Metabolic stress describes a state where the body's normal metabolic processes become disrupted or overwhelmed, leading to cellular dysfunction and potential tissue damage. This physiological response occurs across various conditions, from acute critical illness and major trauma to chronic states such as obesity and type 2 diabetes. At the cellular level, metabolic stress triggers biochemical responses including oxidative stress, mitochondrial dysfunction, and inflammatory signalling. Understanding metabolic stress is essential for managing acutely unwell patients in critical care settings and for individuals seeking to optimise their metabolic health through lifestyle modifications. This article explores the causes, signs, and evidence-based management strategies for metabolic stress.
Summary: Metabolic stress is a physiological state where the body's normal metabolic processes become disrupted or overwhelmed, leading to cellular dysfunction and potential tissue damage.
- Metabolic stress occurs when cells cannot maintain usual energy production, protein synthesis, or waste removal due to internal or external stressors
- Acute causes include major trauma, sepsis, burns, and critical illness; chronic causes include type 2 diabetes, obesity, and cardiovascular disease
- Clinical features include increased energy expenditure, elevated stress hormones (cortisol, adrenaline), altered glucose metabolism, and activation of inflammatory pathways
- Management requires addressing underlying causes, nutritional support (particularly protein in critical illness), lifestyle modifications including diet and exercise, and appropriate medical interventions
- Seek immediate medical attention (call 999) for signs of acute metabolic decompensation including severe weakness, confusion, rapid breathing, or sepsis symptoms
Table of Contents
What Is Metabolic Stress?
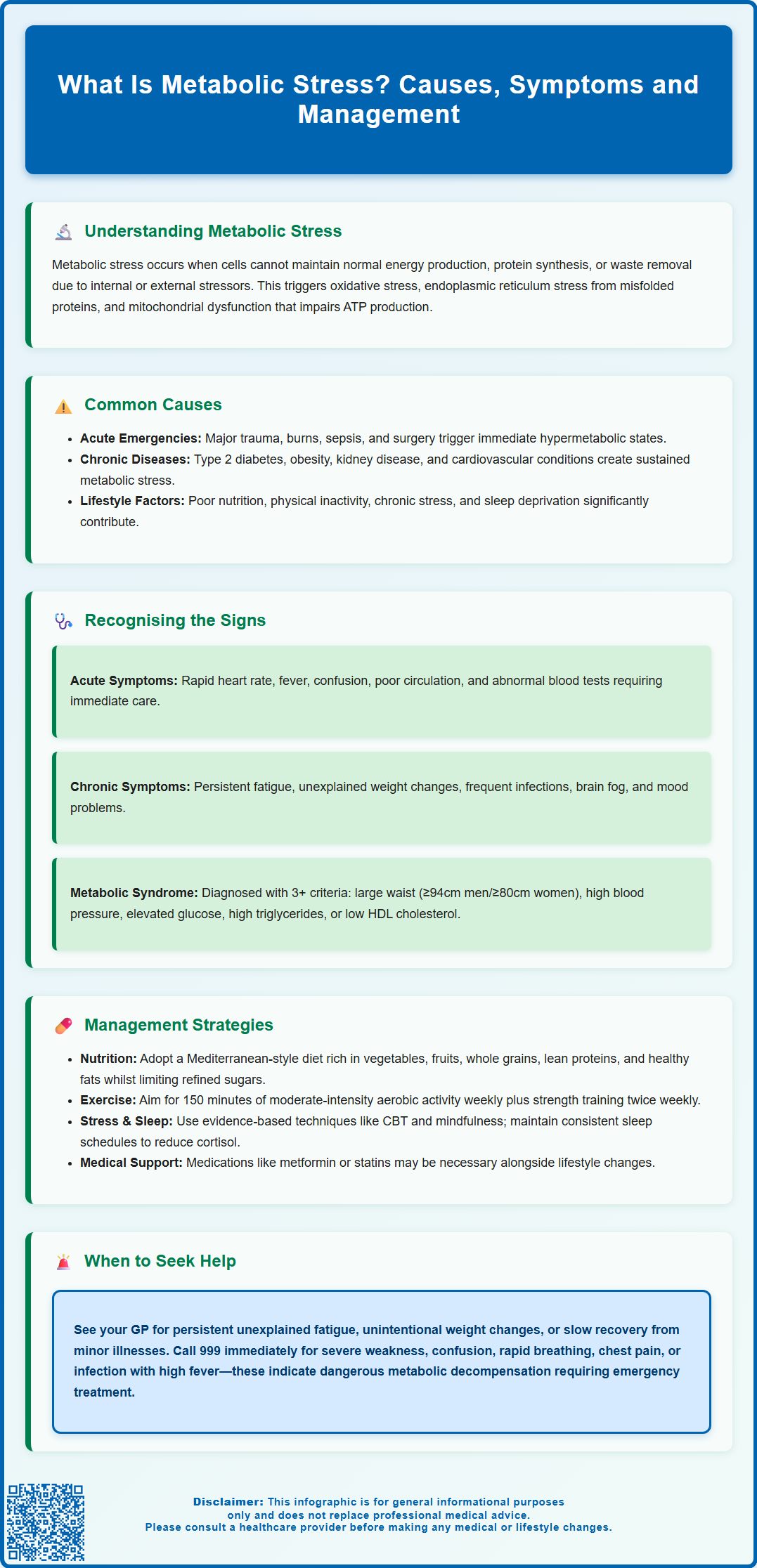
Metabolic stress refers to a state in which the body's normal metabolic processes are disrupted or overwhelmed, leading to cellular dysfunction and potential tissue damage. This physiological concept describes a response across various conditions rather than being a formal diagnosis. It occurs when cells cannot maintain their usual energy production, protein synthesis, or waste removal functions due to various internal or external stressors. The term encompasses both acute situations, such as severe illness or injury, and chronic conditions that gradually impair metabolic function.
At the cellular level, metabolic stress triggers a cascade of biochemical responses. Cells may experience oxidative stress from an accumulation of reactive oxygen species (ROS), endoplasmic reticulum stress from misfolded proteins, or mitochondrial dysfunction affecting ATP production. These disruptions activate stress response pathways, including the unfolded protein response and inflammatory signalling cascades, which attempt to restore cellular homeostasis.
In clinical practice, metabolic stress is particularly relevant in critical care settings, where severe illness, trauma, or major surgery can induce a hypermetabolic state. During such episodes, the body's energy demands increase substantially whilst its ability to utilise nutrients efficiently may be compromised. This can lead to accelerated muscle breakdown (catabolism), altered glucose metabolism, and changes in how the body processes fats and proteins.
Key characteristics of metabolic stress include:
-
Increased energy expenditure and oxygen consumption
-
Elevated stress hormone levels (cortisol, adrenaline)
-
Altered substrate utilisation and nutrient metabolism
-
Activation of inflammatory pathways
-
Potential for organ dysfunction if prolonged or severe
Understanding metabolic stress is essential for healthcare professionals managing acutely unwell patients, as highlighted in NICE Clinical Guideline CG32 on nutrition support, and for individuals seeking to optimise their metabolic health through lifestyle modifications.
Common Causes of Metabolic Stress
Metabolic stress can arise from numerous physiological and pathological conditions, ranging from acute medical emergencies to chronic lifestyle factors. Acute causes typically involve sudden, severe insults to the body that trigger immediate metabolic responses. These include major trauma, extensive burns, sepsis (severe infection) as outlined in NICE guideline NG51, major surgical procedures, and acute organ failure. In these situations, the body enters a hypermetabolic state characterised by increased energy demands, elevated stress hormone secretion, and systemic inflammation.
Critical illness represents one of the most significant causes of metabolic stress. Patients in intensive care units often experience profound metabolic derangements due to sepsis, acute respiratory distress syndrome (ARDS), or multi-organ dysfunction. The inflammatory response in these conditions drives increased protein breakdown, insulin resistance, and altered lipid metabolism, all contributing to the metabolic stress state.
Chronic conditions can also induce sustained metabolic stress. Type 2 diabetes mellitus creates ongoing metabolic dysfunction through insulin resistance and hyperglycaemia, leading to oxidative stress and cellular damage over time. Obesity, particularly visceral adiposity, promotes chronic low-grade inflammation and metabolic dysregulation. Chronic kidney disease and liver disease impair the body's ability to maintain metabolic homeostasis, whilst cardiovascular disease is both a cause and consequence of metabolic stress.
Endocrine disorders such as uncontrolled hyperthyroidism or Cushing's syndrome can significantly disrupt metabolic processes through hormonal imbalances that affect energy expenditure and nutrient metabolism.
Lifestyle and environmental factors play substantial roles in metabolic stress development:
-
Poor nutrition: Excessive caloric intake, high refined sugar consumption, or inadequate micronutrient intake
-
Physical inactivity: Sedentary behaviour impairs metabolic flexibility and insulin sensitivity
-
Chronic psychological stress: Prolonged cortisol elevation affects glucose metabolism and promotes inflammation
-
Sleep deprivation: Disrupts hormonal balance and metabolic regulation
-
Environmental factors: Exposure to certain pollutants may contribute to metabolic disruption in some individuals
Certain medications, particularly long-term systemic corticosteroids (such as prednisolone), can induce metabolic stress through effects on glucose metabolism, protein breakdown, and fat redistribution, as documented in the British National Formulary. Understanding these diverse causes enables targeted prevention and management strategies.
Signs and Symptoms of Metabolic Stress
The clinical presentation of metabolic stress varies considerably depending on its severity, duration, and underlying cause. In acute metabolic stress, such as that occurring during critical illness, signs are often dramatic and require immediate medical attention. Patients may exhibit tachycardia (rapid heart rate), tachypnoea (rapid breathing), fever or hypothermia, altered mental status, and signs of poor tissue perfusion such as cool, mottled skin. Laboratory investigations typically reveal hyperglycaemia (elevated blood glucose), elevated inflammatory markers (C-reactive protein, white cell count), and derangements in electrolytes and acid-base balance.
Acute metabolic stress often manifests with systemic signs including:
-
Significant unintentional weight loss, particularly muscle mass
-
Profound fatigue and weakness
-
Poor wound healing or increased infection susceptibility
-
Fluid retention or oedema
-
Changes in vital signs (blood pressure, heart rate, temperature)
Chronic metabolic stress presents more subtly, with symptoms developing gradually over months or years. Individuals may experience persistent fatigue that doesn't improve with rest, difficulty maintaining or losing weight despite dietary efforts, and increased susceptibility to infections. Brain fog, poor concentration, and mood disturbances are common complaints. Physical signs might include central obesity, skin changes (such as acanthosis nigricans in insulin resistance), or signs of nutrient deficiencies.
Metabolic syndrome, a cluster of conditions associated with chronic metabolic stress, is diagnosed when three or more of the following are present: increased waist circumference (≥94cm for European men, ≥80cm for European women, with lower thresholds for South Asian and some other ethnic groups), elevated blood pressure (≥130/85 mmHg or on treatment), raised fasting glucose (≥5.6 mmol/L or on treatment), high triglycerides (≥1.7 mmol/L or on treatment), and low HDL cholesterol (<1.03 mmol/L in men, <1.29 mmol/L in women, or on treatment). This constellation significantly increases cardiovascular disease risk.
When to seek medical attention: Patients should contact their GP if they experience persistent unexplained fatigue, unintentional weight changes, increased thirst and urination (possible diabetes with fasting glucose ≥7.0 mmol/L or HbA1c ≥48 mmol/mol), or difficulty recovering from minor illnesses. Immediate medical attention (call 999 or go to A&E) is required for signs of acute metabolic decompensation: severe weakness, confusion, rapid breathing, chest pain, or signs of infection with systemic symptoms such as high fever and feeling very unwell. The NHS sepsis page outlines specific red flags requiring emergency care. Healthcare professionals should maintain a high index of suspicion for metabolic stress in vulnerable populations, including older adults, those with multiple comorbidities, and patients recovering from major illness or surgery.
Managing and Reducing Metabolic Stress
Effective management of metabolic stress requires a comprehensive approach tailored to its underlying cause, severity, and chronicity. In acute clinical settings, management focuses on addressing the precipitating condition whilst providing metabolic support. This includes appropriate fluid resuscitation, electrolyte correction, glycaemic control, and nutritional support. NICE guidance emphasises early identification and treatment of sepsis (NG51), optimised perioperative care, and appropriate critical care interventions for severely unwell patients.
Nutritional support is fundamental in managing metabolic stress. In critical illness, early enteral nutrition (feeding via the gastrointestinal tract) is preferred when feasible, as it helps maintain gut integrity and immune function, as recommended in NICE CG32 and ESPEN guidelines. Protein requirements are typically elevated during critical illness, with targets individually prescribed by a dietitian (generally 1.2–2.0 g/kg/day based on ideal or adjusted body weight), to counteract catabolism. Energy provision must be carefully calculated to avoid overfeeding or underfeeding. Assessment and treatment of specific micronutrient deficiencies may be required, guided by clinical assessment and specialist dietetic input.
Lifestyle modifications form the cornerstone of managing chronic metabolic stress:
Dietary interventions:
-
Adopt a balanced, whole-food diet rich in vegetables, fruits, whole grains, lean proteins, and healthy fats
-
Limit refined sugars, processed foods, and excessive saturated fat intake
-
Consider Mediterranean-style eating patterns, which demonstrate metabolic benefits
-
Maintain adequate hydration
-
Time-restricted eating or intermittent fasting may benefit some individuals, but should be discussed with a healthcare professional, particularly for those with diabetes on insulin or sulfonylureas, pregnancy, breastfeeding, history of eating disorders, or frailty
Physical activity: Regular exercise improves insulin sensitivity, reduces inflammation, and enhances metabolic flexibility. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity aerobic activity weekly, plus strength training twice weekly. Even modest increases in physical activity provide metabolic benefits for sedentary individuals.
Stress management and sleep optimisation: Chronic psychological stress perpetuates metabolic dysfunction through sustained cortisol elevation. Evidence-based stress reduction techniques include cognitive behavioural therapy (CBT), mindfulness-based interventions, and relaxation techniques. Prioritising sleep hygiene—maintaining consistent sleep schedules, creating conducive sleep environments, and addressing sleep disorders—is essential for metabolic health.
Smoking cessation: Smoking contributes to metabolic dysfunction and cardiovascular risk. The NHS Stop Smoking Services provide evidence-based support for those looking to quit.
Medical management: For individuals with metabolic syndrome or related conditions, pharmacological interventions may be necessary. Metformin improves insulin sensitivity in type 2 diabetes (NICE NG28), statins address dyslipidaemia (NICE NG238), and antihypertensives control blood pressure (NICE NG136). These medications should be used alongside lifestyle modifications, not as replacements. Regular monitoring through blood tests (glucose, lipids, liver and kidney function) and clinical assessments enables early detection of metabolic derangements. If you suspect you're experiencing side effects from any medication, report them through the MHRA Yellow Card scheme.
Patient safety and monitoring: Individuals with chronic metabolic stress should engage with their GP for regular health reviews, typically annually or more frequently if complications arise. Self-monitoring of weight, blood pressure (if hypertensive), and blood glucose (if diabetic) empowers patients in their care. Healthcare professionals should provide clear safety-netting advice, ensuring patients understand when to seek urgent review—such as with acute illness, unexplained symptoms, or difficulty managing chronic conditions. Call 999 or go to A&E immediately for severe breathlessness, chest pain, confusion, or signs of sepsis. Multidisciplinary approaches involving dietitians, physiotherapists, and diabetes specialist nurses optimise outcomes for complex cases.
Scientific References
Frequently Asked Questions
What are the main causes of metabolic stress?
Metabolic stress can result from acute causes such as major trauma, sepsis, burns, and critical illness, or chronic conditions including type 2 diabetes, obesity, cardiovascular disease, and chronic kidney disease. Lifestyle factors such as poor nutrition, physical inactivity, chronic psychological stress, and sleep deprivation also contribute to metabolic stress development.
How do you know if you have metabolic stress?
Signs of metabolic stress vary by severity but may include persistent fatigue, unintentional weight changes, difficulty concentrating, increased infection susceptibility, and in acute cases, rapid heart rate, altered mental status, and elevated blood glucose. Metabolic syndrome—diagnosed when three or more criteria including increased waist circumference, elevated blood pressure, raised fasting glucose, high triglycerides, or low HDL cholesterol are present—indicates chronic metabolic stress.
Can metabolic stress be reversed?
Many forms of chronic metabolic stress can be improved or reversed through comprehensive lifestyle modifications including a balanced whole-food diet, regular physical activity (at least 150 minutes weekly of moderate-intensity exercise), stress management, adequate sleep, and smoking cessation. Medical management with medications such as metformin, statins, or antihypertensives may be necessary alongside lifestyle changes, with regular monitoring by healthcare professionals.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript