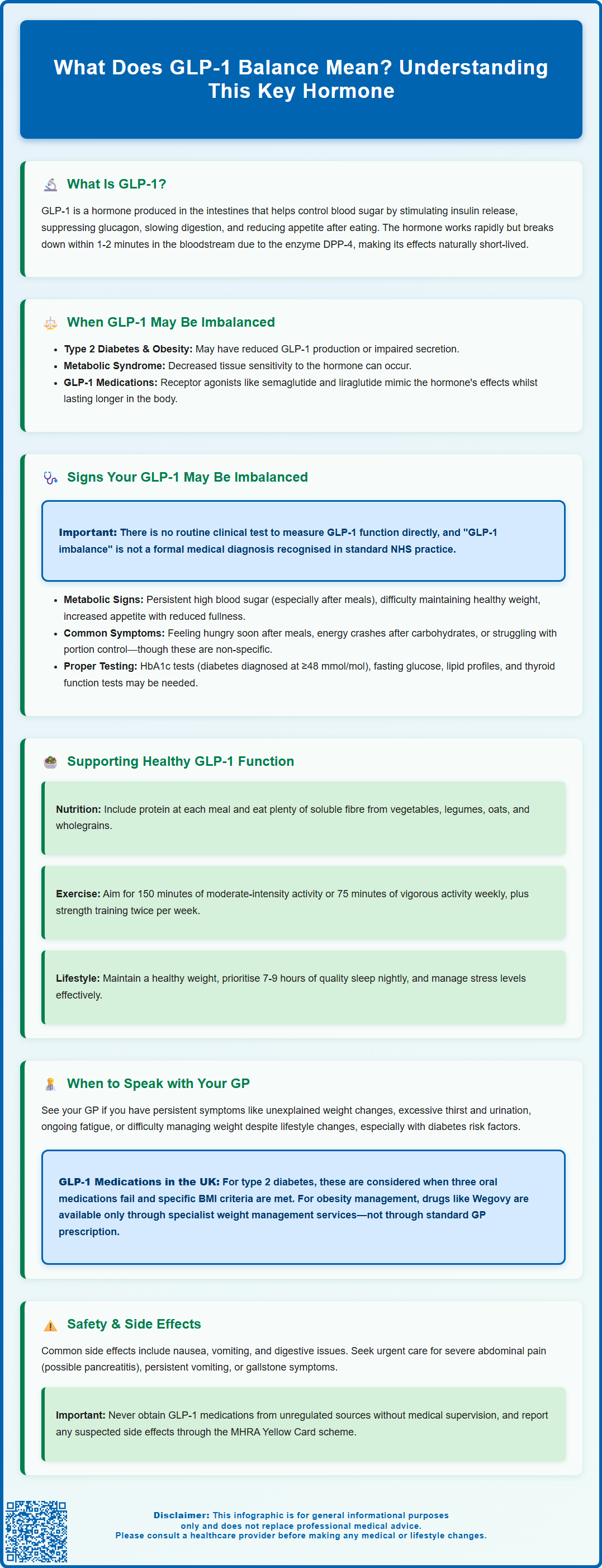
Glucagon-like peptide-1 (GLP-1) is a naturally occurring hormone that regulates blood glucose, appetite, and metabolism. Whilst "GLP-1 balance" is not a formal medical term, it describes the body's ability to produce and respond appropriately to this hormone. GLP-1 is released after eating, stimulating insulin secretion, suppressing glucagon, slowing gastric emptying, and promoting satiety. Alterations in GLP-1 function have been observed in type 2 diabetes and obesity. Understanding GLP-1 physiology has become increasingly relevant with the development of GLP-1 receptor agonists for diabetes and weight management under specialist guidance.
Summary: GLP-1 balance refers to the body's ability to produce and respond appropriately to glucagon-like peptide-1, a hormone that regulates blood glucose, appetite, and metabolism.
- GLP-1 is an incretin hormone produced by intestinal L-cells that stimulates insulin secretion, suppresses glucagon, slows gastric emptying, and promotes satiety in response to food intake.
- The hormone has a very short half-life of 1–2 minutes and is rapidly degraded by the enzyme dipeptidyl peptidase-4 (DPP-4) in circulation.
- Altered GLP-1 function has been observed in type 2 diabetes, obesity, and metabolic syndrome, though there is no routine clinical test to measure GLP-1 activity in standard NHS practice.
- GLP-1 receptor agonists such as semaglutide and liraglutide are prescribed for diabetes and, under specific NICE criteria, weight management through specialist services.
- Lifestyle approaches including protein and fibre intake, regular physical activity, healthy weight maintenance, and quality sleep may support natural GLP-1 function and overall metabolic health.
- Consult your GP if experiencing persistent metabolic symptoms such as unexplained weight changes, excessive thirst, ongoing fatigue, or difficulty managing weight despite lifestyle modifications.
Table of Contents
What Does GLP-1 Balance Mean?
Glucagon-like peptide-1 (GLP-1) is a naturally occurring incretin hormone produced primarily by specialised L-cells in the distal small intestine and colon. This hormone plays a crucial role in glucose homeostasis, appetite regulation, and metabolic health. The term "GLP-1 balance" is not a formal medical diagnosis or standard clinical term used by healthcare professionals, but rather a lay concept describing the body's ability to produce, secrete, and respond to appropriate levels of this hormone in response to food intake and metabolic demands.
In a well-functioning system, GLP-1 is released within minutes of eating, particularly in response to nutrients such as carbohydrates and fats. The hormone then acts on multiple target tissues: it stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, suppresses glucagon release from alpha cells, slows gastric emptying, and promotes satiety through central nervous system pathways. This coordinated response helps maintain blood glucose within normal ranges whilst regulating energy intake.
GLP-1 has a very short half-life of approximately 1-2 minutes in circulation, as it is rapidly degraded by the enzyme dipeptidyl peptidase-4 (DPP-4). Alterations in GLP-1 function may involve reduced production of the hormone or impaired secretion in response to meals. Decreased receptor sensitivity at target tissues has also been observed in some research contexts. Such alterations have been noted in individuals with type 2 diabetes, obesity, and metabolic syndrome, though the precise mechanisms remain an active area of research.
Understanding GLP-1 physiology has become increasingly relevant with the development of GLP-1 receptor agonists (such as semaglutide and liraglutide) for diabetes and, under specific criteria, weight management. These medications mimic the hormone's effects whilst resisting enzymatic breakdown. In the UK, GLP-1 receptor agonists for weight management are subject to NICE guidance and typically initiated through specialist services.
Signs Your GLP-1 May Be Imbalanced
It is important to note that there is no routine clinical test to directly measure GLP-1 function in standard NHS practice. Furthermore, "GLP-1 imbalance" is not a formal medical diagnosis. However, certain metabolic and clinical patterns may suggest suboptimal GLP-1 activity, though these signs are non-specific and can result from numerous other conditions.
Metabolic indicators that may be associated with reduced GLP-1 activity include:
-
Persistent elevated blood glucose levels, particularly postprandial (after-meal) hyperglycaemia
-
Difficulty achieving or maintaining a healthy weight despite dietary efforts
-
Increased appetite and reduced satiety after meals, leading to frequent snacking
-
Diagnosis of type 2 diabetes or non-diabetic hyperglycaemia (NDH, sometimes called prediabetes), conditions where GLP-1 response is often blunted
-
Features of metabolic syndrome, including central obesity, hypertension, and dyslipidaemia
Individuals may also notice practical symptoms such as feeling hungry shortly after eating substantial meals, experiencing energy crashes following carbohydrate-rich foods, or finding portion control particularly challenging. However, these experiences are common and multifactorial, influenced by dietary composition, stress, sleep quality, physical activity, and numerous other hormonal systems beyond GLP-1.
It is crucial to emphasise that experiencing these signs does not confirm a GLP-1 issue, nor is "GLP-1 imbalance" a recognised clinical diagnosis. These patterns warrant discussion with your GP, who can assess for underlying conditions such as diabetes, thyroid disorders, or other metabolic abnormalities through appropriate investigations. These may include HbA1c (diabetes is diagnosed at ≥48 mmol/mol or 6.5%; NDH at 42-47 mmol/mol or 6.0-6.4%), fasting plasma glucose (diabetes ≥7.0 mmol/L), lipid profiles, and thyroid function tests as clinically indicated.
Ways to Support Healthy GLP-1 Function
Whilst pharmaceutical GLP-1 receptor agonists are available by prescription for specific indications, several lifestyle and dietary approaches may support the body's natural GLP-1 production and function. These strategies are evidence-based for general metabolic health, though their specific effects on endogenous GLP-1 levels vary between individuals.
Dietary modifications that may support metabolic health include:
-
Including a source of protein at each meal, as protein can stimulate GLP-1 release
-
Including dietary fibre, particularly soluble fibre from vegetables, legumes, oats, and wholegrains, which may promote GLP-1 secretion through fermentation by gut bacteria
-
Eating regular, balanced meals that align with the NHS Eatwell Guide recommendations
-
Limiting ultra-processed foods high in refined carbohydrates and unhealthy fats
-
Considering fermented foods such as yoghurt, kefir, and sauerkraut, which may benefit overall gut health, though direct effects on GLP-1 require further research
Lifestyle factors that support metabolic health include:
-
Regular physical activity, with both aerobic exercise and resistance training showing benefits for glucose metabolism. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity or 75 minutes of vigorous activity weekly, plus strength exercises on at least 2 days
-
Achieving and maintaining a healthy weight, as obesity is associated with altered metabolic hormone responses
-
Prioritising sleep quality, as sleep deprivation affects multiple metabolic hormones
-
Managing stress, which can impact appetite regulation and glucose control
These approaches align with NICE guidance for preventing and managing type 2 diabetes (NG28) and obesity (CG189) and should be implemented as part of a holistic lifestyle approach. It is worth noting that whilst these strategies support overall metabolic health, they are not substitutes for prescribed medication when clinically indicated. Always discuss significant dietary or lifestyle changes with your healthcare team, particularly if you have existing medical conditions or take regular medications.
When to Speak with Your GP About GLP-1
You should arrange an appointment with your GP if you are experiencing persistent symptoms that may indicate metabolic dysfunction, regardless of whether they relate specifically to GLP-1. Key scenarios warranting medical review include:
Urgent or routine appointments should be considered if you notice:
-
Unexplained weight changes (significant loss or gain) despite stable eating patterns
-
Persistent excessive thirst and urination, which may indicate hyperglycaemia
-
Ongoing fatigue that impacts daily functioning
-
Symptoms of hypoglycaemia (shakiness, confusion, sweating) if you have diabetes
-
Difficulty managing your weight despite sustained lifestyle modifications
-
Family history of type 2 diabetes combined with risk factors such as obesity or PCOS
If you have established type 2 diabetes, GLP-1 receptor agonists may be considered according to NICE guidelines (NG28) when:
-
Triple therapy (metformin plus two other oral medications) is not effective, not tolerated, or contraindicated
-
You have a BMI ≥35 kg/m² (or ≥32.5 kg/m² for people from certain ethnic groups) with obesity-related complications, or BMI <35 kg/m² and insulin would have significant occupational implications or weight loss would benefit obesity-related comorbidities
Treatment is typically reviewed after 6 months and continued only if HbA1c has fallen by at least 11 mmol/mol (1%) and weight by at least 3%.
For obesity management, GLP-1 receptor agonists such as semaglutide 2.4mg (Wegovy) are recommended by NICE (TA875) only through specialist weight management services for people with specific BMI thresholds and weight-related complications.
Your clinician will evaluate potential benefits against risks, considering factors such as cardiovascular disease, renal function, and previous medication responses. Common side effects include nausea, vomiting, diarrhoea and constipation. Seek urgent medical advice if you experience severe, persistent abdominal pain (which might indicate pancreatitis), persistent vomiting leading to dehydration, or symptoms of gallstones. The risk of hypoglycaemia is generally low unless GLP-1 receptor agonists are combined with insulin or sulfonylureas.
If you experience any suspected side effects from medication, report them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Do not attempt to obtain GLP-1 medications without proper medical supervision, as unregulated sources pose significant safety risks. Your GP can provide evidence-based guidance tailored to your individual circumstances, ensuring any treatment aligns with current clinical standards and your overall health needs.
Frequently Asked Questions
Can I test my GLP-1 levels on the NHS?
There is no routine clinical test to directly measure GLP-1 function in standard NHS practice. Your GP can assess metabolic health through tests such as HbA1c, fasting glucose, and lipid profiles if you have symptoms suggesting metabolic dysfunction.
What foods help support natural GLP-1 production?
Protein-rich foods, dietary fibre from vegetables, legumes, oats, and wholegrains, and fermented foods such as yoghurt may support metabolic health and potentially influence GLP-1 secretion, though effects vary between individuals.
Who can be prescribed GLP-1 receptor agonists in the UK?
GLP-1 receptor agonists are prescribed for type 2 diabetes when other treatments are inadequate or unsuitable, according to NICE guidelines. For weight management, they are available only through specialist services for people meeting specific BMI and comorbidity criteria under NICE guidance.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript