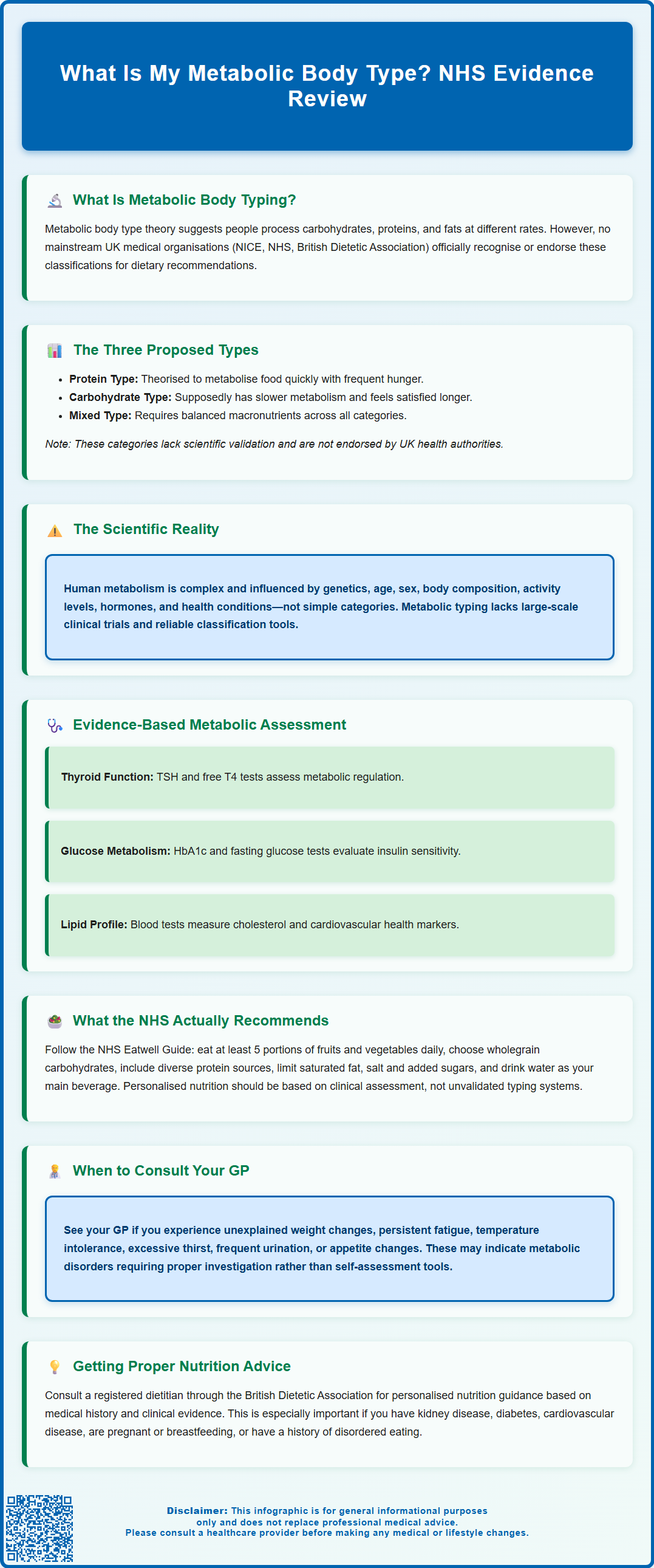
The concept of metabolic body types suggests that individuals process carbohydrates, proteins, and fats differently, influencing dietary needs and energy levels. Whilst this theory has gained popularity in wellness circles, it is important to understand that mainstream UK medical organisations—including NICE, the NHS, and the British Dietetic Association—do not recognise metabolic typing as a validated diagnostic or therapeutic approach. Human metabolism is influenced by numerous factors such as genetics, age, hormonal status, and underlying health conditions, creating complex individual profiles that extend beyond simplified categories. This article examines the metabolic typing concept, its proposed classifications, and evidence-based alternatives recommended by UK health authorities.
Summary: Metabolic body types are theoretical classifications suggesting individuals process macronutrients differently, but this concept lacks validation from UK medical organisations including NICE, the NHS, and the British Dietetic Association.
- The metabolic typing theory proposes three categories (protein, carbohydrate, and mixed types) based on how individuals supposedly convert food to energy, though these lack clinical validation.
- Human metabolism is influenced by genetics, age, body composition, hormonal status, and health conditions rather than fitting into predetermined categories.
- No large-scale randomised controlled trials support metabolic typing, and validated tools for accurate classification do not exist.
- The NHS recommends evidence-based personalised nutrition following the Eatwell Guide and tailored interventions for specific diagnosed conditions rather than metabolic typing.
- Consult your GP for appropriate metabolic assessment including thyroid function tests, HbA1c, and referral to registered dietitians for evidence-based nutritional guidance.
Table of Contents
What Is a Metabolic Body Type?
The concept of metabolic body types suggests that individuals process macronutrients—carbohydrates, proteins, and fats—at different rates and with varying efficiency. This theory proposes that understanding your metabolic type can help tailor dietary choices to optimise energy levels, weight management, and overall health. The idea gained popularity through various wellness programmes and dietary approaches, particularly in the alternative health community.
Proponents of metabolic typing argue that people fall into distinct categories based on how their bodies convert food into energy. These classifications are thought to influence nutritional needs and physical characteristics, though claims about links to personality traits lack scientific evidence.
It is important to note that whilst the concept of metabolic body types has gained considerable attention in popular health literature, there is no official link established by mainstream medical organisations such as NICE, the British Dietetic Association (BDA), or the NHS between specific metabolic "types" and prescribed dietary interventions. The human metabolism is influenced by numerous factors including genetics, age, sex, body composition, physical activity levels, hormonal status, and underlying health conditions. These variables create a complex metabolic profile that may not fit neatly into predetermined categories.
Understanding metabolism remains clinically relevant, particularly for managing specific conditions such as diabetes, thyroid disorders, and obesity. However, the simplified categorisation into distinct metabolic types should be approached with appropriate scientific scrutiny and distinguished from evidence-based metabolic assessment used in clinical practice.
The Three Main Metabolic Body Types Explained
The metabolic typing system typically classifies individuals into three primary categories: protein types, carbohydrate types, and mixed types. Each classification is associated with different macronutrient requirements and metabolic characteristics, though it's important to emphasise that these distinctions lack robust clinical validation and are not endorsed by UK health authorities.
According to the theory, protein types are described as individuals who theoretically metabolise food quickly and may experience frequent hunger. Proponents suggest these individuals might feel better with diets higher in protein and healthy fats, with moderate carbohydrate intake. The concept suggests they have a "faster oxidative rate" (a term not recognised in conventional clinical practice), meaning their cells supposedly convert food to energy rapidly.
Carbohydrate types are characterised in this theory as having slower metabolic rates and may feel satisfied for longer periods after eating. The theory suggests these individuals might respond better to diets higher in complex carbohydrates with moderate protein and lower fat content. They are described as having a "slower oxidative rate" and may experience different energy patterns when consuming whole grains, vegetables, and lean proteins.
Mixed types are said to fall between the two extremes, requiring a balanced approach to all three macronutrients.
Whilst these classifications provide a framework for thinking about individual dietary needs, it is crucial to recognise that human metabolism exists on a spectrum rather than in discrete categories. Factors such as insulin sensitivity, thyroid function, and gut microbiome composition contribute to metabolic individuality in ways that extend far beyond these simplified classifications. The MHRA, NICE and the BDA do not endorse metabolic typing as a diagnostic or therapeutic approach.
Important safety note: If you have existing medical conditions (such as kidney disease, cardiovascular disease, or diabetes), are pregnant or breastfeeding, or have a history of disordered eating, consult your GP or a registered dietitian before making significant changes to your macronutrient intake or following any restrictive dietary pattern.
How to Identify Your Metabolic Body Type
Various methods have been proposed for identifying metabolic body types, though none have been validated through rigorous clinical trials or endorsed by UK medical regulatory bodies. Common approaches include questionnaires assessing dietary preferences, energy patterns, and physical characteristics. These self-assessment tools typically ask about hunger frequency, food cravings, energy levels throughout the day, and responses to different types of meals.
Some practitioners offer more elaborate testing, including analysis of body composition, blood glucose responses to meals, or even genetic testing. However, there is no official link between these assessments and clinically meaningful metabolic classifications. The interpretation of such tests often relies on proprietary systems rather than evidence-based medical guidelines.
Observational approaches suggested by metabolic typing advocates include:
-
Monitoring energy levels after consuming meals with different macronutrient ratios
-
Noting hunger patterns and satiety duration following various food combinations
-
Assessing mood, concentration, and physical performance in relation to dietary intake
-
Tracking weight changes and body composition responses to different eating patterns
If you are concerned about your metabolism or wish to optimise your nutrition, the NHS recommends consulting your GP or requesting referral to a registered dietitian. These healthcare professionals can conduct evidence-based assessments including:
-
Thyroid function tests (typically TSH with free T4 as first-line tests, per NICE guideline NG145)
-
HbA1c and fasting plasma glucose to assess glycaemia and diabetes risk
-
Lipid profiles to evaluate cardiovascular health
-
Body composition analysis using validated methods such as BMI, waist circumference, and waist-to-height ratio
A registered dietitian (find one through the British Dietetic Association's directory) can provide personalised nutritional guidance based on your medical history, current health status, and specific goals, using approaches supported by clinical evidence rather than unvalidated typing systems.
Does Metabolic Typing Have Scientific Evidence?
The scientific evidence supporting metabolic body typing as a valid framework for dietary prescription remains limited and inconclusive. Systematic reviews and meta-analyses have not established robust support for the core principles of metabolic typing theory. The concept lacks the rigorous validation required for acceptance by mainstream medical organisations including NICE, the NHS, and the British Dietetic Association.
Key limitations in the evidence base include:
-
Absence of large-scale, randomised controlled trials comparing metabolic type-based diets to standard nutritional approaches
-
Lack of validated, reliable tools for accurately classifying individuals into metabolic types
-
Inconsistent definitions and criteria across different metabolic typing systems
-
Limited peer-reviewed publications in reputable medical journals
-
Failure to account for the dynamic nature of metabolism, which changes with age, activity, and health status
Whilst individual metabolic variation is scientifically established, the evidence supports a more nuanced understanding than categorical typing systems suggest. Research in nutrigenomics and personalised nutrition demonstrates that genetic variations influence nutrient metabolism, but these effects are complex and involve multiple genes interacting with environmental factors. Single-gene polymorphisms rarely dictate entire dietary patterns.
What the evidence does support is that certain metabolic parameters have clinical relevance. Insulin resistance can be assessed through glucose tolerance tests, though measures like HOMA-IR are primarily used in research rather than routine UK clinical practice. Thyroid function, assessed via TSH and free T4 (per NICE guideline NG145), influences metabolic rate and nutritional needs. These evidence-based assessments differ fundamentally from metabolic typing classifications.
The NHS and NICE emphasise individualised nutritional care based on clinical assessment, medical history, and specific health conditions rather than predetermined metabolic categories. If you have concerns about your metabolism, contact your GP for appropriate investigation rather than relying on unvalidated typing systems. Warning signs requiring medical attention include unexplained weight changes, persistent fatigue, temperature intolerance, or changes in appetite or bowel habits.
Personalised Nutrition and Metabolism: What the NHS Recommends
The NHS advocates for evidence-based approaches to personalised nutrition that consider individual health status, medical conditions, and lifestyle factors rather than categorical metabolic typing. NICE guidelines emphasise comprehensive assessment and tailored interventions for specific conditions affecting metabolism, including obesity, type 2 diabetes, and cardiovascular disease.
Core principles of NHS nutritional guidance include:
-
Following the NHS Eatwell Guide, which recommends balanced intake from all food groups: fruits and vegetables (at least 5 portions daily), starchy carbohydrates (preferably wholegrain), proteins (including plant-based sources), dairy or alternatives, and limited amounts of oils and spreads
-
Maintaining appropriate energy balance for healthy weight management
-
Limiting intake of foods high in saturated fat, salt, and added sugars
-
Staying adequately hydrated with water as the primary beverage
-
Considering specific dietary modifications for diagnosed medical conditions
For individuals with metabolic concerns, the NHS recommends evidence-based interventions rather than metabolic typing. These include structured weight management programmes for obesity (NICE guideline CG189), dietary approaches for type 2 diabetes management focusing on carbohydrate quality and quantity (NICE guideline NG28), and cardiovascular risk reduction through dietary modification (NICE guideline NG238).
When to seek professional guidance:
Contact your GP if you experience unexplained weight loss or gain, persistent fatigue, changes in appetite, or symptoms suggesting metabolic disorders such as excessive thirst, frequent urination, or temperature intolerance. Your GP can arrange appropriate investigations and refer you to specialist services including registered dietitians, endocrinologists, or weight management programmes as clinically indicated.
Registered dietitians provide personalised nutritional advice based on comprehensive assessment including medical history, biochemical markers, body composition (including BMI and waist measurements), dietary intake analysis, and individual preferences. This evidence-based approach to personalised nutrition differs fundamentally from metabolic typing, offering interventions supported by clinical research and aligned with UK medical guidelines. The British Dietetic Association maintains a directory of registered practitioners who can provide safe, effective nutritional guidance tailored to your individual circumstances.
Frequently Asked Questions
Are metabolic body types recognised by the NHS?
No, metabolic body types are not recognised by the NHS, NICE, or the British Dietetic Association as a validated diagnostic or therapeutic approach. The NHS recommends evidence-based personalised nutrition based on comprehensive clinical assessment rather than categorical typing systems.
What should I do if I'm concerned about my metabolism?
Contact your GP for appropriate investigation, which may include thyroid function tests, HbA1c, and lipid profiles. Your GP can refer you to a registered dietitian for evidence-based nutritional guidance tailored to your individual health status and medical conditions.
Is there scientific evidence supporting metabolic typing diets?
No, systematic reviews have not established robust support for metabolic typing theory. Large-scale randomised controlled trials are absent, and validated tools for accurate classification do not exist, limiting acceptance by mainstream medical organisations.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript