Understanding how your body converts stored fat into usable energy is fundamental to metabolic health and weight management. The process, known as lipolysis and beta-oxidation, involves complex biochemical pathways that break down triglycerides in adipose tissue into fatty acids, which are then transported to cells and converted into ATP—the body's primary energy currency. This natural mechanism operates continuously, influenced by hormonal signals, nutritional status, physical activity, and overall metabolic health. Whilst the body efficiently mobilises fat stores during fasting, exercise, or between meals, numerous factors including diet, sleep, stress, and underlying medical conditions can affect this process. This article explores the science behind fat metabolism and provides evidence-based guidance on supporting your body's natural fat-burning capacity.
Summary: The body converts fat into energy through lipolysis (breaking down triglycerides into fatty acids and glycerol) followed by beta-oxidation in mitochondria, producing ATP as cellular fuel.
- Hormones including adrenaline, glucagon, and insulin regulate fat mobilisation and storage through hormone-sensitive lipase activity.
- Beta-oxidation occurs in mitochondria via the carnitine shuttle system, generating acetyl-CoA that enters the citric acid cycle to produce ATP.
- Metabolic rate, influenced by age, body composition, thyroid function, and insulin sensitivity, determines fat-oxidation efficiency.
- Moderate-intensity aerobic exercise (50–65% maximum heart rate) optimises fat oxidation by allowing sufficient oxygen for mitochondrial metabolism.
- Medical conditions including hypothyroidism, type 2 diabetes, and PCOS can impair fat metabolism and require GP assessment and management.
Table of Contents
How Your Body Converts Fat Into Energy
The human body stores excess energy as adipose tissue (body fat), which serves as a vital energy reserve when dietary intake is insufficient to meet metabolic demands. The process of converting fat into usable energy is known as lipolysis, followed by beta-oxidation. This complex biochemical pathway ensures that stored triglycerides can be mobilised and transformed into adenosine triphosphate (ATP), the cellular energy currency.
When energy is required—such as during fasting, exercise, or periods between meals—hormones including adrenaline, noradrenaline, and glucagon signal adipose tissue to release stored fat. Triglycerides within fat cells are broken down by the enzyme hormone-sensitive lipase into glycerol and free fatty acids. These fatty acids enter the bloodstream and are transported to tissues such as skeletal muscle, cardiac muscle, and the liver, where they undergo further processing. The glycerol is transported to the liver where it can enter gluconeogenesis or glycolysis pathways.
Once inside cells, fatty acids are transported into the mitochondria—the cellular powerhouses—via the carnitine shuttle system (CPT1/CPT2), where beta-oxidation occurs. This metabolic process systematically breaks down fatty acid chains into two-carbon units called acetyl-CoA. Acetyl-CoA then enters the citric acid cycle (Krebs cycle), generating electron carriers that drive ATP production through oxidative phosphorylation. A single molecule of palmitic acid (a common fatty acid) can yield approximately 106 ATP molecules, making fat an exceptionally efficient energy source compared to carbohydrates.
During prolonged fasting or very low carbohydrate intake, the liver converts some fatty acids into ketone bodies (acetoacetate, beta-hydroxybutyrate, and acetone) through ketogenesis. These ketones serve as alternative fuel for the brain and other tissues. While mild ketosis is normal during fasting, excessive ketone production in people with diabetes can lead to diabetic ketoacidosis (DKA), a medical emergency.
This physiological mechanism operates continuously at varying intensities, with the rate of fat oxidation influenced by factors including hormonal balance, nutritional status, physical activity levels, and individual metabolic health. Understanding this process provides insight into how the body maintains energy homeostasis and adapts to different physiological demands.
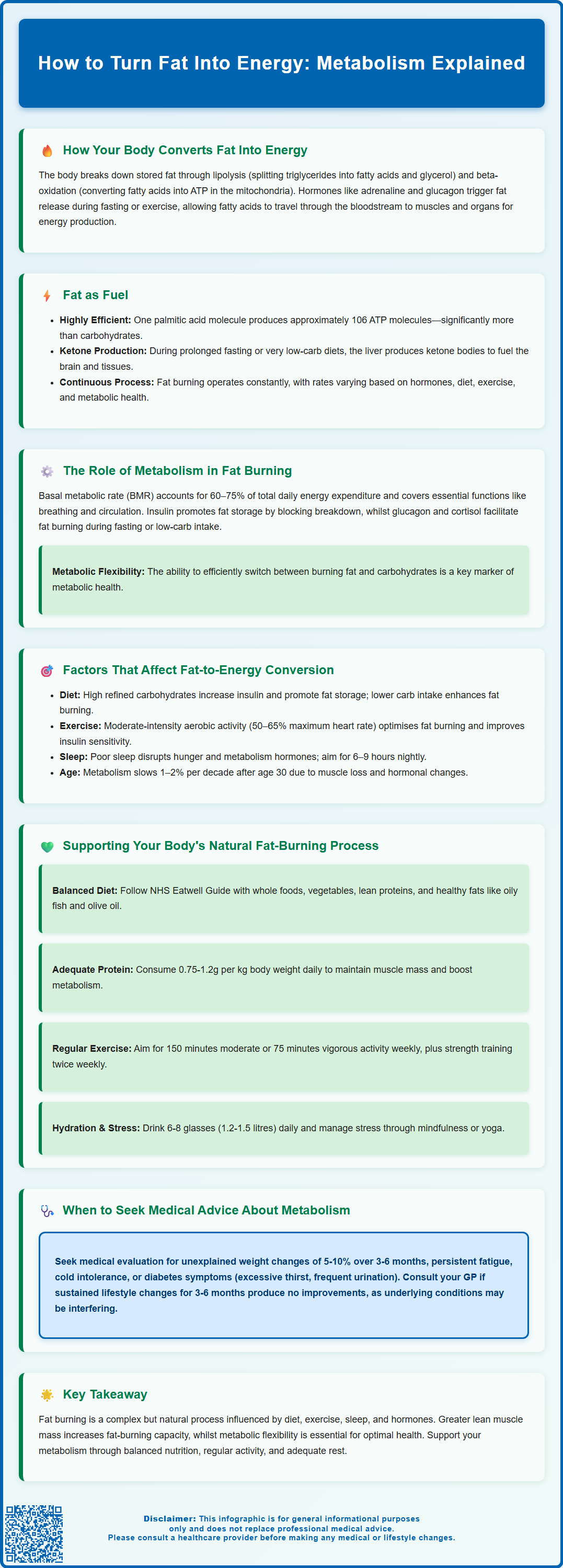
The Role of Metabolism in Fat Burning
Metabolism encompasses all chemical reactions that sustain life, including the breakdown of nutrients for energy (catabolism) and the synthesis of complex molecules (anabolism). Basal metabolic rate (BMR) represents the energy expenditure required to maintain essential physiological functions at rest, including respiration, circulation, cellular repair, and temperature regulation. BMR typically accounts for 60–75% of total daily energy expenditure (TDEE) in sedentary individuals. Other TDEE components include the thermic effect of food (energy used for digestion), non-exercise activity thermogenesis (NEAT), and deliberate physical activity.
Fat metabolism is intricately regulated by the endocrine system. Insulin, secreted by pancreatic beta cells in response to elevated blood glucose, promotes fat storage by inhibiting lipolysis and stimulating lipogenesis (fat synthesis). Conversely, when insulin levels decline—such as during fasting or low-carbohydrate intake—counter-regulatory hormones including glucagon, cortisol, growth hormone, and catecholamines facilitate fat mobilisation. Thyroid hormones (T3 and T4) also play a crucial role in regulating metabolic rate, with hypothyroidism potentially reducing fat oxidation capacity.
The respiratory exchange ratio (RER), measured during metabolic testing, indicates the proportion of energy derived from fat versus carbohydrate oxidation. At rest and during low-intensity activity, the body preferentially oxidises fat, whereas higher-intensity exercise shifts metabolism toward carbohydrate utilisation due to the faster ATP production rate from glycolysis. It's worth noting that indirect calorimetry and RER testing are specialist assessments not routinely available in primary care settings.
Individual metabolic rate varies considerably based on factors including age, sex, body composition, and genetic predisposition. Muscle tissue is metabolically active, consuming more energy at rest than adipose tissue. Consequently, individuals with greater lean muscle mass typically exhibit higher BMR and enhanced fat-oxidation capacity. Metabolic flexibility—the ability to efficiently switch between fuel sources—is a hallmark of metabolic health and is often impaired in conditions such as insulin resistance and type 2 diabetes mellitus.
Factors That Affect Fat-to-Energy Conversion
Numerous physiological, lifestyle, and pathological factors influence the efficiency of fat oxidation. Dietary composition significantly impacts substrate utilisation: diets high in refined carbohydrates and sugars promote insulin secretion, favouring glucose oxidation and fat storage. Conversely, lower carbohydrate intake or periods of fasting enhance fat mobilisation by reducing insulin levels and increasing glucagon secretion.
Physical activity is a potent modulator of fat metabolism. Aerobic exercise at moderate intensity (approximately 50–65% of maximum heart rate) optimises fat oxidation rates, as this intensity allows sufficient oxygen delivery for mitochondrial beta-oxidation. Regular exercise also improves insulin sensitivity, enhances mitochondrial density, and increases expression of enzymes involved in fat metabolism, thereby improving metabolic flexibility over time.
Sleep quality and duration profoundly affect metabolic regulation. Sleep deprivation disrupts hormonal balance, elevating cortisol and ghrelin (hunger hormone) whilst reducing leptin (satiety hormone), which can impair glucose metabolism and promote fat accumulation. The NHS recommends most adults need 6–9 hours of quality sleep nightly for optimal health.
Age-related changes include gradual decline in BMR (approximately 1–2% per decade after age 30), reduced muscle mass (sarcopenia), and hormonal shifts such as menopause in women and declining testosterone in men, all of which can diminish fat-oxidation capacity. Chronic stress elevates cortisol chronically, which promotes visceral fat deposition and insulin resistance.
Certain medical conditions impair fat metabolism, including hypothyroidism, polycystic ovary syndrome (PCOS), Cushing's syndrome, and genetic lipid metabolism disorders. Medications such as corticosteroids, some antipsychotics, and beta-blockers may also affect metabolic rate and fat oxidation. If you suspect a medical condition is affecting your metabolism, consult your GP for appropriate investigation and management. Do not stop or change any prescribed medications without discussing with your healthcare provider first.
Supporting Your Body's Natural Fat-Burning Process
Optimising fat metabolism requires a holistic approach addressing nutrition, physical activity, sleep, and stress management. Balanced nutrition forms the foundation: prioritise whole foods including vegetables, fruits, lean proteins, whole grains, and healthy fats from sources such as oily fish, nuts, seeds, and olive oil. The NHS Eatwell Guide provides evidence-based recommendations for balanced dietary patterns that support metabolic health.
Adequate protein intake is important for muscle maintenance. The UK Reference Nutrient Intake (RNI) is 0.75g per kilogram body weight daily for adults, though higher intakes (1.0–1.2g/kg/day) may benefit older adults, those in energy deficit, or physically active individuals. Protein has a higher thermic effect than carbohydrates or fats, meaning more energy is expended during digestion. Spreading protein intake across meals may optimise muscle protein synthesis and metabolic rate.
Regular physical activity is essential. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity weekly, combined with strength training on two or more days. Resistance training builds lean muscle mass, which elevates resting metabolic rate. High-intensity interval training (HIIT) can enhance post-exercise oxygen consumption (EPOC), though this contributes modestly to overall energy expenditure.
Hydration supports all metabolic processes; even mild dehydration can reduce metabolic efficiency. Aim for 6–8 glasses (approximately 1.2–1.5 litres) of fluid daily, more during exercise or hot weather.
Stress management techniques including mindfulness, yoga, or cognitive behavioural approaches can help regulate cortisol levels. Establishing consistent sleep routines and creating a conducive sleep environment (cool, dark, quiet) supports circadian rhythm regulation and metabolic health.
Avoid extreme caloric restriction, which can trigger metabolic adaptation (reduced BMR) as a protective mechanism. Sustainable, modest caloric deficits (approximately 600 kcal daily) combined with adequate protein and resistance training preserve lean mass whilst promoting fat loss. There is no evidence supporting 'fat-burning' supplements or detox products; many lack regulatory approval and may pose health risks. The MHRA advises caution with unregulated weight-loss products.
When to Seek Medical Advice About Metabolism
Whilst metabolic rate varies naturally between individuals, certain signs and symptoms warrant medical evaluation. Unexplained weight changes—particularly rapid weight gain despite no dietary changes, or unintentional weight loss—may indicate underlying endocrine disorders such as thyroid dysfunction, diabetes mellitus, or Cushing's syndrome. Contact your GP if you experience unintentional weight loss of 5–10% of body weight over 3–6 months, as this is considered clinically significant according to UK malnutrition screening criteria.
Persistent fatigue, cold intolerance, dry skin, hair loss, constipation, or depression may suggest hypothyroidism. Conversely, unexplained weight loss, heat intolerance, palpitations, tremor, or anxiety could indicate hyperthyroidism. Thyroid function tests (TSH, free T4) can diagnose these conditions, which are readily treatable with medication.
Symptoms of diabetes mellitus include excessive thirst, frequent urination, unexplained weight loss, blurred vision, and recurrent infections. Type 2 diabetes significantly impairs metabolic flexibility and fat oxidation. Early diagnosis through fasting glucose or HbA1c testing enables lifestyle interventions and pharmacological management to prevent complications. Seek urgent medical attention if you experience symptoms of diabetic ketoacidosis (DKA): abdominal pain, vomiting, deep/rapid breathing, drowsiness/confusion, or fruity-smelling breath, particularly if you have diabetes or suspect undiagnosed diabetes.
Polycystic ovary syndrome (PCOS), affecting approximately 10% of women of reproductive age, causes insulin resistance, irregular periods, hirsutism, and difficulty losing weight. NICE guidelines recommend lifestyle modification as first-line management. Metformin may be considered for metabolic dysfunction in PCOS, though this is an off-label use in the UK and should be discussed with your healthcare provider regarding risks and benefits.
If you have implemented sustained lifestyle modifications (balanced diet, regular exercise, adequate sleep) for 3–6 months without expected metabolic improvements, discuss this with your GP. They may investigate for underlying conditions, assess medications that might affect metabolism, or refer you to specialist services including endocrinology or dietetics.
Call 999 or go to A&E for severe chest pain, severe breathlessness, or signs of serious illness. For non-urgent concerns about metabolism, weight management, or related symptoms, book a routine GP appointment for comprehensive assessment and evidence-based guidance tailored to your individual circumstances.
Frequently Asked Questions
What is the process called when your body converts fat into energy?
The process is called lipolysis (breakdown of triglycerides into fatty acids and glycerol) followed by beta-oxidation, where fatty acids are converted into acetyl-CoA in mitochondria to produce ATP, the body's energy currency.
What type of exercise is best for burning fat?
Moderate-intensity aerobic exercise at approximately 50–65% of maximum heart rate optimises fat oxidation, as this intensity allows sufficient oxygen delivery for mitochondrial beta-oxidation. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity weekly, combined with strength training twice weekly.
When should I see a GP about my metabolism?
Consult your GP if you experience unexplained weight changes (particularly 5–10% loss over 3–6 months), persistent fatigue, symptoms of thyroid dysfunction, signs of diabetes (excessive thirst, frequent urination), or if lifestyle modifications produce no improvement after 3–6 months.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












