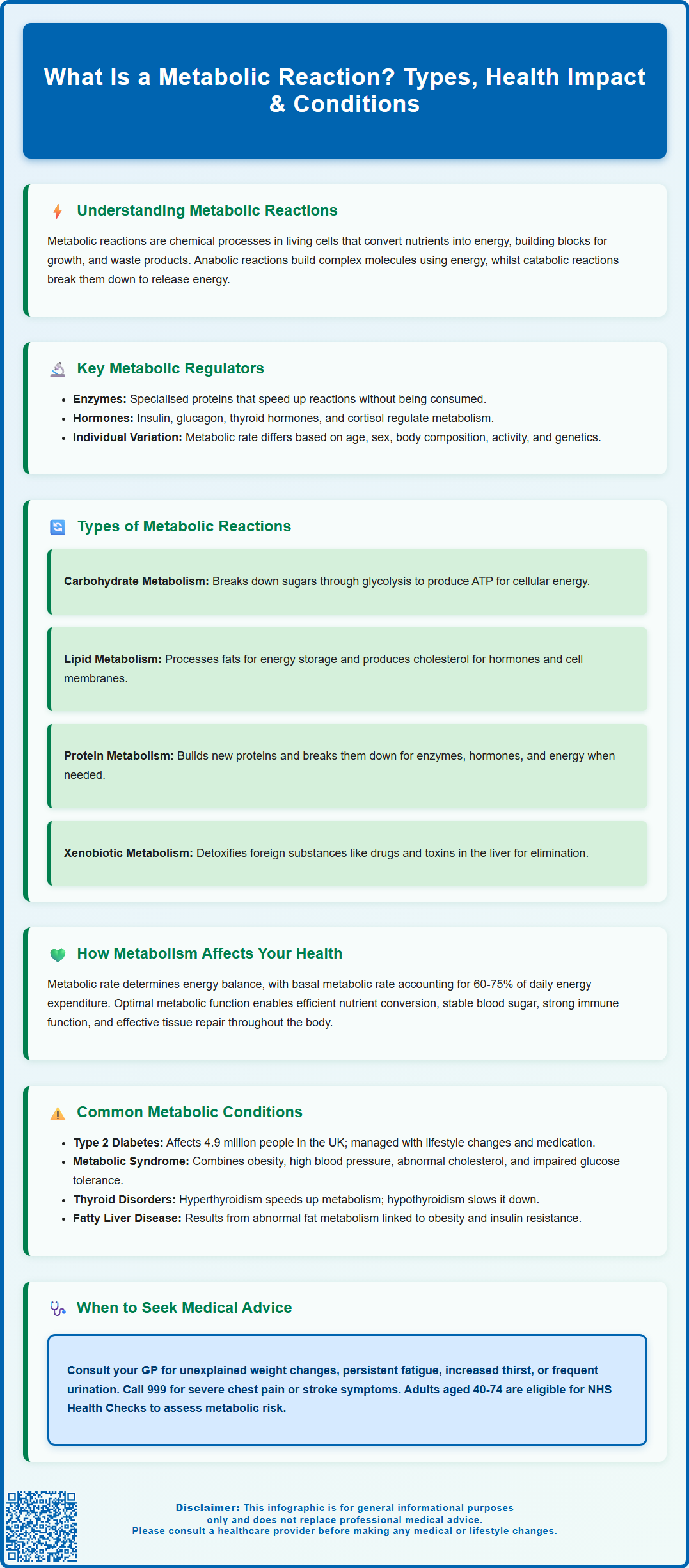
A metabolic reaction is any chemical process occurring within living cells to sustain life. These reactions, collectively termed metabolism, convert nutrients into energy, synthesise essential molecules for growth and repair, and eliminate waste products. Metabolic reactions underpin every bodily function—from breathing and digestion to immune defence and tissue regeneration. They are categorised as anabolic (building complex molecules) or catabolic (breaking down molecules for energy), facilitated by enzymes and regulated by hormones such as insulin and thyroid hormones. Understanding metabolic reactions is fundamental to comprehending health, disease, and how the body maintains balance.
Summary: A metabolic reaction is a chemical process within living cells that converts nutrients into energy, builds essential molecules, and eliminates waste to maintain life.
- Metabolic reactions are categorised as anabolic (building molecules) or catabolic (breaking down molecules for energy).
- Enzymes act as biological catalysts, accelerating metabolic reactions without being consumed.
- Hormones such as insulin, glucagon, and thyroid hormones regulate metabolic reaction rates.
- Disrupted metabolic reactions contribute to conditions including type 2 diabetes, thyroid disorders, and metabolic syndrome.
- Unexplained weight changes, persistent fatigue, or cardiovascular symptoms warrant GP consultation for metabolic assessment.
Table of Contents
What Is a Metabolic Reaction?
A metabolic reaction refers to any chemical process that occurs within living cells to maintain life. These reactions are collectively known as metabolism, which encompasses all the biochemical transformations that convert nutrients from food into energy, building blocks for growth, and waste products for elimination. Metabolic reactions are fundamental to every physiological function, from breathing and digestion to tissue repair and immune responses.
Metabolic reactions can be broadly categorised into two main types: anabolic reactions (building up) and catabolic reactions (breaking down). Anabolic reactions require energy to construct complex molecules from simpler ones, such as synthesising proteins from amino acids or storing glucose as glycogen. Conversely, catabolic reactions release energy by breaking down complex molecules into simpler components, such as converting glucose into carbon dioxide and water during cellular respiration.
These reactions are facilitated by enzymes, which are primarily specialised proteins that act as biological catalysts (though some catalytic RNA molecules called ribozymes also exist). Enzymes accelerate metabolic reactions without being consumed in the process, ensuring that essential biochemical processes occur at rates compatible with life. Each enzyme is highly specific, typically catalysing only one type of reaction or acting on a particular substrate.
Metabolic reactions occur continuously throughout the body, regulated by hormones such as insulin, glucagon, thyroid hormones, cortisol, catecholamines and growth hormone. The rate of metabolism varies between individuals and is influenced by factors including age, sex, body composition, physical activity levels, and genetic factors. Understanding metabolic reactions is essential for comprehending how the body maintains homeostasis and responds to nutritional, environmental, and pathological challenges.
Types of Metabolic Reactions in the Body
Metabolic reactions are organised into interconnected pathways that can be classified according to their function and the molecules they process. Carbohydrate metabolism involves the breakdown of sugars and starches to produce energy. The most important pathway is glycolysis, which converts glucose into pyruvate, generating adenosine triphosphate (ATP)—the cell's primary energy currency. Under aerobic conditions, pyruvate enters the citric acid cycle (Krebs cycle) and electron transport chain within mitochondria, producing substantial amounts of ATP.
Lipid metabolism encompasses the synthesis and breakdown of fats. Lipolysis breaks down triglycerides into fatty acids and glycerol, which can be oxidised for energy through beta-oxidation. Conversely, lipogenesis constructs fatty acids and triglycerides for energy storage. Cholesterol metabolism is also crucial, as cholesterol serves as a precursor for steroid hormones, bile acids, and vitamin D, whilst also forming an essential component of cell membranes.
Protein metabolism involves the synthesis of new proteins from amino acids (protein synthesis) and the breakdown of proteins into amino acids (proteolysis). Amino acids can be used to build structural proteins, enzymes, hormones, and antibodies. When required, amino acids can also be converted into glucose through gluconeogenesis or oxidised for energy, with nitrogen waste being converted to urea in the liver for excretion by the kidneys.
Nucleotide metabolism governs the synthesis and degradation of DNA and RNA components. These pathways are essential for cell division, genetic information storage, and cellular signalling. Additionally, xenobiotic metabolism processes foreign substances, including medications and environmental toxins, primarily in the liver through phase I reactions (such as oxidation by cytochrome P450 enzymes) and phase II reactions (such as glucuronidation), rendering them more water-soluble for elimination.
How Metabolic Reactions Affect Health
Metabolic reactions directly influence overall health, energy levels, body weight, and susceptibility to disease. When metabolic processes function optimally, the body efficiently converts nutrients into energy, maintains stable blood glucose levels, supports immune function, and repairs damaged tissues. Disruptions to metabolic reactions, however, can have wide-ranging health consequences.
Energy balance is fundamentally determined by metabolic rate—the speed at which the body converts food into energy. Basal metabolic rate (BMR) accounts for approximately 60–75% of total daily energy expenditure and represents the energy required for essential functions at rest, including breathing, circulation, and cellular maintenance. Factors that increase metabolic rate include physical activity, muscle mass, fever, hyperthyroidism, and certain medications, whilst ageing, prolonged calorie restriction, and hypothyroidism tend to decrease it.
Metabolic reactions also regulate blood glucose homeostasis, which is critical for preventing both hypoglycaemia (low blood sugar) and hyperglycaemia (high blood sugar). Insulin promotes glucose uptake into cells and stimulates glycogen synthesis, whilst glucagon triggers glycogen breakdown and glucose release. Dysregulation of these processes contributes to conditions such as diabetes mellitus.
Lipid metabolism affects cardiovascular health through its influence on blood lipid levels and atherosclerosis risk. Abnormal lipid metabolism can lead to dyslipidaemia, characterised by elevated non-HDL cholesterol (including low-density lipoprotein or LDL), reduced high-density lipoprotein (HDL) cholesterol, or elevated triglycerides—all independent risk factors for coronary heart disease and stroke. UK clinical practice focuses particularly on non-HDL cholesterol as a primary metric for cardiovascular risk assessment.
Furthermore, metabolic reactions influence body composition and weight management. Imbalances between energy intake and expenditure, coupled with metabolic inefficiencies, contribute to obesity, which itself further disrupts metabolic function, creating a cycle that increases risk for numerous chronic diseases.
Common Conditions Linked to Metabolic Reactions
Several medical conditions arise from or are closely associated with abnormal metabolic reactions. Type 2 diabetes mellitus is perhaps the most prevalent metabolic disorder in the UK, characterised by insulin resistance and impaired glucose metabolism. The pancreas initially compensates by producing more insulin, but over time, beta-cell function declines, resulting in chronic hyperglycaemia. According to Diabetes UK statistics, approximately 4.9 million people in the UK were living with diabetes in 2021, with type 2 diabetes accounting for about 90% of cases. Management typically involves lifestyle modifications, oral hypoglycaemic agents such as metformin (which reduces hepatic glucose production and enhances peripheral insulin sensitivity), and potentially insulin therapy.
Metabolic syndrome represents a cluster of conditions—including central obesity, hypertension, dyslipidaemia, and impaired glucose tolerance—that collectively increase cardiovascular disease risk. The NHS emphasises the importance of identifying and managing these risk factors through weight reduction, increased physical activity, and pharmacological interventions when appropriate.
Thyroid disorders significantly affect metabolic rate. Hyperthyroidism accelerates metabolism, causing weight loss, heat intolerance, tachycardia, and anxiety, whilst hypothyroidism slows metabolic processes, leading to weight gain, fatigue, cold intolerance, and constipation. According to NICE guidance (NG145), initial thyroid function tests include TSH and free T4; free T3 is measured selectively in certain cases such as suspected hyperthyroidism. Levothyroxine is the standard treatment for hypothyroidism.
Inborn errors of metabolism are rare genetic disorders affecting specific metabolic pathways. Examples include phenylketonuria (PKU), which impairs phenylalanine metabolism, and glycogen storage diseases, which affect glycogen synthesis or breakdown. These conditions are typically identified through the NHS newborn blood spot screening programme and require specialised dietary management and monitoring.
Non-alcoholic fatty liver disease (NAFLD) reflects abnormal hepatic lipid metabolism and is increasingly common, often associated with obesity and insulin resistance. Progressive cases may develop into non-alcoholic steatohepatitis (NASH) and cirrhosis, necessitating regular monitoring and lifestyle interventions as recommended in NICE guidance (NG49).
When to Seek Medical Advice About Metabolism
Individuals should consult their GP if they experience symptoms suggestive of metabolic dysfunction. Unexplained weight changes—either significant weight loss without dietary changes or progressive weight gain despite reasonable eating habits—warrant medical evaluation. Sudden weight loss may indicate hyperthyroidism, uncontrolled diabetes, or malignancy, whilst unexplained weight gain could suggest hypothyroidism, Cushing's syndrome, or medication side effects.
Persistent fatigue that does not improve with rest may reflect metabolic disorders such as hypothyroidism, diabetes, or adrenal insufficiency. When accompanied by other symptoms such as increased thirst, frequent urination, or blurred vision, diabetes should be considered. Patients should seek prompt assessment if they experience symptoms of hypoglycaemia (sweating, tremor, confusion, palpitations) or hyperglycaemia (polyuria, polydipsia, lethargy).
Cardiovascular symptoms including chest pain, palpitations, or shortness of breath, particularly in individuals with known metabolic risk factors, require urgent medical attention. Call 999 immediately for severe chest pain or symptoms of heart attack or stroke. These may indicate complications of dyslipidaemia or diabetes affecting the heart and blood vessels.
Individuals with a family history of metabolic conditions such as diabetes, thyroid disease, or inherited metabolic disorders should discuss screening with their GP. The NHS Health Check programme invites adults aged 40–74 for cardiovascular and metabolic risk assessment, including blood pressure, cholesterol, and glucose measurements.
Patients taking medications that affect metabolism—such as corticosteroids, antipsychotics, or thyroid medications—should attend regular monitoring appointments as recommended by NICE guidance. Any new or worsening symptoms whilst on these medications should prompt medical review. If you suspect you are experiencing side effects from medication, report them through the MHRA Yellow Card scheme.
Seek urgent medical care for severe hypoglycaemia (confusion, unconsciousness) or suspected diabetic ketoacidosis (very high glucose, vomiting, abdominal pain, rapid breathing). Additionally, women planning pregnancy or who are pregnant should ensure optimal metabolic control, particularly if they have diabetes or thyroid disease, as these conditions can affect maternal and foetal outcomes. Early intervention and appropriate management of metabolic disorders significantly improve long-term health outcomes and quality of life.
Scientific References
Frequently Asked Questions
What are the two main types of metabolic reactions?
The two main types are anabolic reactions, which build complex molecules from simpler ones using energy, and catabolic reactions, which break down complex molecules to release energy.
How do metabolic reactions affect body weight?
Metabolic reactions determine how efficiently the body converts food into energy. Metabolic rate, influenced by factors such as muscle mass, age, and thyroid function, affects energy balance and body composition.
When should I see a GP about metabolic concerns?
Consult your GP if you experience unexplained weight changes, persistent fatigue, symptoms of abnormal blood sugar (increased thirst, frequent urination), or have a family history of metabolic conditions such as diabetes or thyroid disease.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript