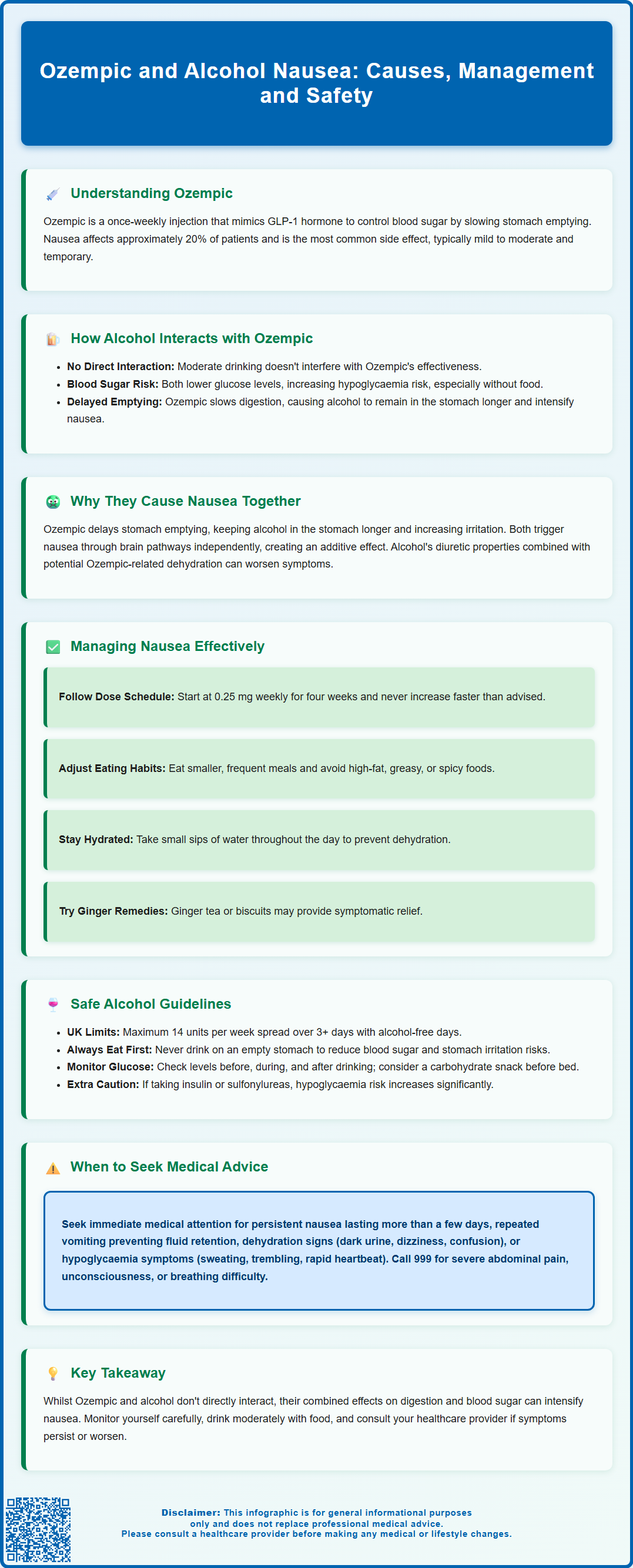
Ozempic (semaglutide) is a GLP-1 receptor agonist used to treat type 2 diabetes in the UK. Nausea is a very common side effect, affecting approximately 20% of patients, particularly during initial treatment. When combined with alcohol, nausea may be exacerbated through overlapping mechanisms including delayed gastric emptying, gastric irritation, and central nervous system effects. Whilst no direct pharmacokinetic interaction exists between Ozempic and alcohol, understanding how these substances interact can help patients manage symptoms effectively. This article explores the relationship between Ozempic and alcohol-related nausea, offering evidence-based guidance for safe management.
Summary: Ozempic and alcohol together may worsen nausea through delayed gastric emptying, gastric irritation, and overlapping effects on brain centres controlling nausea.
- Ozempic (semaglutide) is a GLP-1 receptor agonist causing nausea in approximately 20% of patients through delayed gastric emptying and central effects.
- No direct pharmacokinetic interaction exists between alcohol and Ozempic, but both can independently affect blood glucose and gastrointestinal function.
- Alcohol may remain in the stomach longer when taking Ozempic, prolonging gastric irritation and potentially intensifying nausea.
- Management includes gradual dose titration, smaller frequent meals, adequate hydration, and avoiding alcohol on an empty stomach.
- UK guidelines recommend maximum 14 units weekly; patients should monitor blood glucose and seek medical advice for persistent nausea or dehydration signs.
Table of Contents
Understanding Ozempic and Its Gastrointestinal Effects
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, it works by mimicking the action of the naturally occurring hormone GLP-1, which plays a crucial role in glucose regulation. The medication enhances insulin secretion in response to elevated blood glucose levels, suppresses inappropriate glucagon release, and slows gastric emptying—all mechanisms that contribute to improved glycaemic control.
One of the most commonly reported adverse effects of Ozempic involves the gastrointestinal system. Nausea is experienced very commonly (approximately 20% of patients), particularly during the initial weeks of treatment or following dose escalation. This occurs due to both central GLP-1 effects and delayed gastric emptying, meaning food remains in the stomach for longer periods. Other gastrointestinal effects include vomiting, diarrhoea, constipation, and abdominal discomfort. These symptoms are generally dose-dependent and tend to diminish over time as the body adapts to the medication.
According to the SmPC, gastrointestinal adverse reactions are usually mild to moderate in severity and transient in nature. However, for some individuals, these effects can be persistent enough to affect quality of life or adherence to treatment. Understanding that nausea is an expected pharmacological consequence of how Ozempic works—rather than an allergic reaction—helps patients and clinicians manage expectations and develop appropriate coping strategies. The gradual dose titration schedule as per the SmPC and BNF (starting at 0.25 mg once weekly for four weeks, then increasing to 0.5 mg, with further increases to 1 mg or 2 mg if needed) is specifically designed to minimise these gastrointestinal effects whilst allowing therapeutic benefit. Slower titration or temporary dose reduction may be necessary for some patients experiencing significant gastrointestinal symptoms.
How Alcohol Interacts with Ozempic
The SmPC for Ozempic does not indicate a specific interaction with alcohol. There is no known direct pharmacokinetic interaction documented between alcohol and semaglutide. Alcohol does not appear to significantly alter the absorption, distribution, metabolism, or elimination of Ozempic, nor does semaglutide affect how the body processes alcohol. The medication is metabolised through proteolytic degradation rather than hepatic cytochrome P450 enzymes, which are the primary pathways affected by alcohol metabolism. From a purely pharmacological perspective, moderate alcohol consumption does not appear to interfere with the glucose-lowering efficacy of Ozempic.
However, indirect interactions warrant careful consideration. Both alcohol and Ozempic can independently affect blood glucose levels, though in different ways. Whilst Ozempic lowers blood glucose through its GLP-1 receptor agonist activity, alcohol can cause hypoglycaemia, particularly when consumed without food or in excessive amounts. This occurs because alcohol inhibits hepatic gluconeogenesis—the liver's ability to produce glucose—which can be problematic for individuals with diabetes, especially those taking glucose-lowering medications.
The risk of hypoglycaemia is particularly increased when Ozempic is used in combination with insulin or sulfonylureas, and alcohol consumption may further heighten this risk. Patients using these combinations may need dose adjustments and more frequent blood glucose monitoring when consuming alcohol.
Furthermore, alcohol itself is a gastric irritant that can cause nausea, vomiting, and gastrointestinal discomfort even in healthy individuals. When combined with Ozempic's effect of slowing gastric emptying, alcohol may remain in the stomach longer than usual, potentially intensifying its irritant effects on the gastric mucosa. The delayed gastric emptying means that both food and beverages, including alcoholic drinks, are processed more slowly, which can contribute to feelings of fullness, bloating, and nausea. This physiological interaction, whilst not a formal drug-drug interaction, has practical implications for patients taking Ozempic who choose to consume alcohol.
Why Ozempic and Alcohol Together May Cause Nausea
The combination of Ozempic and alcohol may exacerbate nausea through several overlapping mechanisms, though it's important to note that individual responses vary and clinical trial evidence specifically examining this combination is limited. Firstly, Ozempic significantly delays gastric emptying as part of its therapeutic action. When alcohol is consumed, it may remain in the stomach for an extended period, prolonging contact with the gastric lining. Alcohol is known to stimulate gastric acid secretion and can directly irritate the stomach mucosa, effects that are potentially amplified when gastric contents are retained longer than normal.
Secondly, both substances can independently trigger nausea through central mechanisms. Alcohol affects the vestibular system and chemoreceptor trigger zone in the brain, which are involved in the sensation of nausea and the vomiting reflex. GLP-1 receptors are also present in areas of the brain associated with nausea and satiety, including the area postrema. When Ozempic activates these receptors, it can produce feelings of nausea and reduced appetite. The concurrent use of alcohol may create an additive effect on these neural pathways, making nausea more likely or more severe.
Additionally, dehydration plays a contributory role. Alcohol is a diuretic, promoting fluid loss through increased urination. Dehydration itself can worsen nausea and is a common consequence of both alcohol consumption and gastrointestinal side effects from Ozempic (particularly if vomiting or diarrhoea occur). When patients experience nausea from Ozempic, they may reduce their fluid intake, and adding alcohol to this scenario can compound dehydration and create a cycle of worsening symptoms.
Careful self-monitoring is advised when introducing alcohol while taking Ozempic, particularly during the initial treatment period or after dose increases, as tolerance and susceptibility to these effects vary considerably between individuals.
Managing Nausea When Taking Ozempic
Effective management of nausea whilst taking Ozempic involves both non-pharmacological and, if necessary, pharmacological strategies. The most important initial approach is adherence to the recommended dose titration schedule. Ozempic is typically started at 0.25 mg once weekly for four weeks, then increased to 0.5 mg weekly, with further increases to 1 mg or 2 mg if needed for glycaemic control. This gradual escalation allows the gastrointestinal system to adapt to the medication's effects. Some patients may benefit from slower titration or temporary dose reduction if experiencing significant gastrointestinal symptoms. Patients should never increase their dose more rapidly than recommended, as this significantly increases the risk of nausea and vomiting.
Dietary modifications can substantially reduce nausea. Patients are advised to:
-
Eat smaller, more frequent meals rather than large portions
-
Avoid high-fat, greasy, or spicy foods that can exacerbate gastric discomfort
-
Choose bland, easily digestible foods when nausea is present
-
Eat slowly and chew food thoroughly
-
Avoid lying down immediately after eating
-
Stay well-hydrated with small, frequent sips of water throughout the day
Timing of Ozempic administration may also help; some patients find that injecting in the evening reduces daytime nausea, though this should be discussed with a healthcare provider. Ginger-based remedies, such as ginger tea or ginger biscuits, have traditional use for nausea and may provide symptomatic relief for some individuals, though evidence for their efficacy specifically with GLP-1 agonist-induced nausea is limited.
If nausea persists despite these measures and affects hydration or nutrition, patients should seek medical advice. Antiemetic medications may be considered but should only be used under medical supervision. Options include:
-
Metoclopramide: Restricted to short-term use (maximum 5 days) due to risk of neurological side effects
-
Domperidone: Should only be used at the lowest effective dose for the shortest possible duration and is contraindicated in certain cardiac conditions or with medications that prolong the QT interval
-
Prochlorperazine: May be considered as an alternative
Persistent or severe nausea that interferes with nutrition, hydration, or quality of life warrants medical review, as dose adjustment or alternative diabetes treatments may be necessary. Patients unable to keep fluids down should seek prompt medical attention due to the risk of dehydration and acute kidney injury.
Safe Alcohol Consumption Guidelines for Ozempic Users
The UK Chief Medical Officers' guidelines for alcohol consumption apply to individuals taking Ozempic, recommending no more than 14 units of alcohol per week for both men and women, spread over three or more days with several alcohol-free days each week. One unit equals 10 ml or 8 g of pure alcohol—approximately half a pint of standard-strength (4% ABV) lager, a single measure (25 ml) of spirits (40% ABV), or a small glass (125 ml) of wine (12% ABV). Note that unit calculations depend on the alcohol by volume (ABV) of the drink, with stronger drinks containing more units. However, people with diabetes taking Ozempic should consider additional precautions beyond these general population guidelines.
Practical recommendations for Ozempic users who choose to drink alcohol include:
-
Never drink on an empty stomach: Always consume alcohol with food to reduce both hypoglycaemia risk and gastric irritation
-
Start with smaller amounts: If you are new to Ozempic or have recently increased your dose, consider drinking less than your usual amount to assess tolerance
-
Stay well-hydrated: Alternate alcoholic drinks with water to maintain hydration and reduce nausea risk
-
Avoid binge drinking: Large quantities of alcohol significantly increase risks of hypoglycaemia, nausea, and vomiting
-
Monitor blood glucose: Check blood glucose levels before drinking, during extended drinking occasions, and before bed, as alcohol-induced hypoglycaemia can occur several hours after consumption
-
Consider a bedtime snack: A carbohydrate-containing snack before sleep may help prevent overnight hypoglycaemia, especially after drinking
-
Carry diabetes identification: Ensure you have identification indicating you have diabetes, as hypoglycaemia symptoms can be mistaken for intoxication
Patients taking Ozempic alongside insulin or sulfonylureas should be particularly cautious with alcohol, as the combination significantly increases hypoglycaemia risk. These patients may need medication dose adjustments and more frequent glucose monitoring when consuming alcohol.
It is important to recognise that alcohol provides empty calories (approximately 7 kcal per gram) and can interfere with weight management goals. Many patients taking Ozempic are working towards weight reduction as part of their diabetes management or cardiovascular risk reduction strategy. Regular alcohol consumption can undermine these efforts and may also affect diabetes control through its carbohydrate content and effects on insulin sensitivity. Some individuals may find that abstaining from alcohol or significantly reducing consumption improves both their diabetes management and reduces gastrointestinal symptoms whilst taking Ozempic.
When to Seek Medical Advice
Certain symptoms warrant prompt medical attention when taking Ozempic, whether or not alcohol has been consumed. Patients should contact their GP or diabetes care team if they experience persistent nausea lasting more than a few days that interferes with eating or drinking, as this can lead to dehydration and nutritional deficiencies. Similarly, repeated vomiting that prevents retention of fluids or medications requires medical assessment, as this may necessitate temporary discontinuation of Ozempic or hospital admission for intravenous rehydration.
Signs of dehydration requiring medical review include:
-
Reduced urine output or dark-coloured urine
-
Dizziness or light-headedness, particularly on standing
-
Dry mouth and increased thirst
-
Fatigue and confusion
-
Rapid heartbeat
These symptoms can develop from the combination of Ozempic-related gastrointestinal effects and alcohol consumption, particularly if vomiting or reduced fluid intake occurs.
Hypoglycaemia is another important concern. Whilst Ozempic alone carries a low risk of hypoglycaemia, the combination with alcohol increases this risk, especially if also taking insulin or sulfonylureas. Symptoms of low blood glucose include sweating, trembling, confusion, rapid heartbeat, blurred vision, and in severe cases, loss of consciousness or seizures. If blood glucose falls below 4 mmol/L, immediate treatment with fast-acting carbohydrate (such as glucose tablets, sugary drinks, or sweets) is required, followed by a longer-acting carbohydrate source. Severe hypoglycaemia requiring assistance from another person is a medical emergency—call 999.
Severe abdominal pain, particularly if persistent and located in the upper abdomen radiating to the back, should prompt urgent medical assessment, as acute pancreatitis is a rare but serious adverse effect of GLP-1 receptor agonists. Right upper quadrant pain, especially if accompanied by fever or yellowing of the skin/eyes (jaundice), requires urgent evaluation as GLP-1 receptor agonists have been associated with gallbladder disease.
Patients should seek medical advice for any vision changes, particularly if they have pre-existing diabetic retinopathy, as rapid improvement in glucose control with Ozempic can temporarily worsen retinopathy in some cases. Signs of allergic reaction (rash, swelling, difficulty breathing) require emergency care—call 999 or go to A&E immediately.
For non-emergency concerns, contact your GP or diabetes team, or call NHS 111 for urgent advice when your regular healthcare providers are unavailable. For emergencies such as severe allergic reactions, severe hypoglycaemia with unconsciousness, or severe abdominal pain with systemic symptoms, call 999 or go to A&E.
If you suspect Ozempic has caused a side effect, you can report this through the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Frequently Asked Questions
Can I drink alcohol whilst taking Ozempic?
Yes, there is no absolute contraindication to drinking alcohol with Ozempic, but caution is advised. Follow UK guidelines of maximum 14 units weekly, always consume alcohol with food, stay well-hydrated, and monitor blood glucose levels, as both substances can affect glucose control and may worsen nausea.
Why does Ozempic cause nausea?
Ozempic causes nausea through two main mechanisms: it slows gastric emptying so food remains in the stomach longer, and it activates GLP-1 receptors in brain areas controlling nausea and satiety. This side effect affects approximately 20% of patients and typically improves over time with gradual dose titration.
When should I seek medical help for nausea on Ozempic?
Seek medical advice if nausea persists for more than a few days and interferes with eating or drinking, if you experience repeated vomiting preventing fluid retention, or if you develop signs of dehydration such as reduced urine output, dizziness, or confusion. Severe abdominal pain or hypoglycaemia symptoms require urgent assessment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript