What is a metabolic imbalance? A metabolic imbalance occurs when the body's biochemical processes that convert food into energy and maintain cellular function become disrupted. Rather than a single diagnosis, this umbrella term encompasses various conditions affecting metabolic pathways, from glucose regulation to electrolyte balance. These disturbances can range from mild, symptom-free abnormalities to serious conditions such as diabetes mellitus, thyroid disorders, and metabolic syndrome. Understanding metabolic imbalances is essential, as early recognition and appropriate management can prevent complications affecting cardiovascular health, neurological function, and overall quality of life. This article explores the causes, symptoms, diagnosis, and evidence-based treatment approaches for metabolic imbalances.
Summary: A metabolic imbalance is a disruption in the body's normal biochemical processes that convert food into energy and maintain cellular function, encompassing conditions affecting glucose regulation, lipid metabolism, electrolyte balance, and hormone function.
- Metabolic imbalances affect carbohydrate, lipid, protein metabolism, electrolyte balance, and acid-base homeostasis through dysregulation of enzymes and hormones.
- Common causes include endocrine disorders (thyroid dysfunction, diabetes), genetic factors, medications (corticosteroids, antipsychotics), and lifestyle factors such as poor diet and physical inactivity.
- Symptoms vary but may include persistent fatigue, unexplained weight changes, increased thirst and urination, temperature intolerance, and cognitive changes.
- Diagnosis combines clinical assessment with laboratory investigations including fasting glucose or HbA1c, lipid profile, thyroid function tests, and renal function tests.
- Treatment involves lifestyle modifications (dietary changes, physical activity) alongside pharmacological management such as metformin for diabetes or statins for dyslipidaemia, guided by NICE protocols.
- Seek urgent medical attention for severe confusion, rapid breathing, persistent vomiting, or chest pain, which may indicate acute metabolic decompensation requiring emergency treatment.
Table of Contents
What Is a Metabolic Imbalance?
A metabolic imbalance refers to a disruption in the body's normal biochemical processes that convert food into energy and maintain cellular function. This is an umbrella term rather than a specific diagnosis, encompassing various conditions affecting metabolic pathways. Metabolism encompasses thousands of chemical reactions occurring continuously within cells, regulated by enzymes, hormones, and various organ systems. When these processes become dysregulated, the body may struggle to maintain homeostasis—the stable internal environment necessary for optimal health.
Metabolic imbalances can affect multiple systems simultaneously, as metabolism is fundamental to every bodily function. These disturbances may involve abnormalities in glucose regulation, lipid metabolism, protein synthesis, electrolyte balance, or acid-base homeostasis. The endocrine system, particularly the thyroid gland, pancreas, and adrenal glands, plays a crucial role in metabolic regulation through hormone secretion.
Key metabolic processes that may become imbalanced include:
-
Carbohydrate metabolism (glucose regulation)
-
Lipid metabolism (cholesterol and triglyceride processing)
-
Protein metabolism (amino acid utilisation)
-
Electrolyte balance (sodium, potassium, calcium levels)
-
Acid-base balance (pH regulation)
The severity of metabolic imbalances varies considerably. Some individuals experience mild disturbances with minimal symptoms, whilst others develop serious conditions requiring immediate medical intervention. Common examples include diabetes mellitus, thyroid disorders (hypothyroidism or hyperthyroidism), and metabolic syndrome. Understanding these disturbances is essential for early recognition and appropriate management, as untreated metabolic imbalances can lead to complications affecting cardiovascular health, neurological function, and overall quality of life.
Common Causes of Metabolic Imbalances
Metabolic imbalances arise from diverse aetiologies, ranging from genetic predisposition to lifestyle factors and underlying medical conditions. Endocrine disorders represent a primary cause, with thyroid dysfunction (hypothyroidism or hyperthyroidism) affecting metabolic rate, and pancreatic disorders disrupting insulin production and glucose homeostasis. Diabetes mellitus, both type 1 and type 2, exemplifies how impaired insulin function creates widespread metabolic disturbances affecting carbohydrate, protein, and lipid metabolism.
Genetic and congenital factors contribute significantly to metabolic imbalances. Inherited metabolic disorders, though individually rare, collectively affect a substantial number of individuals. These conditions involve enzyme deficiencies that impair specific metabolic pathways. Familial hypercholesterolaemia affects lipid metabolism and requires specific management as outlined in NICE CG71, whilst phenylketonuria disrupts amino acid processing. Genetic predisposition also influences susceptibility to conditions like metabolic syndrome and type 2 diabetes.
Lifestyle and environmental factors play an increasingly recognised role in metabolic health. Poor dietary habits, particularly excessive consumption of refined carbohydrates and saturated fats, contribute to insulin resistance and dyslipidaemia. Physical inactivity reduces metabolic efficiency and promotes weight gain, creating a cycle that further impairs metabolic function. Chronic stress elevates cortisol levels, which can disrupt glucose metabolism and promote central adiposity.
Additional causes include:
-
Medications (corticosteroids, second-generation antipsychotics, some beta-blockers, thiazide diuretics, antiretrovirals)
-
Chronic kidney or liver disease affecting metabolic processing
-
Hormonal changes during pregnancy or menopause
-
Polycystic ovary syndrome (PCOS)
-
Cushing's syndrome or Addison's disease
-
Haemochromatosis (iron overload)
-
Alcohol misuse
-
Malnutrition or eating disorders
-
Chronic inflammatory conditions
-
Sleep disorders, particularly obstructive sleep apnoea
Understanding these varied causes enables healthcare professionals to identify at-risk individuals and implement preventative strategies where possible.
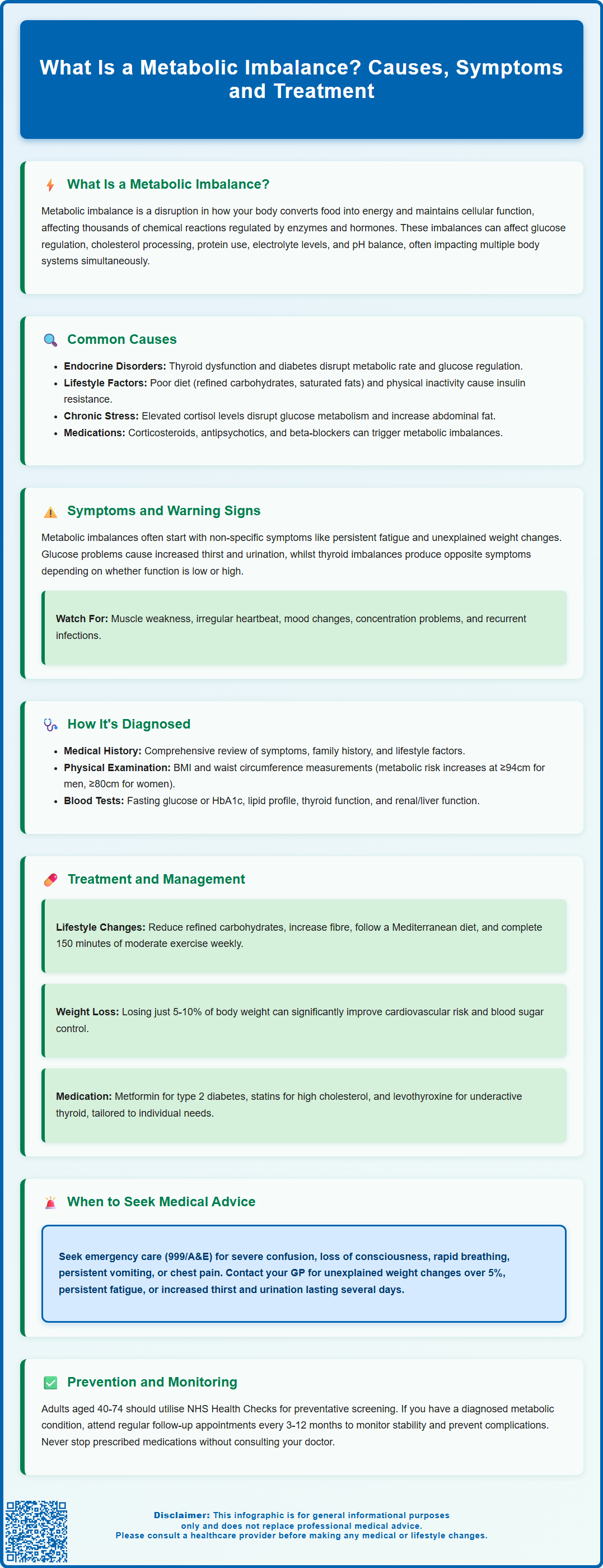
Symptoms and Warning Signs to Watch For
The clinical presentation of metabolic imbalances varies considerably depending on the specific disturbance, its severity, and duration. Many individuals experience non-specific symptoms initially, which can delay diagnosis. Persistent fatigue represents one of the most common complaints, often accompanied by unexplained changes in body weight—either gain or loss—despite stable dietary habits. These symptoms reflect the body's impaired ability to efficiently process nutrients and generate cellular energy.
Glucose metabolism disturbances produce characteristic symptoms that warrant particular attention. Increased thirst (polydipsia) and frequent urination (polyuria) suggest hyperglycaemia, whilst episodes of shakiness, sweating, confusion, or palpitations may indicate hypoglycaemia. Individuals may notice increased hunger despite adequate food intake, or conversely, loss of appetite. Blurred vision can occur with significant blood glucose fluctuations, and slow wound healing may indicate prolonged metabolic dysfunction.
Thyroid-related metabolic imbalances present distinctively. Hypothyroidism typically causes cold intolerance, constipation, dry skin, hair loss, and cognitive slowing. Conversely, hyperthyroidism produces heat intolerance, increased sweating, tremor, anxiety, and unexplained weight loss despite increased appetite. Both conditions may cause menstrual irregularities in women.
Additional warning signs include:
-
Persistent muscle weakness or cramps
-
Irregular heartbeat or palpitations
-
Mood changes, including depression or irritability
-
Difficulty concentrating or memory problems
-
Excessive thirst or changes in urination patterns
-
Unexplained skin changes or darkening (acanthosis nigricans)
-
Recurrent infections
-
Sudden confusion, seizures, or profound muscle weakness (may indicate acute electrolyte or acid-base disturbances requiring urgent assessment)
It is important to note that symptoms often develop gradually, and individuals may attribute them to stress, ageing, or other factors. However, the presence of multiple symptoms, particularly if progressive, warrants medical evaluation to identify potential metabolic disturbances before complications develop.
How Metabolic Imbalances Are Diagnosed
Diagnosing metabolic imbalances requires a systematic approach combining clinical assessment with targeted investigations. The process typically begins with a comprehensive medical history exploring symptom onset, duration, and progression, alongside family history of metabolic or endocrine disorders. Healthcare professionals assess lifestyle factors including diet, physical activity, alcohol consumption, and medication use. A thorough physical examination evaluates vital signs, body mass index (BMI), waist circumference (with increased metabolic risk at ≥94cm for men and ≥80cm for women of European descent), and signs of specific metabolic disorders such as thyroid enlargement or skin changes.
Laboratory investigations form the cornerstone of metabolic assessment. Blood tests provide crucial information about various metabolic parameters. A fasting glucose test or HbA1c measurement evaluates glucose metabolism and diabetes risk. In the UK, diabetes is diagnosed at HbA1c ≥48 mmol/mol (6.5%), while values of 42-47 mmol/mol (6.0-6.4%) indicate non-diabetic hyperglycaemia (pre-diabetes). The lipid profile assesses total cholesterol, LDL-cholesterol, HDL-cholesterol, and triglycerides, identifying dyslipidaemia. Thyroid function tests (TSH, free T4, and sometimes free T3) detect thyroid disorders affecting metabolic rate.
Common investigations may include:
-
Renal function tests (urea, creatinine, eGFR) and electrolytes
-
Liver function tests to assess hepatic metabolic capacity
-
Urinalysis to detect glucose, ketones, or protein
Additional targeted tests when clinically indicated:
-
Vitamin D testing (for those at risk of deficiency, not as routine screening)
-
Vitamin B12 levels (when deficiency is suspected based on symptoms or risk factors)
-
Cortisol measurements if Cushing's syndrome is suspected
-
Insulin and C-peptide levels in specific circumstances (specialist tests)
Specialised testing may be warranted for complex cases. Oral glucose tolerance tests provide detailed information about glucose handling. Continuous glucose monitoring offers insights into glycaemic patterns in selected patients. Genetic testing may be considered when inherited metabolic disorders are suspected, particularly in younger patients or those with family history.
The diagnostic approach is individualised based on clinical presentation. Healthcare professionals interpret results within the clinical context, as isolated abnormalities may not always indicate significant metabolic dysfunction. Serial measurements often prove more informative than single values, particularly for monitoring treatment response or disease progression.
Treatment Options and Management Strategies
Managing metabolic imbalances requires a personalised, multifaceted approach addressing underlying causes whilst optimising metabolic function. Treatment strategies typically combine lifestyle modifications with pharmacological interventions when necessary, guided by evidence-based protocols.
Lifestyle interventions form the foundation of metabolic management. Dietary modification tailored to the specific imbalance is essential—individuals with insulin resistance benefit from reduced refined carbohydrate intake and increased fibre consumption, whilst those with dyslipidaemia require reduced saturated fat intake. The Mediterranean dietary pattern demonstrates robust evidence for improving metabolic health. Regular physical activity enhances insulin sensitivity, improves lipid profiles, and supports weight management. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity weekly for adults, plus muscle-strengthening activities on at least two days per week.
Weight management, when appropriate, significantly improves metabolic parameters. Even modest weight loss (5-10% of body weight) can substantially reduce cardiovascular risk and improve glucose control in individuals with metabolic syndrome or type 2 diabetes.
Pharmacological management targets specific metabolic disturbances:
-
Diabetes management: According to NICE guidance (NG28), metformin is typically first-line for type 2 diabetes, improving insulin sensitivity. However, SGLT2 inhibitors may be considered first-line in people with high cardiovascular risk, established cardiovascular disease, or chronic kidney disease. Additional agents (GLP-1 receptor agonists, DPP-4 inhibitors) may be added based on individual circumstances and risk factors.
-
Lipid management: Following NICE guidance (NG238), statins (typically atorvastatin) are recommended based on QRISK3 assessment. Ezetimibe, PCSK9 inhibitors, or bempedoic acid may be considered for those meeting specific criteria.
-
Thyroid disorders: Levothyroxine replacement for hypothyroidism; antithyroid medications or radioiodine for hyperthyroidism, as outlined in NICE NG145.
Monitoring and follow-up are crucial. Regular review of metabolic parameters, medication adherence, and lifestyle implementation ensures treatment effectiveness. Healthcare professionals adjust management strategies based on response, tolerability, and changing circumstances. Patient education empowers individuals to actively participate in their care, understanding their condition and recognising when adjustments are needed.
Patients taking medications should be aware of 'sick day rules' (e.g., temporarily stopping SGLT2 inhibitors during acute illness or metformin during significant dehydration). Any suspected side effects should be reported to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Multidisciplinary involvement, including dietitians, diabetes specialist nurses, and endocrinologists, optimises outcomes for complex metabolic disorders.
When to Seek Medical Advice
Recognising when to seek medical attention for potential metabolic imbalances is crucial for preventing complications and ensuring timely intervention. Individuals should contact their GP if they experience persistent or progressive symptoms suggestive of metabolic dysfunction, particularly when multiple symptoms occur simultaneously or significantly impact daily functioning.
Urgent medical attention is warranted for certain presentations indicating acute metabolic decompensation. Seek immediate help (call 999 or attend A&E) if experiencing:
-
Severe confusion, drowsiness, or loss of consciousness
-
Rapid breathing or difficulty breathing
-
Persistent vomiting preventing fluid intake
-
Severe abdominal pain
-
Chest pain or severe palpitations
-
Signs of severe dehydration
These symptoms may indicate diabetic ketoacidosis, hyperosmolar hyperglycaemic state, severe hypoglycaemia, or thyroid storm—all requiring emergency treatment.
For urgent but non-life-threatening concerns, contact NHS 111 for advice.
Routine GP consultation is appropriate for:
-
Unexplained weight changes (gain or loss) exceeding 5% of body weight over 6-12 months
-
Persistent fatigue affecting daily activities despite adequate rest
-
Increased thirst and urination lasting more than a few days
-
New or worsening symptoms in individuals with known metabolic conditions
-
Family history of metabolic disorders with concerning symptoms
-
Difficulty managing diagnosed metabolic conditions despite treatment adherence
Preventative screening should be considered for at-risk individuals. The NHS Health Check, offered to adults aged 40-74 without pre-existing conditions, screens for cardiovascular disease, diabetes, kidney disease, and stroke risk. Those with risk factors—including obesity, family history of diabetes or cardiovascular disease, previous gestational diabetes, or certain ethnic backgrounds—may benefit from earlier or more frequent screening.
Individuals already diagnosed with metabolic conditions should maintain regular follow-up appointments as recommended by their healthcare team, typically ranging from three to twelve months depending on condition stability. Never discontinue prescribed medications without medical consultation, as this may precipitate metabolic decompensation. If experiencing medication side effects or concerns about treatment, discuss these promptly with your GP or specialist rather than stopping treatment independently.
Frequently Asked Questions
What are the most common symptoms of a metabolic imbalance?
Common symptoms include persistent fatigue, unexplained weight changes, increased thirst and frequent urination, temperature intolerance, muscle weakness, mood changes, and difficulty concentrating. Symptoms vary depending on the specific metabolic disturbance and may develop gradually over time.
Can lifestyle changes alone correct a metabolic imbalance?
For some individuals, particularly those with early-stage metabolic syndrome or pre-diabetes, lifestyle modifications including dietary changes, regular physical activity, and weight management can significantly improve metabolic parameters. However, many conditions require pharmacological treatment alongside lifestyle interventions, guided by healthcare professionals.
How is a metabolic imbalance diagnosed by a GP?
Diagnosis involves a comprehensive medical history, physical examination, and blood tests including fasting glucose or HbA1c, lipid profile, thyroid function tests, and renal function tests. Additional investigations may be ordered based on clinical presentation, with results interpreted within the individual's clinical context.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript