Metabolic therapy encompasses medical interventions designed to address disorders affecting the body's biochemical processes that convert food into energy and essential molecules. These therapies range from dietary modifications and enzyme replacement to pharmacological treatments, targeting both rare inherited metabolic diseases and common conditions such as diabetes and dyslipidaemia. In the UK, specialist metabolic medicine services coordinate individualised care through multidisciplinary teams, with treatment plans tailored to each patient's specific metabolic defect. Early diagnosis and prompt intervention can prevent irreversible complications, particularly neurological damage, making metabolic therapy a vital component of NHS care for thousands of patients.
Summary: Metabolic therapy comprises medical interventions that correct, compensate for, or manage abnormalities in metabolic pathways caused by genetic conditions, acquired diseases, or lifestyle factors.
- Treatment approaches include dietary modification, enzyme replacement therapy, pharmacological interventions, and vitamin or cofactor supplementation tailored to specific metabolic defects.
- Conditions treated range from rare inherited metabolic disorders such as phenylketonuria and lysosomal storage diseases to common conditions including diabetes mellitus and dyslipidaemia.
- Specialist metabolic centres across the UK provide multidisciplinary care coordinated through NHS England, with 24-hour emergency protocols for acute metabolic decompensation.
- Regular biochemical monitoring ensures therapeutic targets are achieved whilst minimising adverse effects such as nutritional deficiencies, infusion reactions, or medication-specific complications.
- Early diagnosis through the NHS Newborn Blood Spot Screening Programme enables prompt treatment initiation, preventing irreversible neurological damage in inherited metabolic disorders.
Table of Contents
What Is Metabolic Therapy?
Metabolic therapy refers to a range of medical interventions designed to address disorders of metabolism—the complex biochemical processes that convert food into energy and building blocks for growth, repair, and cellular function. These therapies aim to correct, compensate for, or manage abnormalities in metabolic pathways that can arise from genetic conditions, acquired diseases, or lifestyle factors.
In clinical practice, metabolic therapy encompasses several approaches. Dietary modification forms the cornerstone of many interventions, restricting or supplementing specific nutrients to prevent toxic accumulation or deficiency. Enzyme replacement therapy provides missing or deficient enzymes in certain inherited metabolic disorders. Pharmacological treatments may enhance residual enzyme activity, facilitate toxin removal, or modulate metabolic pathways. Vitamin and cofactor supplementation can support enzymatic function in responsive conditions.
The scope of metabolic therapy extends from rare inherited metabolic diseases—such as phenylketonuria (PKU), maple syrup urine disease, and lysosomal storage disorders—to more common conditions including diabetes mellitus, obesity, and dyslipidaemia. In the UK, specialist metabolic medicine services coordinate care for patients with complex metabolic disorders, working within multidisciplinary teams that include metabolic physicians, dietitians, genetic counsellors, and specialist nurses.
Metabolic therapy is highly individualised, with treatment plans tailored to the specific metabolic defect, disease severity, patient age, and response to intervention. Regular biochemical monitoring ensures therapeutic targets are met whilst minimising adverse effects. Early diagnosis and prompt initiation of appropriate metabolic therapy can prevent irreversible complications, particularly neurological damage in inherited metabolic disorders, making the NHS Newborn Blood Spot Screening Programme an essential component of preventive healthcare in the UK.
Conditions Treated with Metabolic Therapy
Metabolic therapy addresses a diverse spectrum of conditions affecting carbohydrate, amino acid, lipid, and complex molecule metabolism. Inherited metabolic disorders (IMDs) represent a significant category, with over 1,000 recognised conditions, though individually rare. Phenylketonuria (PKU) requires lifelong dietary restriction of phenylalanine to prevent intellectual disability, with sapropterin (BH4) available for responsive patients. Galactosaemia necessitates elimination of galactose-containing foods. Organic acidaemias and urea cycle disorders demand protein restriction alongside emergency protocols to prevent metabolic decompensation.
Lysosomal storage disorders, including Gaucher disease, Fabry disease, and mucopolysaccharidoses, may benefit from enzyme replacement therapy (ERT), substrate reduction therapy, or chaperone therapy. These conditions result from deficient lysosomal enzymes, causing progressive accumulation of undegraded substrates in tissues. Mitochondrial disorders affecting energy production may respond to specific cofactor supplementation in selected cases (coenzyme Q10, riboflavin, thiamine), though evidence is limited and treatment remains largely supportive.
Diabetes mellitus—both type 1 and type 2—represents the most prevalent metabolic condition treated in the UK, affecting approximately 4.7 million people according to Diabetes UK. Metabolic therapy includes insulin replacement, oral hypoglycaemic agents, dietary modification, and increasingly, newer agents such as GLP-1 receptor agonists and SGLT2 inhibitors that target specific metabolic pathways, guided by NICE recommendations.
Dyslipidaemia and obesity are managed through lifestyle interventions, statins, fibrates, PCSK9 inhibitors (according to NICE criteria), and in selected cases, bariatric surgery—a metabolic intervention with profound effects on glucose and lipid metabolism. Porphyrias, disorders of haem synthesis, require avoidance of precipitating factors and specific treatments including haem arginate infusions and, for recurrent acute hepatic porphyria, givosiran. The MHRA and NICE provide guidance on appropriate use of metabolic therapies, ensuring evidence-based, safe prescribing across these varied conditions.
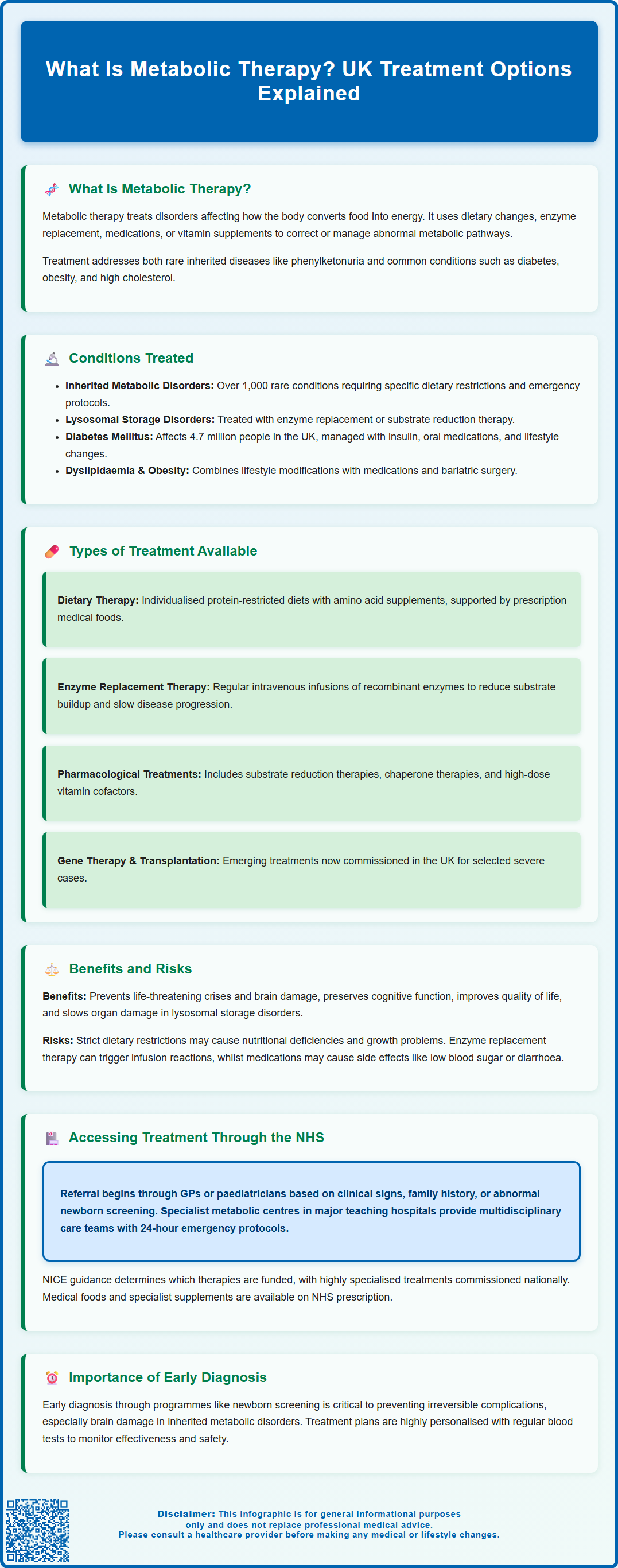
Types of Metabolic Therapy Available in the UK
The UK offers a comprehensive range of metabolic therapies through specialist centres and the NHS. Dietary therapy remains fundamental, delivered by specialist metabolic dietitians who design individualised nutritional plans. For amino acid disorders, this involves protein-restricted diets supplemented with amino acid mixtures lacking the problematic amino acid. Medical foods and low-protein products are available on prescription through the Advisory Committee on Borderline Substances (ACBS) arrangements, supporting adherence to restrictive diets whilst maintaining adequate nutrition.
Enzyme replacement therapy (ERT) has transformed outcomes in several lysosomal storage disorders. Intravenous infusions of recombinant enzymes—such as imiglucerase for Gaucher disease, agalsidase for Fabry disease, and laronidase for mucopolysaccharidosis type I—are administered regularly, with frequency varying by product (weekly or fortnightly) according to the specific MHRA-approved product characteristics. These therapies reduce substrate accumulation and prevent or slow disease progression, though they generally cannot reverse established damage or cross the blood-brain barrier effectively, with exceptions such as intraventricular cerliponase alfa for CLN2 disease.
Pharmacological interventions include substrate reduction therapies (e.g., miglustat and eliglustat for Gaucher disease), chaperone therapies that stabilise mutant enzymes (e.g., migalastat for Fabry disease with amenable mutations), and medications that enhance residual enzyme activity. Cofactor supplementation—including high-dose vitamins such as pyridoxine (vitamin B6), riboflavin (vitamin B2), biotin, and cobalamin (vitamin B12)—can restore or enhance enzyme function in specific vitamin-responsive metabolic disorders.
Gene therapy represents an emerging frontier, with several clinical trials underway for inherited metabolic disorders. Some gene therapies are now commissioned in the UK, such as atidarsagene autotemcel (Libmeldy) for metachromatic leukodystrophy. Haematopoietic stem cell transplantation may be considered for selected severe metabolic disorders, offering potential enzyme replacement through donor cells. Emergency regimens for acute metabolic decompensation include intravenous glucose, specific detoxification protocols, and dialysis when required, coordinated through specialist metabolic units with 24-hour advice lines following British Inherited Metabolic Disease Group (BIMDG) protocols.
Benefits and Risks of Metabolic Therapy
The benefits of metabolic therapy can be life-saving and life-changing, particularly when initiated early. Prevention of acute metabolic crises in conditions such as urea cycle disorders and organic acidaemias reduces mortality and prevents neurological injury. Preservation of cognitive function through dietary management of PKU has enabled generations of affected individuals to lead normal lives—a stark contrast to the inevitable intellectual disability seen before treatment availability.
Improved quality of life is documented across many metabolic conditions. Enzyme replacement therapy reduces pain, improves exercise tolerance, and slows organ damage in lysosomal storage disorders. Effective diabetes management prevents microvascular complications (retinopathy, nephropathy, neuropathy) and reduces macrovascular risk. Symptom control through appropriate metabolic therapy alleviates fatigue, gastrointestinal symptoms, and other manifestations that significantly impact daily functioning.
However, metabolic therapies carry inherent risks and limitations. Dietary restrictions may lead to nutritional deficiencies if not carefully monitored, with risks of inadequate protein, essential fatty acids, vitamins, and minerals. Growth faltering in children requires vigilant nutritional surveillance. Enzyme replacement therapy can provoke infusion reactions ranging from mild (fever, chills) to severe anaphylaxis, necessitating premedication and careful monitoring. Development of neutralising antibodies may reduce treatment efficacy.
Pharmacological interventions carry specific adverse effect profiles. Substrate reduction therapies may cause diarrhoea, weight loss, and peripheral neuropathy. Medications for diabetes include risks of hypoglycaemia (insulin, sulphonylureas), gastrointestinal upset (metformin, GLP-1 agonists), and rarely, diabetic ketoacidosis with SGLT2 inhibitors (which should be temporarily discontinued during acute illness or before surgery). Psychological burden of lifelong dietary restriction, frequent hospital visits, and chronic disease management should not be underestimated. Cost and access issues may arise, particularly for ultra-orphan drugs. Patients should discuss potential benefits and risks with their metabolic team, ensuring informed decision-making and realistic expectations regarding treatment outcomes. Suspected adverse reactions should be reported through the MHRA Yellow Card scheme.
Accessing Metabolic Therapy Through the NHS
Access to metabolic therapy in the UK is coordinated through a network of specialist inherited metabolic disease centres. In England, these centres are designated by NHS England, while Scotland, Wales, and Northern Ireland have their own arrangements. Referral pathways typically begin with general practitioners or paediatricians who suspect a metabolic disorder based on clinical presentation, family history, or abnormal screening results. The NHS Newborn Blood Spot Screening Programme identifies several treatable metabolic conditions, enabling pre-symptomatic diagnosis and immediate referral to specialist services.
Specialist metabolic centres are located in major teaching hospitals across the UK, with paediatric and adult services often co-located to facilitate transition. These centres provide comprehensive multidisciplinary care including metabolic physicians, specialist nurses, dietitians, clinical geneticists, and biochemists. Emergency protocols ensure 24-hour access to specialist advice for patients and healthcare professionals managing acute metabolic decompensation, with clear pathways for hospital admission when required, following British Inherited Metabolic Disease Group (BIMDG) guidelines.
NICE guidance informs commissioning decisions for metabolic therapies, evaluating clinical effectiveness and cost-effectiveness. Highly specialised services, including enzyme replacement therapies and complex dietary management, are commissioned nationally through Highly Specialised Services arrangements, ensuring equitable access. Individual Funding Requests (IFRs) are reserved for exceptional cases that fall outside established commissioning policies.
Prescription support ensures patients receive necessary medical foods, low-protein products, and specialist supplements on NHS prescription, though availability may vary between regions. Patient organisations such as Metabolic Support UK and the British Inherited Metabolic Disease Group (BIMDG) provide valuable information, support networks, and advocacy. Transition services facilitate transfer from paediatric to adult care, addressing the specific needs of adolescents and young adults with lifelong metabolic conditions. Patients experiencing difficulties accessing appropriate metabolic therapy should discuss concerns with their specialist team or seek support through patient advocacy organisations and NHS complaints procedures.
Frequently Asked Questions
Who needs metabolic therapy in the UK?
Metabolic therapy is required for patients with inherited metabolic disorders such as phenylketonuria, lysosomal storage diseases, and mitochondrial conditions, as well as those with common metabolic conditions including diabetes mellitus, obesity, and dyslipidaemia. Specialist metabolic centres coordinate care through multidisciplinary teams across the NHS.
How do I access metabolic therapy through the NHS?
Access begins with referral from your GP or paediatrician to specialist inherited metabolic disease centres designated by NHS England. The NHS Newborn Blood Spot Screening Programme identifies several treatable conditions at birth, enabling immediate specialist referral and treatment initiation.
What are the main types of metabolic therapy available?
Main types include dietary therapy with specialist medical foods, enzyme replacement therapy for lysosomal storage disorders, pharmacological interventions such as substrate reduction therapies, vitamin and cofactor supplementation, and emerging treatments including gene therapy. Treatment is individualised based on the specific metabolic defect and patient response.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript