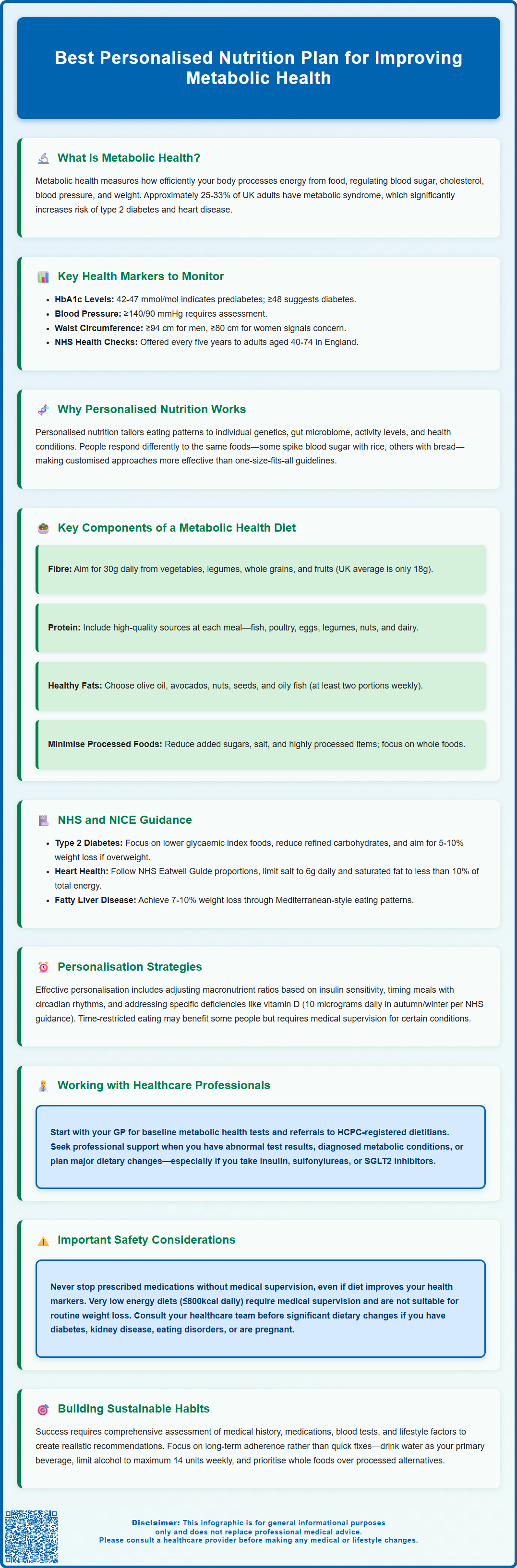
What's the best personalised nutrition plan for improving metabolic health? The answer depends on your unique biology, health status, and lifestyle. Personalised nutrition tailors dietary recommendations to individual characteristics—genetics, gut microbiome, activity levels, and existing conditions—rather than applying generic advice. This approach recognises that metabolic responses to identical foods vary considerably between people. Emerging research suggests personalised plans may improve outcomes such as blood glucose control, lipid profiles, and weight management more effectively than standard guidelines. Working with qualified healthcare professionals, including GPs and registered dietitians, ensures your plan is evidence-based, safe, and aligned with NHS and NICE guidance for conditions like type 2 diabetes, cardiovascular disease, and metabolic syndrome.
Summary: The best personalised nutrition plan for improving metabolic health is one tailored to your individual biology, health status, and lifestyle, developed with qualified healthcare professionals such as registered dietitians.
- Personalised nutrition adjusts macronutrient ratios, meal timing, and food choices based on individual insulin sensitivity, gut microbiome, genetics, and activity levels.
- Key dietary principles include prioritising fibre-rich carbohydrates, high-quality protein, unsaturated fats, and limiting processed foods high in saturated fat, salt, and free sugars.
- NICE and NHS guidance recommend intensive lifestyle programmes for metabolic conditions, with dietitians providing evidence-based, individualised advice.
- Regular monitoring of biomarkers (HbA1c, lipid profile, blood pressure, waist circumference) through NHS Health Checks enables timely intervention and plan adjustment.
- Individuals taking insulin, sulfonylureas, or SGLT2 inhibitors must consult their healthcare team before significant dietary changes due to hypoglycaemia or ketoacidosis risks.
Table of Contents
- What Is Metabolic Health and Why Does It Matter?
- How Personalised Nutrition Plans Support Metabolic Health
- Key Components of an Effective Metabolic Health Diet
- NHS and NICE Guidance on Nutrition for Metabolic Conditions
- Working with Healthcare Professionals for Personalised Plans
- Scientific References
- Frequently Asked Questions
What Is Metabolic Health and Why Does It Matter?
Metabolic health refers to the body's ability to efficiently process and utilise energy from food, maintaining optimal levels of blood glucose, lipids (cholesterol and triglycerides), blood pressure, and body composition. Good metabolic health means your body can effectively regulate insulin, manage inflammation, and maintain healthy weight—all fundamental processes that influence long-term wellbeing. While some people achieve metabolic health through lifestyle alone, others may maintain good metabolic function with appropriate medication.
Poor metabolic health significantly increases the risk of developing serious conditions including type 2 diabetes, cardiovascular disease, non-alcoholic fatty liver disease (NAFLD), and stroke. According to data from the Office for Health Improvement and Disparities (OHID), around a quarter to a third of UK adults have metabolic syndrome—a cluster of conditions including raised blood pressure, elevated blood sugar, excess abdominal fat, and abnormal cholesterol levels. When three or more of these risk factors occur together, the likelihood of developing cardiovascular disease and diabetes increases substantially.
The importance of metabolic health extends beyond disease prevention. Optimal metabolic function supports sustained energy levels, cognitive performance, immune function, and healthy ageing. Research demonstrates that metabolic dysfunction often develops silently over years, with many individuals unaware of deteriorating metabolic markers until clinical disease manifests. Early intervention through lifestyle modification, particularly nutrition, offers the most effective strategy for preventing progression to chronic disease.
Understanding your metabolic health status requires assessment of multiple biomarkers. Key indicators include:
-
Fasting blood glucose and HbA1c (glycated haemoglobin) – HbA1c of 42–47 mmol/mol indicates non-diabetic hyperglycaemia ('prediabetes'), while ≥48 mmol/mol suggests diabetes
-
Lipid profile (total cholesterol, LDL, HDL, triglycerides)
-
Blood pressure measurements – clinic readings ≥140/90 mmHg require assessment; readings ≥180/120 mmHg or with symptoms need urgent medical attention
-
Waist circumference (≥94 cm for men, ≥80 cm for women; lower thresholds of ≥90 cm apply for South Asian men) and body mass index (BMI)
-
Liver function tests, though these can be normal in early NAFLD
Regular monitoring through the NHS Health Check (offered to adults aged 40–74 in England every five years) provides valuable insight into metabolic status and enables timely intervention before irreversible damage occurs. Similar health assessment programmes exist in other UK nations.
How Personalised Nutrition Plans Support Metabolic Health
Personalised nutrition represents a shift from generic dietary advice to individualised eating patterns tailored to a person's unique biological, genetic, lifestyle, and health characteristics. This approach recognises that metabolic responses to identical foods vary considerably between individuals due to differences in genetics, gut microbiome composition, physical activity levels, sleep patterns, stress, and existing health conditions.
Emerging research, including studies published in Cell (Zeevi et al., 2015) and the PREDICT studies, demonstrates that personalised nutrition approaches show promise for improving metabolic outcomes compared to standard dietary guidelines, though long-term clinical outcomes remain under investigation. For example, continuous glucose monitoring studies reveal that blood sugar responses to the same meal can differ dramatically between people—some individuals experience significant glucose spikes from rice but minimal response to bread, whilst others show the opposite pattern. These inter-individual variations help explain why universal dietary recommendations often yield inconsistent results.
Personalised nutrition plans may support metabolic health through several mechanisms:
-
Optimising macronutrient ratios: Adjusting the balance of carbohydrates, proteins, and fats based on individual insulin sensitivity, activity levels, and metabolic goals. Some individuals thrive on moderate carbohydrate intake, whilst others with insulin resistance benefit from lower carbohydrate approaches.
-
Timing nutrient intake: Aligning eating patterns with circadian rhythms and individual schedules to optimise metabolic hormone secretion, particularly insulin and cortisol. Time-restricted eating or intermittent fasting may benefit certain individuals but requires medical supervision if you have diabetes (especially if taking insulin, sulfonylureas or SGLT2 inhibitors), are pregnant, have an eating disorder, are underweight, or are an adolescent.
-
Addressing micronutrient needs: Identifying and addressing specific vitamin and mineral requirements (such as vitamin D, which the NHS recommends at 10 micrograms daily during autumn and winter, magnesium, or B vitamins) that support metabolic function. People taking metformin long-term should have B12 levels checked.
-
Managing food sensitivities: Identifying foods that trigger digestive symptoms through structured elimination and reintroduction under professional guidance, which may improve overall dietary quality and adherence.
The personalisation process typically involves comprehensive assessment including medical history, current medications, blood test results, dietary preferences, cultural considerations, and practical constraints. This holistic approach ensures recommendations are not only metabolically beneficial but also sustainable and realistic for long-term adherence—a critical factor often overlooked in generic dietary advice.
Key Components of an Effective Metabolic Health Diet
Whilst personalisation is essential, certain nutritional principles consistently support metabolic health across diverse populations. An effective metabolic health diet emphasises whole, minimally processed foods that stabilise blood glucose, reduce inflammation, support healthy lipid profiles, and promote sustainable weight management.
Prioritising fibre-rich carbohydrates forms the foundation of metabolic nutrition. Dietary fibre slows glucose absorption, promotes satiety, feeds beneficial gut bacteria, and helps regulate cholesterol levels. Excellent sources include vegetables, legumes (beans, lentils, chickpeas), whole grains (oats, quinoa, brown rice), and fruits. The Scientific Advisory Committee on Nutrition (SACN) recommends 30g of fibre daily, yet average UK intake remains around 18g. Gradually increasing fibre intake whilst maintaining adequate hydration prevents digestive discomfort.
High-quality protein intake supports metabolic health by preserving lean muscle mass (which enhances insulin sensitivity), promoting satiety, and requiring more energy for digestion compared to carbohydrates or fats. Aim for protein sources including fish, poultry, eggs, legumes, nuts, seeds, and dairy products. The NHS recommends eating at least two portions of fish per week, including one portion of oily fish. Distributing protein across meals, rather than concentrating intake at dinner, optimises muscle protein synthesis and metabolic benefits.
Healthy fats play crucial roles in hormone production, nutrient absorption, and inflammation regulation. Emphasise unsaturated fats from olive oil, avocados, nuts, seeds, and oily fish (salmon, mackerel, sardines) whilst limiting saturated fats from processed meats, pastries, and fried foods. Check food labels for partially hydrogenated oils (trans fats), though levels in UK foods are generally low.
Limiting foods high in saturated fat, salt and free sugars represents an important dietary modification. These products—often highly processed with long ingredient lists including additives, preservatives, and refined ingredients—are associated with weight gain, insulin resistance, and inflammation. Focus instead on foods requiring minimal preparation: fresh produce, whole grains, lean proteins, and simple cooking methods, as outlined in the NHS Eatwell Guide.
Adequate hydration supports metabolic processes, with water being the optimal choice. Limit sugar-sweetened beverages and restrict fruit juices and smoothies to no more than 150ml per day (counting as a maximum of one portion towards your '5 A Day'). The UK Chief Medical Officers advise limiting alcohol consumption to no more than 14 units per week, spread over several days, with several alcohol-free days each week.
NHS and NICE Guidance on Nutrition for Metabolic Conditions
The National Institute for Health and Care Excellence (NICE) and NHS provide evidence-based guidance for managing metabolic conditions through nutrition, emphasising structured lifestyle interventions as first-line treatment before pharmacological approaches.
For type 2 diabetes prevention, NICE guideline NG215 recommends intensive lifestyle programmes for those at high risk. The Healthier You: NHS Diabetes Prevention Programme offers eligible individuals (those with non-diabetic hyperglycaemia or 'prediabetes', HbA1c 42–47 mmol/mol) access to structured education and support. For diabetes management, NICE guideline NG28 provides dietary recommendations including:
-
Considering lower glycaemic index (GI) foods as part of an overall healthy dietary pattern
-
Reducing total calorie intake if overweight, aiming for 5–10% weight loss
-
Limiting refined carbohydrates and sugar-sweetened beverages
-
Increasing dietary fibre to at least 30g daily
-
Including at least two portions of fish weekly, one of which should be oily
For cardiovascular disease prevention, NICE guidance on lipid modification and cardiovascular risk emphasises dietary patterns proven to reduce cardiovascular risk. The NHS Eatwell Guide provides a visual representation of recommended proportions: approximately one-third vegetables and fruits, one-third starchy carbohydrates (preferably wholegrain), with remaining portions divided between proteins and dairy, plus small amounts of unsaturated fats. Specific recommendations include limiting salt intake to 6g daily and reducing saturated fat to less than 10% of total energy intake.
For obesity management, NICE guideline CG189 recommends multicomponent interventions addressing diet, physical activity, and behaviour change. Dietary approaches should create a sustainable calorie deficit of 600kcal daily, achieved through portion control, reducing energy-dense foods, and increasing nutrient-dense options. Very low energy diets (≤800kcal daily) are not for routine use and require medical supervision, typically as part of structured programmes such as the NHS Type 2 Diabetes Path to Remission Programme. These are time-limited interventions for specific individuals, particularly those with type 2 diabetes, as evidence suggests potential for disease remission.
For non-alcoholic fatty liver disease (NAFLD), NICE guideline NG49 recommends weight loss of 7–10% for those overweight or obese, achieved through calorie reduction and increased physical activity. Mediterranean-style dietary patterns show particular promise for improving liver health markers.
These guidelines emphasise that dietary changes should be individualised, culturally appropriate, and sustainable, with regular review and adjustment based on clinical outcomes and patient preferences.
Working with Healthcare Professionals for Personalised Plans
Developing an effective personalised nutrition plan for metabolic health requires collaboration with qualified healthcare professionals who can assess your individual needs, interpret clinical data, and provide evidence-based recommendations tailored to your circumstances.
Your GP serves as the initial point of contact for metabolic health concerns. They can arrange baseline investigations including blood tests (fasting glucose, HbA1c, lipid profile, liver function), blood pressure measurement, and anthropometric assessments. Based on results, your GP may diagnose metabolic conditions, prescribe medications if necessary, and refer you to specialist services. The NHS Health Check, available to adults aged 40–74 in England, provides systematic screening for cardiovascular and metabolic risk factors.
Registered dietitians are the most qualified professionals for personalised nutrition advice. They complete rigorous university training and maintain registration with the Health and Care Professions Council (HCPC). Dietitians can be accessed through:
-
NHS referrals: Your GP can refer you to NHS dietetic services, particularly if you have diagnosed conditions like diabetes, cardiovascular disease, or obesity. Waiting times vary by region. NHS weight management services are available at different tiers depending on need.
-
Private practice: Many dietitians offer private consultations, providing more immediate access and extended appointment times. Ensure practitioners are HCPC-registered and members of the British Dietetic Association (BDA).
Registered Nutritionists (RNutr or ANutr) are qualified nutrition professionals registered with the UK Voluntary Register of Nutritionists (UKVRN), maintained by the Association for Nutrition. While 'nutritionist' itself is not a protected title, checking UKVRN registration ensures appropriate qualifications.
Diabetes specialist nurses and educators offer valuable support for those with diabetes or prediabetes, providing structured education programmes (such as DESMOND or DAFNE) that include nutritional guidance alongside medication management and self-monitoring techniques.
When to seek professional support:
-
You have abnormal blood test results indicating metabolic dysfunction
-
You've been diagnosed with diabetes, cardiovascular disease, or metabolic syndrome
-
You're struggling to achieve metabolic health goals independently
-
You're considering significant dietary changes and want professional guidance
-
You're taking medications that may interact with dietary modifications
Seek urgent medical attention if you experience symptoms of high blood glucose (excessive thirst, frequent urination, unexplained weight loss), blood pressure readings ≥180/120 mmHg, or any acute symptoms such as chest pain or neurological deficits.
Important safety considerations: Never discontinue prescribed medications without consulting your doctor, even if dietary changes improve your metabolic markers. Some medications require gradual adjustment as metabolic health improves, and this must be medically supervised. If you take insulin, sulfonylureas or SGLT2 inhibitors, consult your healthcare team before making significant dietary changes or attempting intermittent fasting due to risks of hypoglycaemia or euglycaemic diabetic ketoacidosis. Similarly, individuals with kidney disease, eating disorders, pregnancy, or other complex health conditions require specialist input before making significant dietary changes.
Successful metabolic health improvement through personalised nutrition is a collaborative journey. Regular monitoring, honest communication with your healthcare team, and realistic goal-setting create the foundation for sustainable improvements in metabolic health and overall wellbeing.
Scientific References
Frequently Asked Questions
What is metabolic health and why is it important?
Metabolic health refers to the body's ability to efficiently process energy from food, maintaining optimal blood glucose, lipids, blood pressure, and body composition. Good metabolic health reduces the risk of type 2 diabetes, cardiovascular disease, non-alcoholic fatty liver disease, and stroke, whilst supporting sustained energy, cognitive function, and healthy ageing.
How does personalised nutrition differ from standard dietary advice?
Personalised nutrition tailors eating patterns to individual characteristics such as genetics, gut microbiome, insulin sensitivity, and lifestyle factors, recognising that metabolic responses to identical foods vary considerably between people. This individualised approach may improve outcomes more effectively than generic dietary guidelines.
Who should I consult for a personalised metabolic health nutrition plan?
Consult your GP initially for metabolic health assessment and blood tests, then seek referral to a registered dietitian (HCPC-registered) for evidence-based, personalised nutrition advice. Dietitians are available through NHS referrals or private practice and can tailor plans to your medical history, medications, and individual needs.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












