Is obesity a metabolic disease? This question reflects a fundamental shift in how obesity is understood within UK healthcare. Obesity is now recognised by NICE and NHS England as a complex, chronic medical condition—not simply a lifestyle choice. It involves profound metabolic disturbances including insulin resistance, dyslipidaemia, and chronic inflammation, which collectively increase the risk of type 2 diabetes, cardiovascular disease, and metabolic dysfunction-associated steatotic liver disease. Understanding obesity as a metabolic disease has important implications for diagnosis, treatment, and how patients are supported in achieving sustainable health improvements.
Summary: Obesity is increasingly recognised as a chronic metabolic disease characterised by insulin resistance, hormonal dysregulation, and systemic inflammation that drive conditions such as type 2 diabetes and cardiovascular disease.
- NICE guidance (CG189) classifies obesity as a chronic disease requiring long-term medical management, not merely a behavioural issue.
- Obesity causes insulin resistance, dyslipidaemia, and chronic low-grade inflammation, particularly from visceral adipose tissue.
- Approximately 90% of individuals with type 2 diabetes in the UK are overweight or obese, reflecting the strong metabolic link.
- Treatment options include lifestyle modification, pharmacotherapy (orlistat, GLP-1 receptor agonists), and bariatric surgery for eligible patients.
- NHS tiered services provide structured weight management from primary care advice through to specialist multidisciplinary intervention and surgery.
- Regular monitoring of blood pressure, lipids, and glucose is essential; patients should contact their GP for symptoms of metabolic complications.
Table of Contents
What Is Obesity and How Is It Defined in the UK?
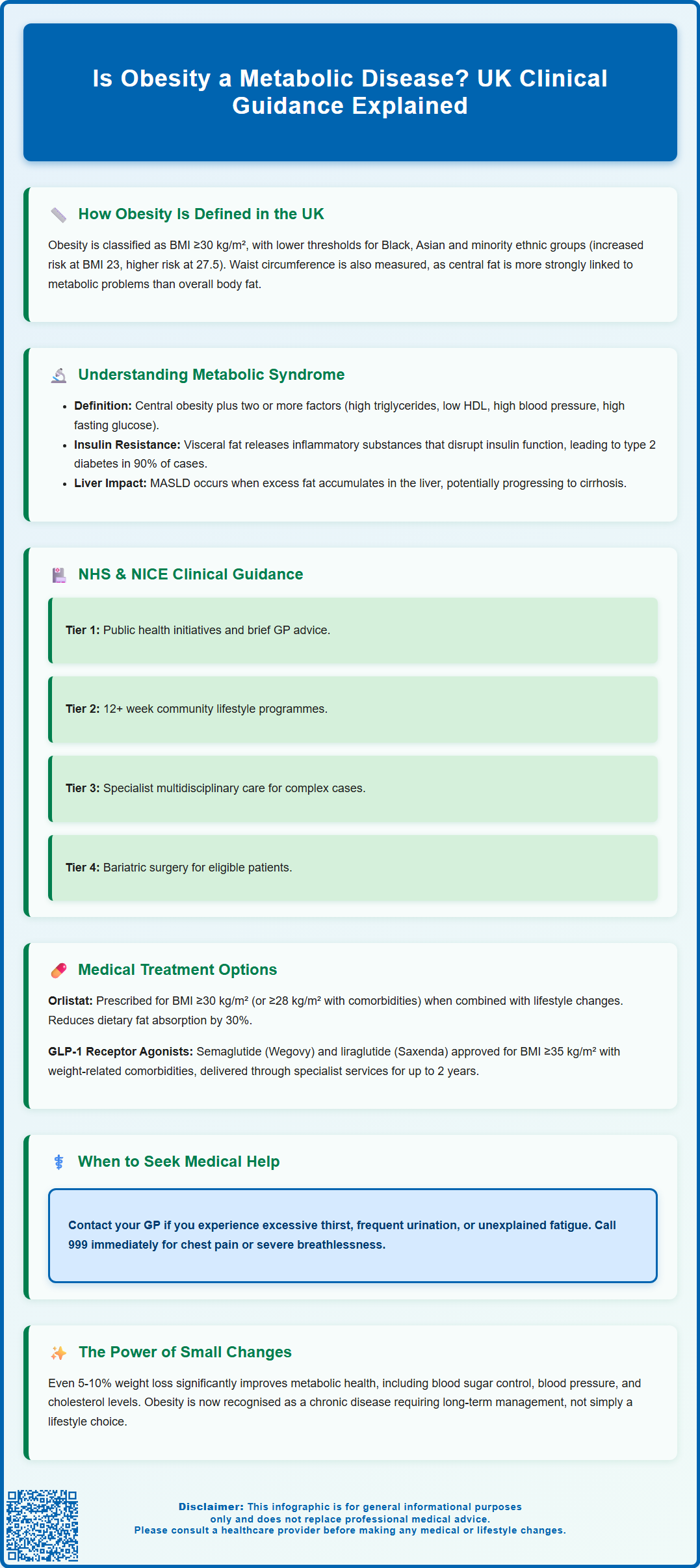
Obesity is formally defined in the UK as an abnormal or excessive accumulation of body fat that presents a risk to health. The most widely used measure is body mass index (BMI), calculated by dividing a person's weight in kilograms by the square of their height in metres. According to NHS and NICE criteria, a BMI of 30 kg/m² or above indicates obesity, whilst a BMI between 25 and 29.9 kg/m² is classified as overweight. For people from Black, Asian and other minority ethnic groups, NICE guidance (PH46) recommends lower BMI thresholds for intervention due to increased health risks at lower BMI values—with increased risk beginning at BMI 23 kg/m² and higher risk at 27.5 kg/m² for these populations.
Whilst BMI remains the standard screening tool in clinical practice, it has recognised limitations. It does not distinguish between muscle and fat mass, nor does it account for fat distribution. Waist circumference is therefore used as an additional measure, as central (abdominal) adiposity is more strongly associated with metabolic complications. For the general population, men with a waist circumference above 94 cm and women above 80 cm are at increased health risk, with very high risk thresholds set at 102 cm and 88 cm respectively. For South Asian men, risk is increased at a lower threshold of 90 cm, while for South Asian women it remains at 80 cm.
Obesity is now understood not simply as a lifestyle issue but as a complex, chronic medical condition influenced by genetic, environmental, psychological, and physiological factors. This shift in understanding has important implications for how obesity is managed within the NHS and how patients are supported in achieving sustainable weight management.
The Link Between Obesity and Metabolic Disorders
Obesity is strongly associated with a cluster of metabolic abnormalities collectively known as metabolic syndrome. According to International Diabetes Federation criteria, this syndrome is diagnosed when central obesity (defined by waist circumference) is present alongside at least two of the following: raised triglycerides, reduced HDL cholesterol, raised blood pressure, or raised fasting plasma glucose. When these factors coexist, they significantly increase the risk of developing type 2 diabetes, cardiovascular disease, and stroke. The underlying mechanism involves chronic low-grade inflammation and hormonal dysregulation caused by excess adipose tissue, particularly visceral fat surrounding internal organs.
Insulin resistance is a hallmark feature linking obesity to metabolic disease. Adipose tissue, especially visceral fat, secretes inflammatory cytokines and free fatty acids that interfere with insulin signalling in muscle, liver, and fat cells. This forces the pancreas to produce more insulin to maintain normal blood glucose levels. Over time, pancreatic beta cells may become exhausted, leading to impaired glucose tolerance and eventually type 2 diabetes. According to Diabetes UK, approximately 90% of individuals with type 2 diabetes are overweight or obese.
Obesity also disrupts lipid metabolism, typically resulting in elevated triglycerides, reduced high-density lipoprotein (HDL) cholesterol, and an atherogenic lipid profile. Excess adipose tissue produces hormones such as leptin and adiponectin in abnormal quantities, further contributing to metabolic dysfunction. Metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease (NAFLD), is another metabolic consequence of obesity, potentially progressing to cirrhosis and liver failure. NICE guidance (NG49) recognises this condition as increasingly common in the UK, affecting people with obesity and metabolic risk factors.
These interconnected metabolic disturbances explain why obesity is increasingly recognised not merely as a risk factor but as a metabolic disease in its own right, requiring comprehensive medical management.
NHS and NICE Guidance on Obesity as a Medical Condition
NICE guidance (CG189) explicitly recognises obesity as a chronic disease requiring long-term management rather than short-term intervention. This represents a significant shift from viewing obesity purely as a behavioural problem. The guidance emphasises that obesity results from complex interactions between genetic predisposition, environmental factors, psychological influences, and physiological mechanisms that regulate appetite and energy expenditure.
NHS England and Public Health England have developed a tiered approach to obesity management within the NHS. Tier 1 involves universal public health interventions and brief advice in primary care. Tier 2 comprises lifestyle weight management programmes delivered in community settings, typically offering dietary advice, physical activity support, and behavioural change techniques over 12 weeks or more. Tier 3 services provide specialist multidisciplinary assessment and intervention for individuals with complex obesity, often including psychological support, dietetic input, and consideration of pharmacological or surgical options. Tier 4 represents bariatric surgery services.
The NHS Long Term Plan commits to expanding access to weight management services, particularly for individuals with obesity-related complications such as type 2 diabetes or cardiovascular disease. GPs are encouraged to raise the topic of weight sensitively, using non-stigmatising language and recognising that many patients have attempted weight loss multiple times. Assessment should include measurement of BMI and waist circumference, evaluation of comorbidities, and discussion of realistic goals.
NICE also provides specific guidance on pharmacological treatments. Orlistat may be considered as an option for adults with a BMI of 30 kg/m² or above (or 28 kg/m² with comorbidities), provided it is used alongside lifestyle interventions. More recently, GLP-1 receptor agonists have been approved for weight management in specific circumstances. NICE technology appraisal (TA875) recommends semaglutide (Wegovy) for adults with at least one weight-related comorbidity and a BMI of at least 35 kg/m² (or 30 kg/m² in exceptional circumstances), delivered through specialist weight management services for a maximum of 2 years. Similarly, liraglutide (Saxenda) is recommended under specific criteria (TA664). These approvals reflect growing recognition of obesity as a condition requiring medical treatment.
Treatment Approaches for Obesity-Related Metabolic Problems
Management of obesity-related metabolic disorders requires an integrated approach addressing both weight reduction and specific metabolic abnormalities. Lifestyle modification remains the foundation of treatment, with evidence showing that even modest weight loss of 5-10% can produce significant metabolic benefits, including improved glycaemic control, reduced blood pressure, and favourable changes in lipid profiles.
For individuals with type 2 diabetes and obesity, NICE recommends considering weight loss as a primary therapeutic target. Structured education programmes such as DESMOND (Diabetes Education and Self-Management for Ongoing and Newly Diagnosed) incorporate weight management strategies. Certain diabetes medications offer additional weight loss benefits—metformin typically causes modest weight reduction, whilst GLP-1 receptor agonists (such as liraglutide, semaglutide, or dulaglutide) promote substantial weight loss alongside glucose-lowering effects by enhancing satiety and slowing gastric emptying. Common side effects of GLP-1 receptor agonists include nausea, vomiting and diarrhoea, particularly during dose escalation. Conversely, some diabetes treatments including insulin, sulphonylureas, and thiazolidinediones may cause weight gain and should be used judiciously.
Pharmacological interventions specifically for weight management include orlistat, which inhibits pancreatic lipase to reduce dietary fat absorption by approximately 30%. Common adverse effects include gastrointestinal symptoms such as oily stools, faecal urgency, and flatulence, which can be minimised by reducing dietary fat intake. Semaglutide (Wegovy) 2.4 mg weekly is available through specialist NHS weight management services for eligible adults with a BMI ≥35 kg/m² (or ≥30 kg/m² in exceptional circumstances) and at least one weight-related comorbidity, for a maximum of 2 years. Clinical trials have demonstrated average weight loss of 10-15% with this treatment.
Bariatric surgery represents the most effective intervention for severe obesity. NICE recommends considering bariatric surgery as a first-line option (alongside lifestyle interventions) for adults with a BMI of 50 kg/m² or above. For those with a BMI of 40 kg/m² or above, or 35-39.9 kg/m² with significant comorbidities, bariatric surgery is recommended when other interventions have not achieved or maintained adequate weight loss. For people with recent-onset type 2 diabetes and a BMI of 30-34.9 kg/m², NICE recommends considering an assessment for bariatric surgery. Procedures such as gastric bypass and sleeve gastrectomy produce substantial, sustained weight loss and often result in remission or significant improvement of type 2 diabetes, hypertension, and dyslipidaemia.
Patients should be advised to contact their GP if they experience symptoms suggesting metabolic complications, including excessive thirst, frequent urination, unexplained fatigue, or cardiovascular symptoms. For chest pain or severe breathlessness, patients should call 999 immediately. Regular monitoring of blood pressure, lipids, and glucose is essential for individuals with obesity, particularly those with established metabolic disorders. Patients should report any suspected side effects from medications to their healthcare professional or directly to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk). A multidisciplinary approach involving dietitians, specialist nurses, psychologists, and physicians offers the best outcomes for managing obesity as a chronic metabolic disease.
Frequently Asked Questions
Does the NHS recognise obesity as a disease?
Yes, NICE guidance (CG189) and NHS England explicitly recognise obesity as a chronic disease requiring long-term medical management, not simply a lifestyle issue. This reflects understanding of obesity as a complex condition involving genetic, environmental, psychological, and physiological factors.
What metabolic problems are caused by obesity?
Obesity causes insulin resistance, type 2 diabetes, dyslipidaemia (abnormal cholesterol and triglycerides), hypertension, metabolic syndrome, and metabolic dysfunction-associated steatotic liver disease (MASLD). These result from chronic inflammation and hormonal dysregulation caused by excess adipose tissue, particularly visceral fat.
What treatments are available on the NHS for obesity-related metabolic disease?
NHS treatment includes tiered lifestyle interventions, pharmacotherapy (orlistat, GLP-1 receptor agonists such as semaglutide for eligible patients), and bariatric surgery for those meeting NICE criteria. Management also addresses specific metabolic complications such as type 2 diabetes and hypertension through medication and monitoring.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












