptying. Whilst these mechanisms contribute to improved glycaemic control and weight reduction, they also account for one of the most commonly reported adverse effects: nausea.
Nausea associated with GLP-1 receptor agonists typically occurs because these medications delay the rate at which food leaves the stomach (gastric emptying). This physiological effect, whilst beneficial for reducing post-prandial glucose spikes and promoting satiety, can lead to feelings of fullness, bloating, and nausea—particularly during the initial weeks of treatment or following dose escalations. The severity and duration of nausea vary considerably between individuals and between different GLP-1 preparations.
Clinical studies indicate that nausea is generally most pronounced during treatment initiation and tends to diminish over time as the body adapts to the medication. However, for some patients, persistent nausea can significantly impact quality of life and treatment adherence. These medications should be used with caution in patients with significant gastrointestinal disease, such as gastroparesis, as noted in product SmPCs.
Importantly, patients should seek urgent medical attention if they experience severe or persistent abdominal pain (especially if radiating to the back), repeated vomiting, inability to keep fluids down, signs of dehydration, or jaundice, as these may indicate serious conditions such as pancreatitis or gallbladder disease. Understanding which GLP-1 formulations are associated with lower rates of nausea is essential for both healthcare professionals and patients when selecting the most appropriate treatment option.
Which GLP-1 Has Less Nausea: Comparing Options
Several GLP-1 receptor agonists are currently licensed in the UK, each with distinct pharmacological profiles that influence their tolerability. Semaglutide is available as once-weekly subcutaneous injection (Ozempic® for diabetes, with nausea rates of 16-20% depending on dose; and Wegovy® for weight management, with significantly higher nausea rates of approximately 44% in clinical trials), as well as oral formulation Rybelsus® (approximately 20% nausea incidence).
Dulaglutide (Trulicity®), another once-weekly injectable GLP-1 agonist, demonstrates a somewhat more favourable gastrointestinal tolerability profile in some studies, with nausea reported in approximately 8-12% of patients at lower doses, though rates increase with higher doses (3.0-4.5 mg). The SUSTAIN-7 trial directly compared dulaglutide with semaglutide, showing differences in gastrointestinal tolerability.
Liraglutide shows dose-dependent nausea rates—Victoza® (for diabetes) has rates around 10-17% depending on dose, while Saxenda® (3.0 mg for weight management) has significantly higher nausea rates of approximately 39% according to its SmPC.
Exenatide is available in both short-acting (twice-daily, Byetta®) and extended-release (once-weekly, Bydureon®) formulations. The twice-daily preparation has historically shown higher nausea rates of up to 30-40% of patients, while the extended-release formulation demonstrates improved tolerability.
Tirzepatide (Mounjaro®), a dual GIP/GLP-1 receptor agonist, shows dose-dependent nausea rates, ranging from approximately 12-18% at lower doses to higher rates at doses used for weight management, as demonstrated in the SURPASS-2 trial comparing it with semaglutide.
Current evidence suggests that dulaglutide and extended-release formulations generally demonstrate lower rates of nausea compared to twice-daily exenatide or higher doses of semaglutide and liraglutide used for weight management, though individual responses vary considerably.
Why Some GLP-1 Medications Cause Less Nausea
The variation in nausea rates between different GLP-1 receptor agonists relates to several pharmacological and formulation factors. Dosing frequency and titration schedules play a crucial role: medications that allow for gradual dose escalation over several weeks enable the gastrointestinal system to adapt more effectively to the delayed gastric emptying effect. Once-weekly formulations typically provide more stable plasma concentrations with lower peak levels compared to shorter-acting preparations, potentially reducing the intensity of gastrointestinal side effects.
Receptor binding affinity and selectivity may also influence tolerability, though this relationship is not firmly established. GLP-1 receptor agonists differ in their structural similarity to native human GLP-1, with some being modified peptides and others being exendin-4 analogues. These structural differences may affect how they interact with GLP-1 receptors in the gastrointestinal tract and central nervous system, which could contribute to differences in nausea experienced. It's worth noting that some long-acting GLP-1 agonists (such as semaglutide at higher doses) can still cause significant nausea despite their extended half-life.
The rate of gastric emptying delay varies between different GLP-1 agonists. Whilst all medications in this class slow gastric emptying to some degree, the magnitude and duration of this effect differ. Preparations that cause more moderate, sustained slowing rather than pronounced acute effects may be better tolerated. Additionally, individual patient factors—including baseline gastric motility, previous gastrointestinal conditions, concomitant medications, and genetic variations in drug metabolism—significantly influence susceptibility to nausea. There is no official link established between specific genetic markers and GLP-1-induced nausea, though research in pharmacogenomics continues to evolve. Understanding these mechanisms helps clinicians select the most appropriate GLP-1 agonist for individual patients and set realistic expectations regarding tolerability.
How to Reduce Nausea When Taking GLP-1 Medications
Practical strategies can significantly reduce nausea associated with GLP-1 receptor agonist therapy, improving treatment adherence and patient outcomes. The most important approach is gradual dose titration: starting with the lowest available dose and increasing slowly according to the manufacturer's recommended schedule allows the gastrointestinal system time to adapt. Patients should never accelerate dose escalation without medical supervision, even if initial tolerance seems good.
Dietary modifications can substantially alleviate nausea. Patients should be advised to:
-
Eat smaller, more frequent meals rather than large portions
-
Avoid high-fat, greasy, or heavily spiced foods that delay gastric emptying further
-
Stay well hydrated with small, frequent sips of water throughout the day
-
Avoid lying down immediately after eating; remaining upright for 2–3 hours post-meal can help
-
Identify and avoid personal trigger foods that worsen symptoms
Timing of medication administration may also help: some patients find that taking their injectable GLP-1 medication before bedtime (where applicable) means sleeping through the peak nausea period. However, it's important to note that oral semaglutide (Rybelsus®) must be taken on waking, in a fasting state, with a small amount of water, and at least 30 minutes before food, drink or other medications, as per its SmPC.
When to seek medical advice: Patients should contact their healthcare provider if nausea is severe, persistent beyond the first few weeks, or accompanied by repeated vomiting. Urgent medical attention is required for severe or persistent abdominal pain (especially if radiating to the back), persistent vomiting preventing adequate fluid intake, signs of dehydration, blood in vomit, black stools, or jaundice, as these may indicate serious conditions such as pancreatitis or gallbladder disease.
In some cases, temporary dose reduction, switching to an alternative GLP-1 preparation, or clinician-supervised, short-term anti-emetic medication may be appropriate. Patients should never discontinue GLP-1 therapy abruptly without medical consultation. Any suspected adverse reactions should be reported through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Which GLP-1 medication causes the least nausea?
Current evidence suggests dulaglutide (Trulicity) and extended-release exenatide (Bydureon) generally demonstrate lower nausea rates (approximately 8-12% at lower doses) compared to twice-daily exenatide or higher-dose semaglutide and liraglutide used for weight management. However, individual responses vary considerably, and gradual dose titration is essential for all GLP-1 preparations.
How long does nausea from GLP-1 medications typically last?
Nausea associated with GLP-1 receptor agonists is generally most pronounced during treatment initiation and following dose escalations, typically diminishing over the first few weeks as the body adapts. If nausea persists beyond this period or is severe, patients should contact their healthcare provider for assessment and potential dose adjustment.
What can I do to reduce nausea when taking GLP-1 medications?
To reduce nausea, follow gradual dose titration schedules, eat smaller frequent meals, avoid high-fat and greasy foods, stay well hydrated, and remain upright for 2-3 hours after eating. If nausea is severe or accompanied by persistent vomiting, abdominal pain, or signs of dehydration, seek medical advice promptly as these may indicate serious complications.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












