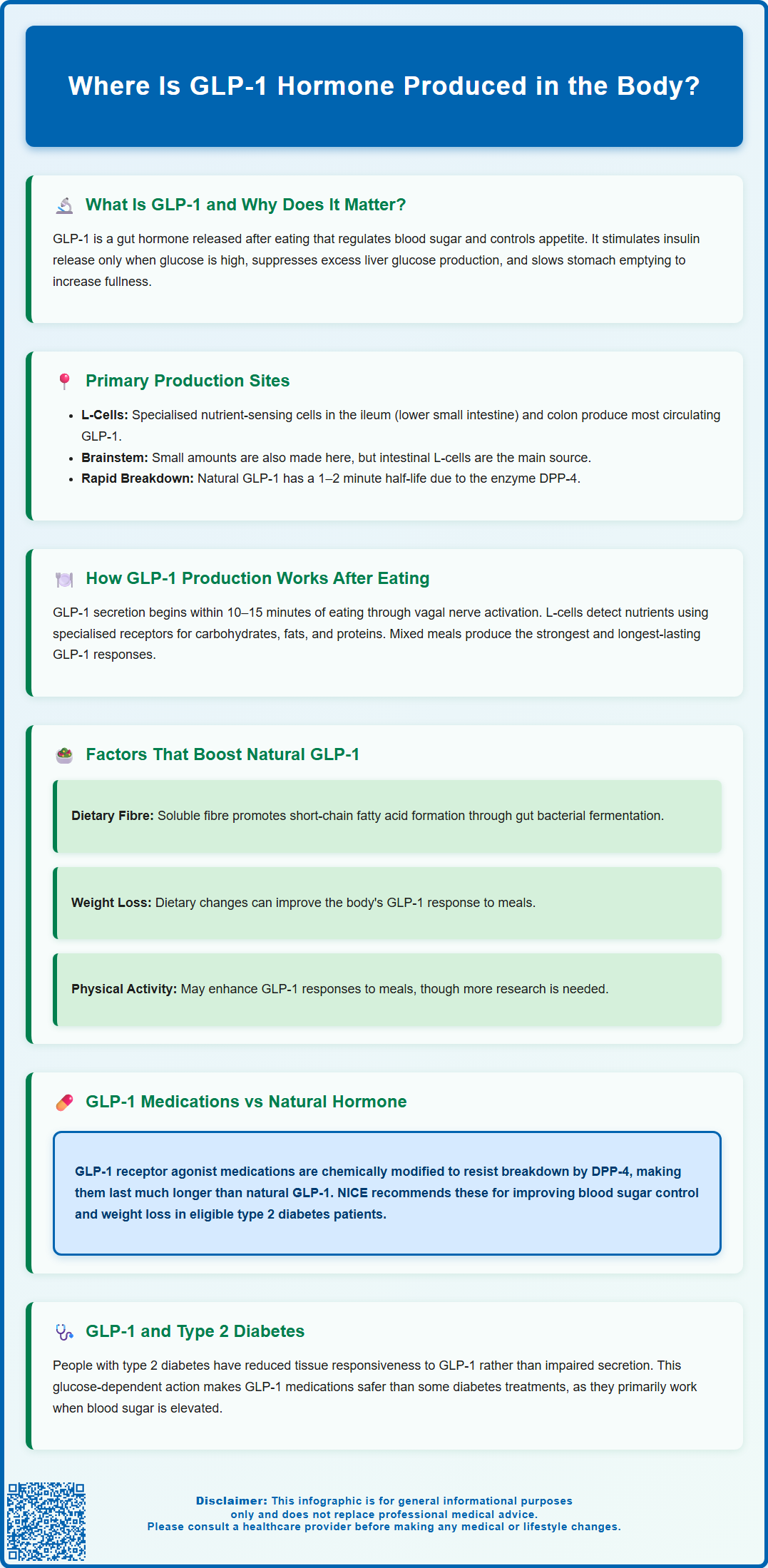
Glucagon-like peptide-1 (GLP-1) is a naturally occurring hormone that plays a vital role in blood glucose regulation and appetite control. Understanding where GLP-1 is produced helps explain how the body maintains metabolic balance and why GLP-1-based medications have become important therapeutic options. GLP-1 is primarily produced by specialised L-cells in the intestine, which release the hormone in response to food intake. This article explores the sites of GLP-1 production, the mechanisms involved, and factors that influence its secretion, providing insight into both normal physiology and the rationale behind GLP-1 receptor agonist therapies used in type 2 diabetes and weight management.
Summary: GLP-1 hormone is primarily produced by specialised L-cells located in the distal small intestine (ileum) and colon, with the highest concentrations in the ileum and large intestine.
- GLP-1 is an incretin hormone that enhances glucose-dependent insulin secretion and suppresses glucagon release from the pancreas.
- L-cells are enteroendocrine cells that function as nutrient sensors, detecting glucose, fatty acids, and amino acids in the intestinal lumen.
- GLP-1 has a very short half-life of 1–2 minutes due to rapid degradation by the enzyme dipeptidyl peptidase-4 (DPP-4).
- Dietary composition, particularly carbohydrates, fats, proteins, and fibre, significantly influences GLP-1 secretion from intestinal L-cells.
- GLP-1 receptor agonists are used in accordance with NICE guidance for managing type 2 diabetes (NG28) and, in defined circumstances, for weight management (TA875).
Table of Contents
What Is GLP-1 and Why Is It Important?
Glucagon-like peptide-1 (GLP-1) is a naturally occurring incretin hormone that plays a crucial role in regulating blood glucose levels and appetite. This peptide hormone belongs to a family of gut-derived hormones that are released in response to food intake, particularly nutrients such as carbohydrates and fats. GLP-1 acts as a key metabolic regulator, coordinating multiple physiological processes to maintain glucose homeostasis.
The primary importance of GLP-1 lies in its ability to enhance insulin secretion from pancreatic beta cells in a glucose-dependent manner. This means that GLP-1 stimulates insulin release only when blood glucose levels are elevated, which significantly reduces (though does not eliminate) the risk of hypoglycaemia. Additionally, GLP-1 suppresses glucagon secretion from pancreatic alpha cells, which helps prevent excessive glucose production by the liver. These complementary actions make GLP-1 essential for maintaining stable blood sugar levels throughout the day.
Beyond glucose regulation, GLP-1 exerts important effects on appetite and satiety. The hormone slows gastric emptying, prolonging the feeling of fullness after meals, and acts on appetite centres in the brain to reduce food intake. These properties have made GLP-1 receptor agonists valuable therapeutic agents for managing type 2 diabetes and obesity. GLP-1 receptor agonists are used in line with NICE guidance for certain people with type 2 diabetes (NICE NG28) and, in defined circumstances, for weight management (NICE TA875). Understanding where and how GLP-1 is produced provides insight into both normal metabolic function and the rationale behind GLP-1-based medications.
Where Is GLP-1 Hormone Produced in the Body?
GLP-1 is primarily produced by specialised cells called L-cells, which are enteroendocrine cells located predominantly in the distal small intestine (ileum) and colon. These L-cells are scattered throughout the intestinal epithelium, forming part of the gut's endocrine system. The highest concentration of L-cells is found in the ileum and large intestine, though smaller numbers are present in the duodenum and jejunum. This distribution pattern is physiologically significant, as it allows the gut to sense nutrients at various stages of digestion.
L-cells function as nutrient sensors, detecting the presence of food components in the intestinal lumen and responding by secreting GLP-1 into the bloodstream. These cells possess various receptors and transporters on their surface that recognise specific nutrients, particularly glucose, fatty acids, and amino acids. When activated, L-cells release GLP-1 along with other hormones such as peptide YY (PYY) and oxyntomodulin, which collectively contribute to metabolic regulation and satiety signalling.
Interestingly, small amounts of GLP-1 are also produced in the central nervous system, specifically in the nucleus tractus solitarius of the brainstem. However, the vast majority of circulating GLP-1 originates from intestinal L-cells. Once secreted, GLP-1 has a very short half-life of approximately 1-2 minutes in the circulation, as it is rapidly degraded by the enzyme dipeptidyl peptidase-4 (DPP-4). This rapid breakdown explains why therapeutic GLP-1 receptor agonists have been chemically modified to resist DPP-4 degradation, thereby extending their duration of action and clinical efficacy in managing diabetes and obesity.
Factors That Affect Natural GLP-1 Production
Several physiological and lifestyle factors influence the body's natural production of GLP-1, with significant implications for metabolic health. Dietary composition is perhaps the most important determinant of GLP-1 secretion. Meals rich in carbohydrates, fats, and proteins all stimulate GLP-1 release, though the magnitude and timing of secretion vary depending on the specific nutrients consumed. Dietary fibre, particularly soluble fibre, appears to enhance GLP-1 production by promoting the formation of short-chain fatty acids through bacterial fermentation in the colon, which may then stimulate L-cells.
Body weight and metabolic status also affect GLP-1 production. Research suggests that some individuals with obesity may have altered GLP-1 responses, though findings are heterogeneous. Conversely, weight loss through dietary intervention may improve GLP-1 responses to meals. In type 2 diabetes, the incretin effect is reduced; GLP-1 secretion is often preserved, but tissue responsiveness to GLP-1 may be diminished. This partly explains why pharmacological GLP-1 receptor agonists can still be effective in this population.
Gut microbiota composition has emerged as a potential modulator of GLP-1 production, though human evidence remains limited. The bacteria residing in the intestine may influence L-cell function through various mechanisms, including the production of metabolites that could affect GLP-1 secretion. Additionally, some evidence suggests that physical activity might enhance GLP-1 responses to meals, though the mechanisms and consistency of this effect require further investigation. Age-related changes in gut function may also influence GLP-1 production, though there is no definitive consensus on this relationship. Understanding these factors helps explain individual variation in metabolic health and may inform lifestyle approaches to support metabolic function.
How GLP-1 Production Works After Eating
The process of GLP-1 production following food intake involves a sophisticated cascade of nutrient sensing and hormonal signalling. When food enters the digestive tract, it undergoes mechanical and enzymatic breakdown, releasing nutrients that interact with L-cells at various points along the intestinal tract. The initial phase of GLP-1 secretion occurs rapidly, within 10–15 minutes of eating, even before nutrients reach the distal intestine where most L-cells reside. This early response involves proximal small-intestinal L-cells alongside neural and hormonal signals, including vagal nerve activation and the release of gastric hormones.
As digestion progresses and nutrients move through the small intestine, direct contact between nutrients and L-cells triggers the main phase of GLP-1 secretion. L-cells express numerous receptors that detect specific nutrients: glucose transporters (such as SGLT1) sense carbohydrates, G-protein coupled receptors detect fatty acids, and amino acid transporters recognise proteins. When these receptors are activated, they initiate intracellular signalling pathways that lead to the release of stored GLP-1 from secretory granules within the L-cells. The hormone then enters the bloodstream through nearby capillaries.
The magnitude and duration of GLP-1 secretion depend on the meal's composition, size, and rate of gastric emptying. Mixed meals containing carbohydrates, fats, and proteins typically produce robust and sustained GLP-1 responses. Once in circulation, GLP-1 travels to target tissues, including the pancreas, where it enhances insulin secretion, and the brain, where it promotes satiety. However, the enzyme DPP-4 rapidly degrades circulating GLP-1, limiting its duration of action. Long-acting GLP-1 receptor agonists provide sustained receptor activation and clinically meaningful improvements in glycaemic control and weight in eligible patients, as recognised in NICE guidance (NG28) for type 2 diabetes management.
Frequently Asked Questions
Which cells produce GLP-1 in the intestine?
GLP-1 is produced by specialised enteroendocrine cells called L-cells, which are located predominantly in the distal small intestine (ileum) and colon. These cells function as nutrient sensors and release GLP-1 in response to food intake.
Why does GLP-1 have such a short duration in the body?
Natural GLP-1 has a very short half-life of approximately 1–2 minutes because it is rapidly broken down by the enzyme dipeptidyl peptidase-4 (DPP-4). This is why therapeutic GLP-1 receptor agonists are chemically modified to resist degradation and provide longer-lasting effects.
What triggers GLP-1 release after eating?
GLP-1 release is triggered when nutrients—particularly carbohydrates, fats, and proteins—come into contact with L-cells in the intestine. These cells detect nutrients through specialised receptors and transporters, initiating the secretion of GLP-1 into the bloodstream.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












