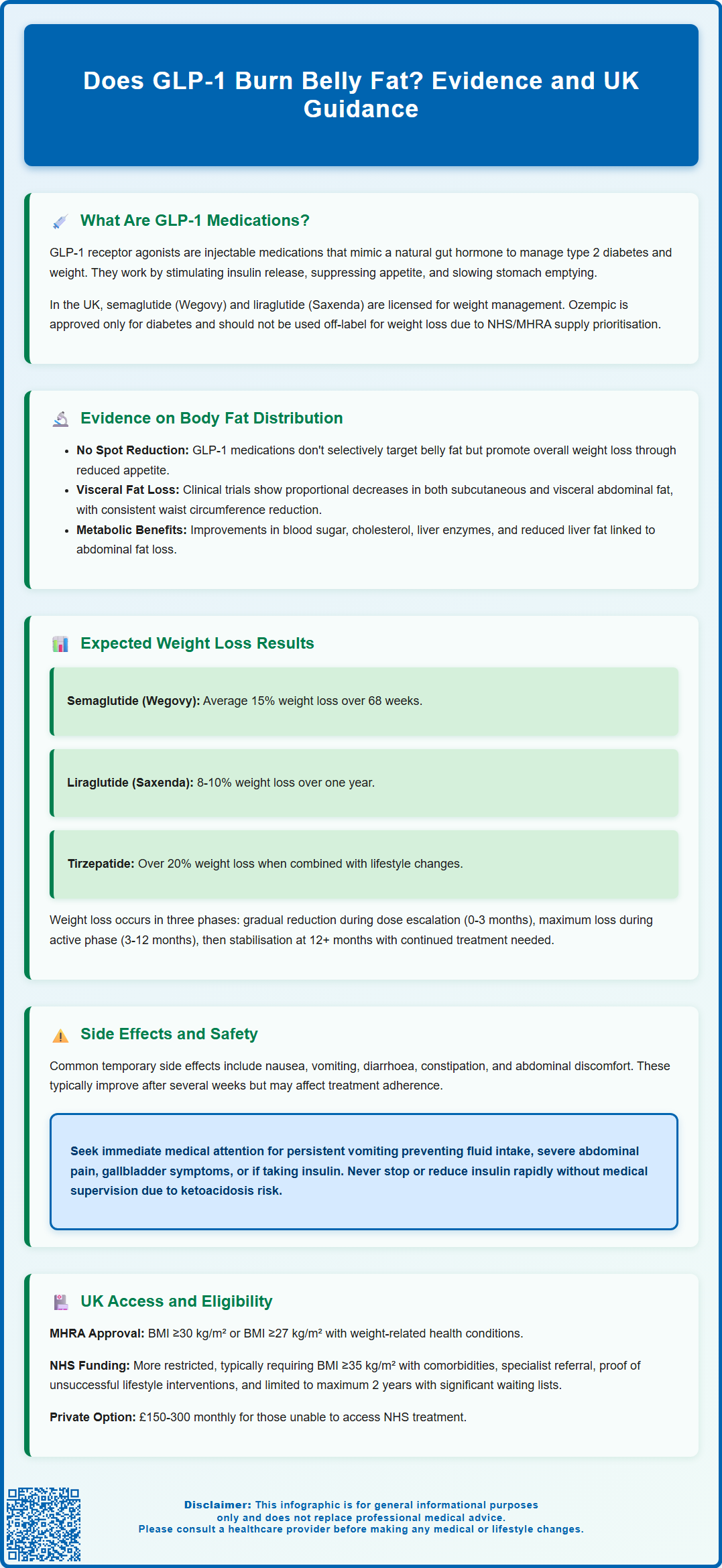
GLP-1 receptor agonists have gained considerable attention for their role in weight management, prompting questions about their effects on abdominal fat. Whilst these medications do not selectively 'burn' belly fat through direct mechanisms, clinical evidence demonstrates they promote significant overall weight loss, including reductions in visceral adipose tissue—the metabolically harmful fat surrounding internal organs. Understanding how GLP-1 medications work, what realistic outcomes to expect, and who may be suitable for treatment is essential for informed decision-making. This article examines the evidence on GLP-1 medications and body fat distribution, drawing on UK clinical guidance and regulatory frameworks.
Summary: GLP-1 medications do not selectively burn belly fat but promote generalised weight loss that includes significant reductions in visceral abdominal fat.
- GLP-1 receptor agonists reduce appetite and slow gastric emptying, creating a caloric deficit that leads to fat mobilisation throughout the body.
- Clinical trials demonstrate reductions in waist circumference and visceral adipose tissue alongside overall weight loss of 8–20% depending on the specific medication.
- These medications work through appetite suppression rather than direct fat-burning mechanisms such as thermogenesis or lipolysis.
- NHS access requires BMI ≥35 kg/m² with weight-related comorbidities, specialist referral, and prior engagement with lifestyle interventions.
- Common side effects include nausea, gastrointestinal disturbance, and injection site reactions; regular monitoring is essential throughout treatment.
- Medications are contraindicated in pregnancy and require careful assessment for interactions, particularly with insulin or in patients with severe gastrointestinal disease.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management but now also licensed for weight management. These injectable medicines mimic the action of naturally occurring GLP-1, a hormone produced in the intestine following food intake.
The mechanism of action involves several physiological pathways. GLP-1 medications bind to GLP-1 receptors in the pancreas, stimulating insulin secretion when blood glucose levels are elevated whilst simultaneously suppressing glucagon release. Crucially for weight management, these drugs act on receptors in the brain—particularly in the hypothalamus and brainstem—to reduce appetite and increase feelings of satiety. They also slow gastric emptying, meaning food remains in the stomach longer, contributing to prolonged fullness after meals, though this effect may attenuate over time.
Currently available GLP-1 medications in the UK include:
-
Semaglutide (Ozempic for diabetes only; Wegovy specifically licensed for weight management)
-
Liraglutide (Victoza for diabetes only; Saxenda specifically licensed for weight management)
-
Dulaglutide (Trulicity, licensed only for diabetes, not weight management)
-
Tirzepatide (Mounjaro), a dual GLP-1 and GIP receptor agonist licensed for type 2 diabetes
These medications are administered via subcutaneous injection, typically weekly or daily depending on the specific formulation. It's important to note that Ozempic (semaglutide 0.25-1mg) should not be used off-label for weight loss, particularly given NHS/MHRA supply prioritisation for people with diabetes.
The delayed gastric emptying effect may reduce the absorption of some oral medicines. Patients should consult their healthcare provider or refer to the medicine's patient information leaflet for specific guidance on managing potential interactions.
Evidence on GLP-1 and Body Fat Distribution
The question of whether GLP-1 medications specifically 'burn' belly fat requires careful consideration of the available evidence. GLP-1 drugs do not selectively target abdominal fat through direct fat-burning mechanisms; rather, they promote generalised weight loss through reduced energy intake and metabolic changes. However, clinical studies have demonstrated that the weight lost with GLP-1 treatment includes significant reductions in visceral adipose tissue—the metabolically active fat surrounding internal organs in the abdominal cavity.
Clinical trials using imaging techniques such as MRI and CT scans have shown that GLP-1 receptor agonists lead to reductions in both subcutaneous fat (beneath the skin) and visceral fat. Research from the STEP programme (semaglutide), SCALE studies (liraglutide), and SURMOUNT trials (tirzepatide) consistently demonstrates significant reductions in waist circumference, which correlates with abdominal fat loss. These studies suggest that visceral fat may decrease proportionally during GLP-1-induced weight loss, similar to patterns seen with dietary caloric restriction.
Key findings from clinical trials include:
-
Reductions in waist circumference, an indirect marker of abdominal fat
-
Improvements in metabolic markers associated with visceral adiposity (HbA1c, lipid profiles, liver enzymes)
-
Decreased hepatic fat content in patients with fatty liver disease
It is important to understand that GLP-1 medications do not 'burn' fat through thermogenesis or direct lipolysis. Instead, they create a sustained caloric deficit by reducing appetite and food intake, leading to mobilisation of fat stores throughout the body. The apparent benefit for abdominal fat reflects the body's natural pattern of fat loss during caloric restriction, where visceral fat often responds favourably to weight reduction interventions.
What to Expect: Weight Loss Results with GLP-1
Weight loss outcomes with GLP-1 medications vary considerably depending on the specific agent used, dosage, treatment duration, and individual patient factors. Clinical trial data provides useful benchmarks, though real-world results may differ.
In the STEP clinical trials, semaglutide 2.4 mg (Wegovy) demonstrated average weight loss of approximately 15% of initial body weight over 68 weeks when combined with lifestyle interventions. The SCALE programme showed liraglutide 3.0 mg (Saxenda) typically produces weight loss of around 8-10% over one year. In the SURMOUNT-1 trial, tirzepatide demonstrated even more substantial results, with some participants losing over 20% of their starting weight.
Weight loss typically follows a predictable pattern:
-
Initial phase (0-3 months): Gradual dose escalation with modest weight reduction as appetite suppression begins
-
Active loss phase (3-12 months): Most significant weight reduction occurs during this period
-
Plateau phase (12+ months): Weight stabilises; continued treatment helps maintain losses
Common side effects that may affect treatment adherence include:
-
Nausea and vomiting (usually temporary, improving after several weeks)
-
Diarrhoea or constipation
-
Abdominal discomfort
-
Fatigue
-
Injection site reactions
Important safety considerations include:
-
Risk of hypoglycaemia if used with insulin or sulfonylureas
-
Do not stop or reduce insulin rapidly without medical advice (risk of diabetic ketoacidosis)
-
Maintain adequate hydration to prevent acute kidney injury
-
Potential for gallbladder problems (pain, stones)
-
Rare risk of intestinal obstruction
-
Possible worsening of diabetic retinopathy in people with diabetes during rapid improvement in blood glucose
-
For tirzepatide: use additional non-oral contraception for 4 weeks after initiation and each dose escalation
Patients should contact their GP if they experience: persistent vomiting preventing fluid intake, severe abdominal pain, signs of gallbladder disease, or unusual thyroid symptoms. Regular monitoring is essential throughout treatment.
If you experience any side effects, talk to your healthcare professional. This includes any possible side effects not listed in the package leaflet. You can also report side effects directly via the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Who Can Access GLP-1 Treatment in the UK?
Access to GLP-1 medications for weight management in the UK involves understanding both licensing (what the medicines are approved for) and NHS commissioning (who can receive them on the NHS).
Licensing (Marketing Authorisation): The MHRA has approved:
-
Semaglutide (Wegovy) for adults with BMI ≥30 kg/m² or BMI ≥27 kg/m² with at least one weight-related comorbidity
-
Liraglutide (Saxenda) with similar BMI criteria
NHS Access (NICE Guidance): According to NICE guidance (TA664 for semaglutide), NHS-funded treatment is more restricted and typically available for adults with:
- BMI ≥35 kg/m² with at least one weight-related comorbidity (such as hypertension, type 2 diabetes, dyslipidaemia, obstructive sleep apnoea, or cardiovascular disease)
For individuals from Black, Asian, and minority ethnic backgrounds, lower BMI thresholds may apply, recognising that these populations face increased metabolic risk at lower BMI levels.
NICE recommends treatment only within specialist weight management services, typically for a maximum of 2 years, and only if non-surgical weight management interventions have been unsuccessful.
Current NHS availability is limited. Due to high demand, global supply constraints, and budgetary considerations, access through NHS prescription remains restricted. Many specialist weight management services have waiting lists or strict prioritisation criteria. The NHS England pathway typically requires:
-
Referral to a specialist weight management service
-
Demonstrated engagement with dietary and lifestyle interventions
-
Assessment of suitability and precautions
-
Regular monitoring and review
Private prescription is an alternative route, though costs are substantial—typically £150-300 monthly depending on the medication and dose. Patients considering private treatment should ensure proper medical assessment, monitoring, and follow-up care.
Important precautions: These medicines are contraindicated in pregnancy. They are not recommended during breast-feeding. Caution is needed in people with severe gastrointestinal disease (e.g., gastroparesis). Patients should discuss any thyroid symptoms with their healthcare provider (as a precaution based on animal studies). A full medical assessment is essential before starting treatment.
Scientific References
Frequently Asked Questions
Can GLP-1 medications specifically target belly fat?
GLP-1 medications do not selectively target abdominal fat but promote generalised weight loss through appetite suppression and reduced caloric intake. Clinical studies show that this weight loss includes significant reductions in visceral fat, the metabolically active fat surrounding internal organs.
How much weight can I expect to lose with GLP-1 treatment?
Weight loss varies by medication and individual factors. Clinical trials show semaglutide (Wegovy) produces average weight loss of approximately 15% over 68 weeks, liraglutide (Saxenda) around 8–10% over one year, and tirzepatide over 20% in some participants, all combined with lifestyle interventions.
Who can access GLP-1 medications for weight loss on the NHS?
NHS access typically requires BMI ≥35 kg/m² with at least one weight-related comorbidity, referral to a specialist weight management service, and demonstrated engagement with dietary and lifestyle interventions. Current availability is limited due to supply constraints and budgetary considerations.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript