GLP-1 receptor agonist fatigue management strategies are essential for patients experiencing tiredness whilst taking medications such as semaglutide, dulaglutide, or liraglutide. Fatigue is a recognised adverse reaction with these diabetes and weight management treatments, though its severity and duration vary considerably between individuals. Effective management involves optimising nutrition despite reduced appetite, maintaining hydration, addressing gastrointestinal symptoms, and implementing lifestyle modifications to support energy levels. Understanding when fatigue warrants medical evaluation is crucial, as persistent tiredness may indicate underlying conditions requiring investigation. This article explores evidence-based approaches to managing fatigue during GLP-1 therapy whilst ensuring safe, effective treatment outcomes.
Summary: GLP-1 receptor agonist fatigue management strategies include optimising nutrient-dense food intake, maintaining proper hydration, gradual dose titration, managing gastrointestinal symptoms, regular physical activity, and seeking medical review for persistent or severe tiredness.
- Fatigue is a recognised adverse reaction with GLP-1 receptor agonists including semaglutide, dulaglutide, and liraglutide, though mechanisms are not fully established.
- Reduced caloric intake, gastrointestinal symptoms, and metabolic adjustments may contribute to tiredness during treatment.
- Consuming nutrient-dense foods with adequate protein, maintaining hydration (1.2–1.5 litres daily), and gradual dose titration help minimise fatigue.
- Persistent or worsening fatigue, hypoglycaemia symptoms, severe gastrointestinal effects, or signs of pancreatitis require prompt medical evaluation.
- Blood tests may be arranged to exclude anaemia, thyroid dysfunction, vitamin deficiencies, or other underlying causes of tiredness.
Table of Contents
Understanding Fatigue with GLP-1 Receptor Agonists
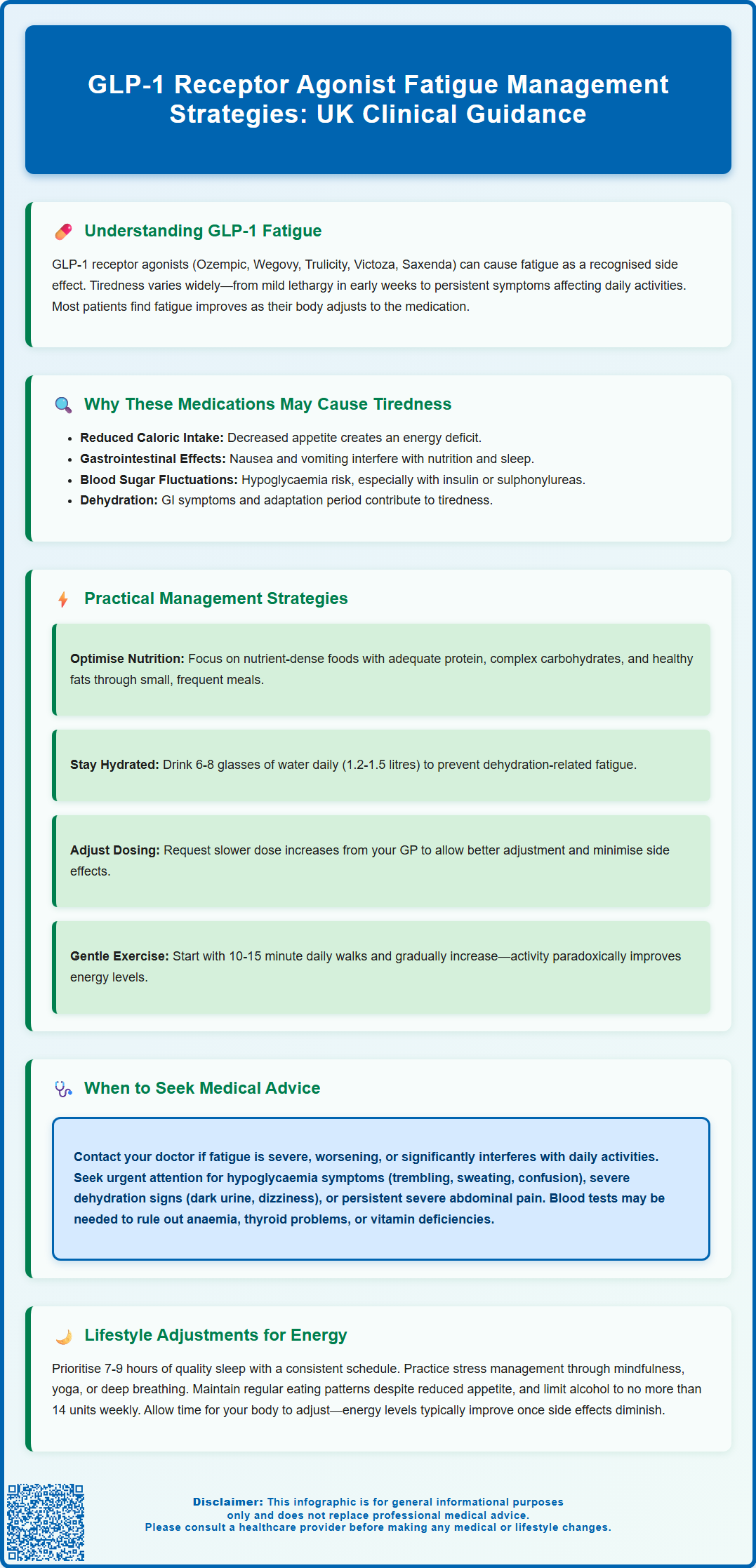
GLP-1 receptor agonists are a class of medications increasingly prescribed for type 2 diabetes management and, more recently, for weight management. These medicines include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and exenatide (Byetta, Bydureon). Whilst these medications offer significant benefits in glycaemic control and weight reduction, some patients report experiencing fatigue or tiredness during treatment.
Fatigue or asthenia is recognised as a common adverse reaction for some GLP-1 receptor agonists, as documented in their Summary of Product Characteristics (SmPCs). The frequency varies between different products and indications. The experience of tiredness can vary considerably between individuals—some may notice mild lethargy during the initial weeks of treatment, whilst others may experience more persistent symptoms that affect daily functioning.
It is important to recognise that fatigue is a non-specific symptom with multiple potential causes. When fatigue occurs in patients taking GLP-1 receptor agonists, it may be directly related to the medication, secondary to the physiological changes these drugs induce (such as reduced caloric intake or altered glucose metabolism), or entirely unrelated to the treatment. Understanding the potential mechanisms and distinguishing between medication-related tiredness and other causes is essential for appropriate management.
Patients should be reassured that fatigue, when it does occur, often improves with time as the body adjusts to the medication. However, persistent or severe tiredness warrants clinical evaluation to exclude other underlying conditions and to optimise treatment strategies.
Why GLP-1 Medications May Cause Tiredness
Fatigue or asthenia is listed as an adverse reaction in the SmPCs for several GLP-1 receptor agonists, though the precise mechanisms remain not fully established. Several physiological factors may potentially contribute to tiredness in patients taking these medications.
Reduced caloric intake is one hypothesis. GLP-1 receptor agonists work by mimicking the naturally occurring hormone glucagon-like peptide-1, which slows gastric emptying, increases satiety, and reduces appetite. This often leads to a significant decrease in food consumption. Whilst beneficial for weight loss and glycaemic control, a substantial caloric deficit—particularly if nutritional intake becomes inadequate—may contribute to fatigue and reduced energy levels.
Gastrointestinal adverse effects are among the most commonly reported side effects of GLP-1 therapy, including nausea, vomiting, diarrhoea, and constipation. These symptoms can interfere with adequate nutrition and hydration, potentially contributing to feelings of tiredness. Persistent nausea may also disrupt sleep patterns and overall wellbeing.
Additionally, changes in blood glucose levels may play a role. Whilst GLP-1 receptor agonists themselves have a low risk of causing hypoglycaemia when used alone, this risk increases when combined with insulin or sulphonylureas. Hypoglycaemia (low blood sugar) can manifest as fatigue, dizziness, and weakness. Conversely, the body's adjustment to improved glucose regulation after periods of hyperglycaemia may temporarily affect energy levels.
Other potential contributing factors include dehydration (especially if gastrointestinal symptoms are present) and the body's adaptation period to the medication. It is worth noting that fatigue may also be coincidental and unrelated to GLP-1 therapy, arising from underlying conditions such as anaemia, thyroid dysfunction, depression, or sleep disorders.
Practical Strategies to Manage Fatigue on GLP-1 Therapy
Managing fatigue whilst taking GLP-1 receptor agonists requires a multifaceted approach that addresses both medication-related factors and general health optimisation. The following strategies can help patients maintain energy levels during treatment.
Optimising nutritional intake is paramount. Despite reduced appetite, patients should focus on consuming nutrient-dense foods that provide adequate protein, complex carbohydrates, healthy fats, vitamins, and minerals. Small, frequent meals may be better tolerated than larger portions, particularly if nausea is present. Adequate protein intake is important to help preserve muscle mass during weight loss and support energy production. The exact amount should be individualised, particularly for those with kidney disease, and a registered dietitian can provide personalised advice. Including iron-rich foods, B vitamins, and ensuring adequate vitamin D levels can also combat fatigue.
Maintaining proper hydration is essential, particularly if gastrointestinal symptoms are present. The NHS recommends 6-8 drinks daily (approximately 1.2-1.5 litres), with increased intake during hot weather, exercise, or illness. Dehydration can significantly worsen fatigue and may also exacerbate constipation, a common side effect of GLP-1 medications.
Gradual dose titration can minimise side effects. Healthcare professionals typically initiate GLP-1 therapy at a low dose and increase gradually over several weeks. If fatigue is problematic, discussing a slower titration schedule with your prescriber may allow better tolerance whilst the body adjusts.
Timing of medication administration should follow the specific instructions for your prescribed GLP-1 product. Always adhere to the administration guidance in the patient information leaflet or as directed by your healthcare professional. For example, oral semaglutide (Rybelsus) must be taken in the morning on an empty stomach.
Managing gastrointestinal symptoms proactively can improve overall wellbeing and energy. Simple dietary modifications (avoiding fatty, spicy, or very sweet foods) can reduce gastrointestinal discomfort. For persistent nausea, consult your GP or pharmacist before using anti-emetic medications. For constipation, increasing fibre, fluids, and physical activity may help; if persistent, discuss with your healthcare provider about suitable laxatives such as macrogol.
Regular physical activity, even when feeling tired, can paradoxically improve energy levels. Starting with gentle activities such as walking for 10–15 minutes daily and gradually increasing intensity can enhance cardiovascular fitness, improve mood, and reduce fatigue. Exercise also helps maintain muscle mass during weight loss.
When to Seek Medical Advice About Persistent Tiredness
Whilst mild fatigue during the initial weeks of GLP-1 therapy may be expected as the body adjusts, certain situations warrant prompt medical evaluation. Patients should contact their GP or prescribing clinician if they experience any of the following:
Severe or worsening fatigue that significantly impairs daily activities, work performance, or quality of life should be assessed. Fatigue that progressively worsens rather than improving over time may indicate an underlying issue requiring investigation.
Symptoms suggesting hypoglycaemia require urgent attention, particularly in patients taking GLP-1 receptor agonists alongside insulin or sulphonylureas. Warning signs include trembling, sweating, confusion, palpitations, dizziness, or extreme tiredness. If you experience hypoglycaemia, take a fast-acting carbohydrate (such as glucose tablets or fruit juice), recheck your blood glucose after 15 minutes, and discuss with your healthcare provider about possible adjustment of insulin or sulphonylurea doses.
Signs of dehydration or electrolyte imbalance should prompt medical review. These include persistent dizziness, reduced urine output, dark-coloured urine, muscle cramps, or confusion. Severe gastrointestinal symptoms causing inability to maintain adequate fluid intake require assessment, as there is a risk of acute kidney injury with significant dehydration.
Symptoms of acute pancreatitis or gallbladder disease require urgent medical attention. These include severe, persistent abdominal pain (which may radiate to the back), with or without vomiting for pancreatitis, or pain in the right upper abdomen, fever, or yellowing of the skin/eyes for gallbladder problems. These are known potential complications of GLP-1 therapy.
Symptoms suggesting other medical conditions warrant investigation. These include unexplained weight loss beyond expected therapeutic effects, persistent fever, night sweats, shortness of breath, chest pain, palpitations, or changes in mood such as low mood or anxiety. Fatigue accompanied by pallor, easy bruising, or unusual bleeding may indicate anaemia or other haematological conditions.
New or worsening depression should be addressed, as fatigue is a common symptom of mood disorders. Mental health concerns require appropriate evaluation and support.
Your healthcare provider may arrange blood tests to exclude other causes of fatigue, including full blood count (to check for anaemia), thyroid function tests, vitamin B12 and folate levels, vitamin D status, renal and liver function, and HbA1c to assess diabetes control. Based on findings, medication adjustments, nutritional supplementation, or referral to specialist services may be recommended.
Call 999 for severe chest pain, severe persistent abdominal pain, or collapse. Use NHS 111 for urgent advice when your GP is unavailable.
Lifestyle Adjustments to Support Energy Levels
Beyond medication-specific strategies, comprehensive lifestyle modifications can significantly improve energy levels and overall wellbeing during GLP-1 therapy. These approaches support the body's adaptation to treatment and promote optimal health outcomes.
Sleep hygiene is fundamental to managing fatigue. Adults should aim for 7–9 hours of quality sleep nightly. Establishing a consistent sleep schedule, creating a comfortable sleep environment (cool, dark, and quiet), limiting screen time before bed, and avoiding caffeine in the late afternoon can improve sleep quality. If sleep disturbances persist, discussing this with a healthcare professional is important, as sleep disorders such as sleep apnoea may require specific treatment. The NHS website offers helpful resources on improving sleep.
Stress management plays a crucial role in energy levels. Chronic stress contributes to fatigue and can be addressed through various techniques including mindfulness meditation, deep breathing exercises, yoga, or cognitive behavioural approaches. The NHS offers resources and referrals for psychological support when needed.
Balanced meal planning should focus on regular eating patterns despite reduced appetite. Skipping meals can worsen fatigue and may lead to nutritional deficiencies. Working with a registered dietitian can help develop a personalised eating plan that meets nutritional needs whilst accommodating reduced appetite and any gastrointestinal symptoms. The British Dietetic Association provides resources for finding qualified professionals.
Limiting alcohol consumption is advisable, as alcohol can interfere with sleep quality, contribute to dehydration, affect blood glucose levels, and worsen fatigue. UK Chief Medical Officers recommend no more than 14 units weekly, spread over several days, with some alcohol-free days each week.
Monitoring blood glucose levels (where appropriate) helps identify patterns that may contribute to fatigue. Patients with diabetes should follow their individualised monitoring plan and report any concerning trends to their healthcare team.
Social connection and support should not be underestimated. Engaging with family, friends, or support groups (including online communities for patients on GLP-1 therapy) can provide emotional support, practical advice, and motivation. Isolation can worsen fatigue and mood.
Finally, patience and realistic expectations are important. The body often requires time to adjust to GLP-1 therapy, and energy levels typically improve as side effects diminish and the body adapts to metabolic changes. Maintaining open communication with healthcare providers ensures that any concerns are addressed promptly and that treatment remains optimised for individual needs.
If you suspect your fatigue is related to your medication, you can report this as a suspected side effect through the MHRA Yellow Card Scheme, which helps monitor the safety of medicines in the UK.
Frequently Asked Questions
Why do GLP-1 receptor agonists cause fatigue?
GLP-1 receptor agonists may cause fatigue through reduced caloric intake, gastrointestinal symptoms affecting nutrition and hydration, changes in blood glucose regulation, and the body's adaptation period to the medication. The precise mechanisms are not fully established and fatigue may also be unrelated to the medication.
How long does fatigue last when taking GLP-1 medications?
Fatigue often improves within the first few weeks as the body adjusts to GLP-1 therapy. However, duration varies between individuals, and persistent or worsening tiredness warrants medical evaluation to exclude other underlying conditions.
When should I contact my GP about fatigue on GLP-1 treatment?
Contact your GP if you experience severe or worsening fatigue impairing daily activities, symptoms of hypoglycaemia (especially if taking insulin or sulphonylureas), signs of dehydration, severe abdominal pain, or fatigue accompanied by other concerning symptoms such as unexplained weight loss, fever, or mood changes.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript