How to taper off Saxenda is a common question for patients discontinuing this GLP-1 receptor agonist used for weight management. Saxenda (liraglutide 3.0 mg) does not typically require a formal tapering schedule, as it clears the body relatively quickly and causes no dangerous withdrawal effects. However, some clinicians recommend a gradual dose reduction for practical and psychological reasons. Discontinuation should always be discussed with your GP or prescribing clinician to ensure safe transition and establish a plan for ongoing weight maintenance. Understanding what to expect after stopping—including appetite changes and potential weight regain—helps you prepare appropriate strategies for long-term success.
Summary: Saxenda does not typically require formal tapering, as it clears the body quickly without causing dangerous withdrawal effects, though some clinicians may suggest gradual dose reduction for practical reasons.
- Liraglutide (Saxenda) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with comorbidities.
- Discontinuation should be discussed with your GP or prescribing clinician to ensure safe transition and establish ongoing weight management plans.
- Increased appetite and hunger are common after stopping as the medication's satiety effects diminish over days to weeks.
- Weight regain is well-documented after discontinuation, but successful maintenance is achievable with dietary management, physical activity, and behavioural support.
- Patients with type 2 diabetes may require blood glucose monitoring and medication adjustments after stopping Saxenda.
- Severe abdominal pain or persistent vomiting after discontinuation requires urgent medical review via NHS 111, your GP, or A&E.
Table of Contents
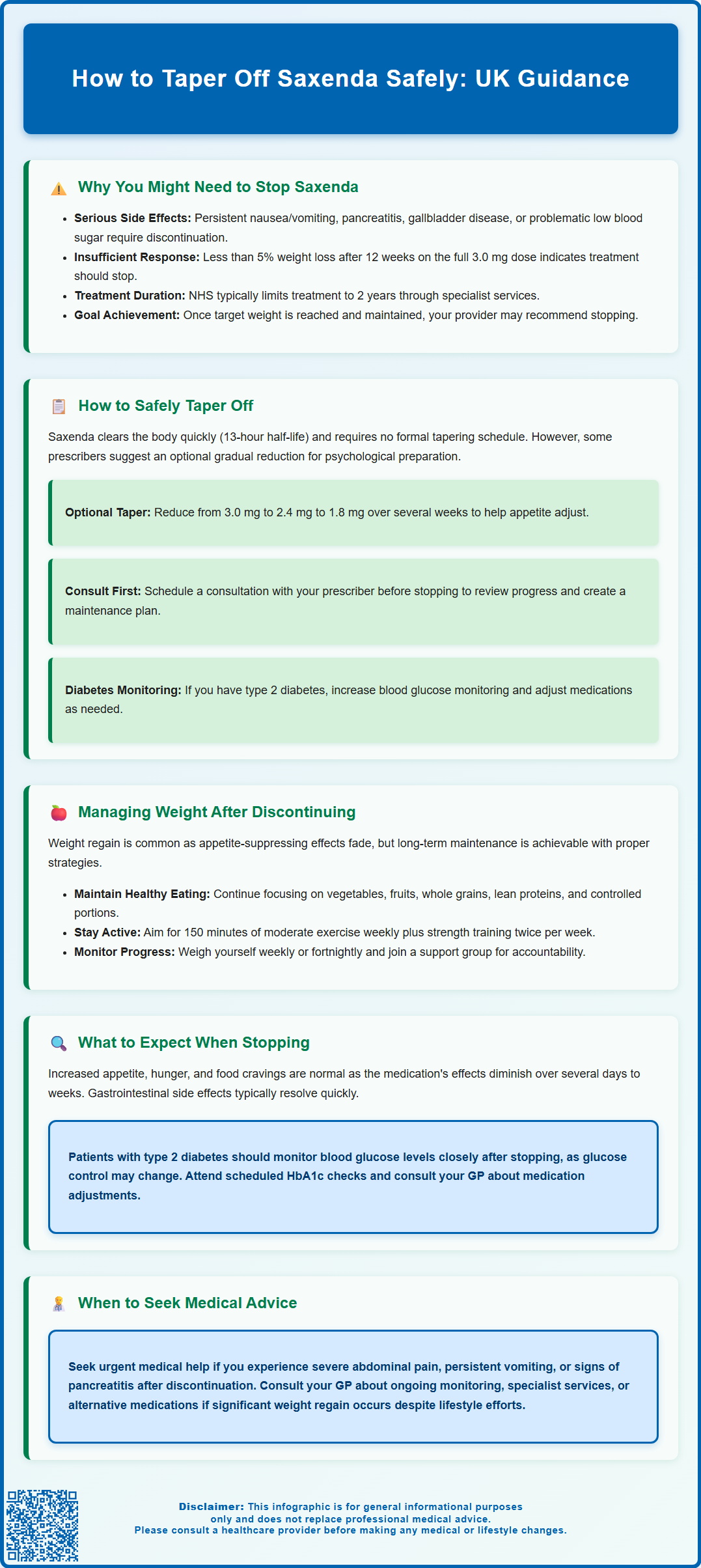
Why You Might Need to Stop Saxenda
Saxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with weight-related comorbidities. It is also licensed for certain adolescents (aged 12 to <18 years with body weight >60 kg). Whilst many patients achieve meaningful weight loss with Saxenda, there are several legitimate reasons why discontinuation may become necessary.
Medical reasons for stopping include the development of adverse effects that significantly impact quality of life. Common gastrointestinal symptoms such as persistent nausea, vomiting, or diarrhoea may prove intolerable for some patients despite dose adjustments. More serious concerns include acute pancreatitis, gallbladder disease, or hypoglycaemia (particularly in patients with type 2 diabetes on concurrent glucose-lowering medications such as sulfonylureas or insulin). Saxenda is contraindicated in pregnancy, so women who become pregnant or are planning conception must discontinue treatment immediately.
Treatment response considerations also guide discontinuation decisions. NICE guidance recommends stopping Saxenda if patients have not lost at least 5% of their initial body weight after 12 weeks on the 3.0 mg daily maintenance dose. This threshold ensures that treatment continues only when clinically beneficial. Additionally, once patients reach their target weight or have maintained weight loss for a sustained period, healthcare professionals may discuss stopping treatment as part of a transition to long-term lifestyle maintenance. NHS treatment with Saxenda typically occurs within specialist weight management services and is often time-limited (commonly up to 2 years).
Practical factors such as cost, needle phobia that develops during treatment, or significant life changes may also necessitate stopping Saxenda. Some patients may wish to attempt weight maintenance without medication after achieving their goals. Whatever the reason, discontinuation should ideally be discussed with your GP or prescribing clinician to ensure a safe and supported transition.
How to Safely Taper Off Saxenda
Unlike some medications that require gradual dose reduction to prevent withdrawal symptoms, Saxenda does not typically require a formal tapering schedule from a pharmacological perspective. Liraglutide has a half-life of approximately 13 hours, meaning it clears from the body relatively quickly after the final dose. There is no official guidance from the MHRA or manufacturer requiring a step-down approach, and abrupt cessation does not cause dangerous physiological withdrawal effects.
However, some clinicians and patients prefer a gradual reduction approach for practical and psychological reasons. This is optional, not required by the SmPC or MHRA, and should be prescriber-led. If you have been using the maximum 3.0 mg daily dose, your prescriber might suggest reducing to 2.4 mg for one to two weeks, then 1.8 mg for another week before stopping completely. This approach may help your appetite regulation adjust more gradually and can provide psychological preparation for managing weight without medication. It may also minimise any rebound increase in appetite that some patients experience, though this is not evidence-based.
Before stopping Saxenda, schedule a consultation with your prescribing doctor or practice nurse. This appointment should cover your reasons for discontinuation, review your weight loss progress, and establish a plan for ongoing weight management. Your healthcare provider can assess whether stopping is appropriate at this time or whether alternative strategies might be beneficial. They should also review any other medications you take, particularly if you have type 2 diabetes, as glucose control may change after stopping a GLP-1 receptor agonist. If you take insulin or sulfonylureas, you may need more frequent blood glucose monitoring and medication adjustments.
Important safety considerations include monitoring for any unusual symptoms after stopping. If you experience severe abdominal pain, persistent vomiting, or signs of pancreatitis in the weeks following discontinuation, seek urgent medical help via NHS 111, your GP, or A&E if symptoms are severe. Keep a record of your final dose and the date you stopped, as this information may be relevant for future medical consultations. If you are stopping due to side effects, ensure these are documented in your medical records and consider reporting them through the MHRA Yellow Card scheme.
Managing Weight After Discontinuing Saxenda
Weight regain after stopping Saxenda is a common concern and a well-documented phenomenon in clinical studies. Research indicates that many patients experience some weight regain following discontinuation, as the appetite-suppressing effects of liraglutide diminish. However, successful long-term weight maintenance is achievable with appropriate strategies and support.
Dietary management becomes paramount after stopping Saxenda. Focus on maintaining the healthy eating patterns you established during treatment rather than reverting to previous habits. A balanced diet rich in vegetables, fruits, whole grains, and lean proteins, with controlled portions, forms the foundation of weight maintenance. Consider continuing to use strategies that worked well during treatment, such as meal planning, food diaries, or mindful eating practices. The NHS Better Health weight loss plan and resources from the British Dietetic Association provide evidence-based guidance. Some patients benefit from referral to a registered dietitian for personalised advice, particularly if they have complex nutritional needs or comorbidities.
Physical activity plays a crucial role in preventing weight regain. Current UK Chief Medical Officers' guidelines recommend at least 150 minutes of moderate-intensity aerobic activity weekly, plus strength training twice weekly. If you were not exercising regularly during Saxenda treatment, now is an excellent time to establish this habit. Activities need not be intensive—brisk walking, swimming, cycling, or gardening all contribute to energy expenditure and metabolic health. Building muscle through resistance exercises is particularly valuable, as muscle tissue burns more calories at rest than fat tissue.
Behavioural strategies and support significantly improve long-term outcomes. Consider joining a weight management group (such as those offered through NHS services or commercial programmes), which provides accountability and peer support. Regular self-weighing (weekly or fortnightly) helps detect early weight regain, allowing prompt intervention. Set realistic expectations: maintaining most of your weight loss is a success, even if some regain occurs. Discuss with your GP whether ongoing monitoring appointments or referral to specialist weight management services would be beneficial. Some patients may be candidates for alternative weight management medications if significant regain occurs despite lifestyle efforts, though NHS access follows specific NICE criteria.
What to Expect When Stopping Saxenda
Understanding the physiological and psychological changes that may occur after discontinuing Saxenda helps you prepare and respond appropriately. Appetite changes are typically the most noticeable effect. Saxenda works by mimicking GLP-1, a hormone that promotes satiety and reduces hunger. When you stop treatment, these effects gradually diminish over several days to weeks. Many patients report increased appetite, more frequent hunger sensations, and stronger food cravings—particularly for high-calorie, palatable foods. This is a normal physiological response as your body's natural appetite regulation resumes. Being prepared for this change allows you to implement coping strategies proactively.
Gastrointestinal symptoms that some patients experienced during treatment—such as nausea, altered bowel habits, or early satiety—typically resolve within days to weeks of stopping. Your digestive system returns to its pre-treatment state. Conversely, if you had adapted well to Saxenda and experienced no side effects, you should not develop new gastrointestinal symptoms upon stopping. Any severe or persistent abdominal symptoms warrant urgent medical review—contact NHS 111 or go to A&E if symptoms are severe.
Weight and metabolic changes vary considerably between individuals. Some patients maintain their weight loss successfully, whilst others experience gradual regain over subsequent months. Clinical studies of GLP-1 receptor agonists suggest that without ongoing intervention, weight regain is common after discontinuation, though the extent varies between individuals. Your metabolic rate may decrease slightly as your body weight stabilises, which is a normal adaptive response. If you have type 2 diabetes, your glucose control may change after stopping Saxenda, so monitor blood glucose levels as advised by your diabetes team and attend scheduled HbA1c checks.
Psychological and emotional responses to stopping Saxenda should not be underestimated. Some patients feel anxious about managing weight independently or fear regaining lost weight. Others feel relief at no longer needing daily injections. Acknowledge these feelings and seek support if needed—your GP can provide reassurance or refer you to appropriate services. Remember that stopping Saxenda does not represent failure; it is simply a transition to a different phase of weight management. If you experience significant weight regain or find maintenance particularly challenging, discuss with your healthcare provider whether restarting treatment or exploring alternative options might be appropriate.
Frequently Asked Questions
Do I need to gradually reduce my Saxenda dose before stopping?
Saxenda does not typically require formal tapering from a pharmacological perspective, as it clears the body quickly without causing dangerous withdrawal effects. However, some clinicians may suggest gradual dose reduction (e.g., 3.0 mg to 2.4 mg to 1.8 mg over several weeks) for practical and psychological reasons, though this is optional and should be prescriber-led.
Will I regain weight after stopping Saxenda?
Weight regain is common after discontinuing Saxenda as appetite-suppressing effects diminish, but successful long-term maintenance is achievable with appropriate dietary management, regular physical activity, and behavioural support strategies. Discuss ongoing weight management plans with your GP or specialist weight management service.
What should I do if I experience severe symptoms after stopping Saxenda?
If you experience severe abdominal pain, persistent vomiting, or signs of pancreatitis after discontinuing Saxenda, seek urgent medical help via NHS 111, your GP, or A&E if symptoms are severe. Keep a record of your final dose and discontinuation date for future medical consultations.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript