Catabolism during fasting describes the body's natural process of breaking down stored energy reserves—glycogen, fat, and sometimes protein—to maintain vital functions when food intake ceases. This metabolic shift is a normal physiological adaptation, allowing survival during periods without nutrition. Understanding what catabolic means in fasting is essential for anyone considering intermittent or prolonged fasting, as the duration and individual health status significantly influence which energy stores are used and the potential health effects. Whilst short-term fasting may offer metabolic benefits for healthy adults, prolonged or poorly managed fasting can lead to muscle loss, nutrient deficiencies, and serious complications. This article explains the catabolic process, its phases, health implications, and how to manage fasting safely under appropriate guidance.
Summary: Catabolic in fasting means the body breaks down stored energy reserves—glycogen, fat, and protein—to maintain vital functions when food intake stops.
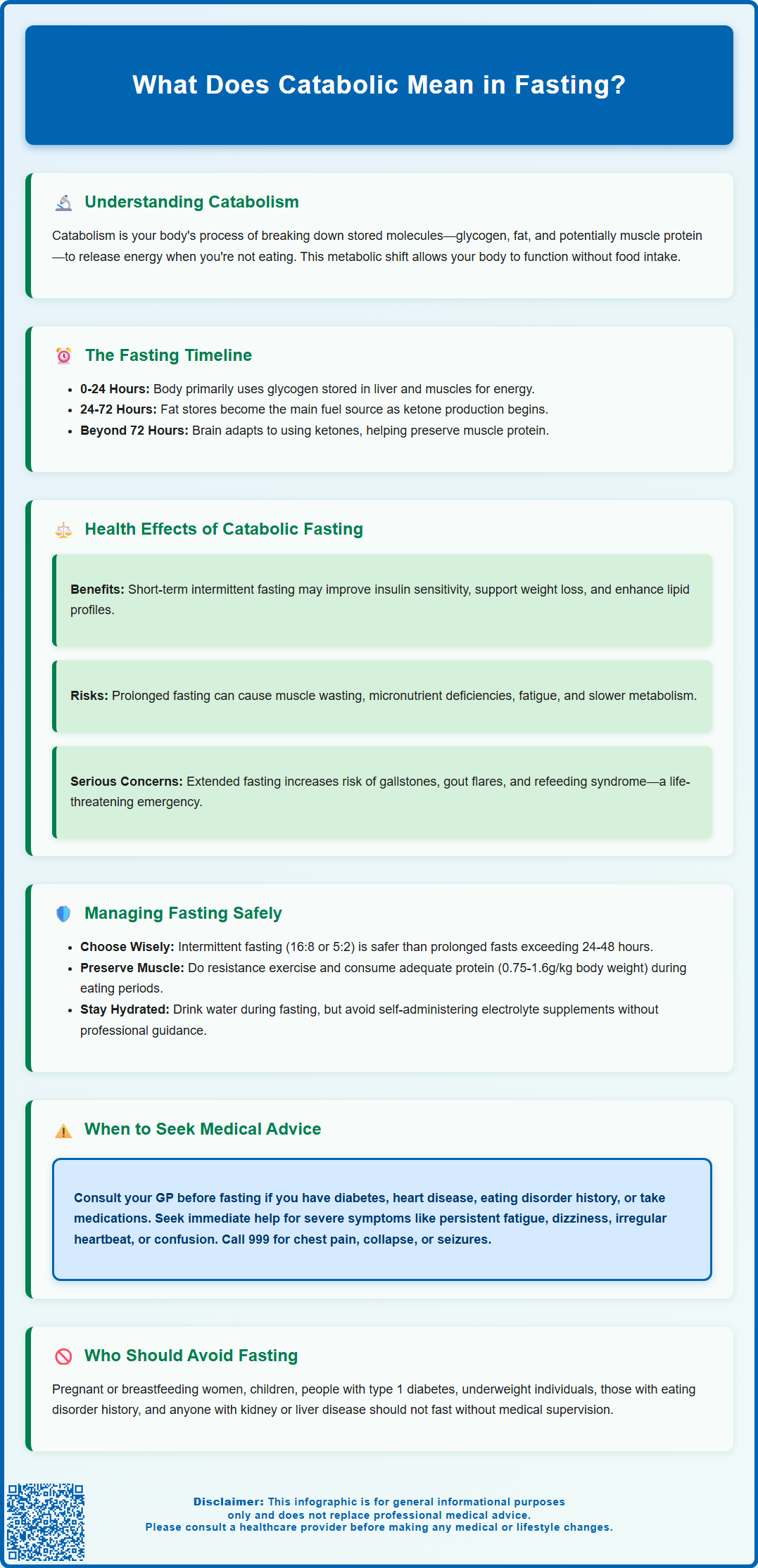
- Catabolism is a normal metabolic process where complex molecules are broken down into simpler ones to release energy during periods without food.
- The body progresses through phases: glycogen breakdown (0–24 hours), fat breakdown and ketone production (24–72 hours), then protein-sparing adaptation during prolonged fasting.
- Short-term intermittent fasting may improve insulin sensitivity and support weight management in healthy adults when done appropriately.
- Prolonged or poorly managed fasting can cause muscle wasting, micronutrient deficiencies, electrolyte imbalances, and refeeding syndrome requiring medical monitoring.
- Pregnant women, children, people with type 1 diabetes, eating disorders, or those who are underweight should not fast without medical supervision.
Table of Contents
What Does Catabolic Mean in Fasting?
Catabolism refers to the metabolic process whereby the body breaks down complex molecules into simpler ones to release energy. During fasting, when dietary intake ceases, the body must rely on its internal energy stores to maintain vital functions. This shift from using recently consumed nutrients (an anabolic state, where tissues are built) to breaking down stored reserves represents the transition into a catabolic state.
In practical terms, catabolism during fasting involves the breakdown of glycogen (stored carbohydrate in the liver and muscles), adipose tissue (fat stores), and—when fasting is prolonged or nutritional reserves are depleted—muscle protein. The body typically begins using liver glycogen within the first 12–24 hours of fasting, though this timing varies between individuals. Once glycogen stores diminish, the metabolic machinery shifts towards lipolysis (fat breakdown) and gluconeogenesis (the production of glucose from non-carbohydrate sources such as amino acids and glycerol).
It is important to understand that catabolism is a normal, adaptive physiological response. The body is designed to survive periods without food by mobilising energy reserves. However, the extent and duration of catabolism, and the specific substrates broken down, depend on factors including the length of the fast, the individual's nutritional status, activity level, and underlying health conditions. Short-term fasting (e.g., overnight or intermittent fasting) predominantly utilises glycogen and fat, whereas prolonged fasting without adequate nutritional support may lead to protein catabolism, which can have adverse health consequences.
Certain groups should not attempt fasting without medical guidance, including pregnant or breastfeeding women, children and adolescents, people with type 1 diabetes, those who are underweight or frail, and individuals with a history of eating disorders. If you're considering fasting for health reasons, the NHS and British Dietetic Association provide guidance on safe approaches to intermittent fasting and weight management.
How the Body Enters a Catabolic State During Fasting
The transition into a catabolic state during fasting follows a predictable metabolic sequence governed by hormonal and enzymatic changes. Initially, in the fed state, insulin levels are elevated, promoting glucose uptake and storage as glycogen, and inhibiting fat breakdown. As hours pass without food intake, insulin levels fall, and counter-regulatory hormones such as glucagon, cortisol, growth hormone, and adrenaline rise. These hormonal shifts signal the body to begin mobilising stored energy.
Phase 1: Glycogenolysis (0–24 hours) In the early fasting period, the liver releases glucose through glycogenolysis, the breakdown of glycogen into glucose molecules. This maintains blood glucose levels to supply the brain and red blood cells, which rely heavily on glucose. Muscle glycogen is also broken down, but it is used locally within muscle tissue and does not directly contribute to blood glucose.
Phase 2: Lipolysis and Ketogenesis (24–72 hours) As glycogen stores diminish, the body increasingly relies on lipolysis, the breakdown of triglycerides in adipose tissue into free fatty acids and glycerol. Fatty acids are transported to the liver and other tissues for oxidation (beta-oxidation), providing energy. The liver also converts fatty acids into ketone bodies (acetoacetate, beta-hydroxybutyrate, and acetone) through ketogenesis. Ketones begin to rise within 12–24 hours of fasting, with the brain starting to use them as an alternative fuel source after approximately 2–3 days, reducing the need for glucose and thereby helping to spare protein. Maximal ketone adaptation may take 1–2 weeks of sustained fasting.
Phase 3: Protein Metabolism During Prolonged Fasting (beyond 72 hours) During prolonged fasting, gluconeogenesis (glucose production from non-carbohydrate sources) begins early but changes in pattern over time. Initially, amino acids from muscle protein contribute significantly to glucose production. However, as ketone levels rise and tissues adapt to using ketones and fatty acids, the body becomes more protein-sparing. Protein breakdown typically decreases during this adaptation phase. If fasting continues for extended periods and fat stores become critically low, protein catabolism may increase again, which can lead to loss of lean body mass and functional impairment.
Health Effects of Catabolic Fasting on the Body
The health effects of catabolic fasting are highly variable and depend on the duration, frequency, and individual context. Short-term or intermittent fasting (e.g., 16:8 time-restricted eating or alternate-day fasting) is often safe for many healthy adults when done appropriately and may be associated with metabolic benefits, including improved insulin sensitivity, weight loss, and favourable changes in lipid profiles. Some research suggests these benefits may involve cellular repair processes such as autophagy (the removal of damaged cellular components), though evidence for significant autophagy benefits in humans remains preliminary, with most data coming from animal studies.
However, prolonged or poorly managed fasting can lead to adverse effects:
-
Muscle wasting: Excessive protein catabolism results in loss of skeletal muscle mass, which can impair physical function, reduce metabolic rate, and compromise immune function.
-
Micronutrient deficiencies: Extended fasting without supplementation may lead to deficiencies in vitamins (e.g., B vitamins, vitamin D) and minerals (e.g., potassium, magnesium, calcium), increasing the risk of conditions such as anaemia, bone loss, and electrolyte imbalances.
-
Fatigue and weakness: Depletion of energy reserves and muscle protein can cause significant fatigue, dizziness, and reduced exercise tolerance.
-
Metabolic adaptations: The body may lower its basal metabolic rate in response to prolonged energy restriction, which can hinder weight loss efforts and predispose to weight regain upon refeeding.
-
Gallstones: Rapid weight loss associated with prolonged fasting increases the risk of gallstone formation.
-
Gout flares: Fasting can temporarily increase uric acid levels, potentially triggering gout attacks in susceptible individuals.
-
Menstrual disturbances: Women may experience menstrual irregularities or amenorrhoea with prolonged or frequent fasting (Relative Energy Deficiency in Sport or RED-S).
-
Refeeding syndrome: Rapid reintroduction of food after prolonged fasting can cause dangerous shifts in electrolytes (particularly phosphate, potassium, and magnesium), leading to cardiac arrhythmias, respiratory failure, and neurological complications. This is a medical emergency requiring careful monitoring.
Certain populations are at higher risk of adverse effects from catabolic fasting, including individuals with diabetes (particularly type 1 diabetes at risk of diabetic ketoacidosis, or those taking SGLT2 inhibitors at risk of euglycaemic ketoacidosis), eating disorders, chronic kidney or liver disease, pregnant or breastfeeding women, children or adolescents, and those who are frail, underweight, or malnourished. Medical supervision is advised for those with underlying health conditions or those considering prolonged fasts.
Managing Catabolic States Safely During Fasting
Safe management of catabolic states during fasting requires careful planning, monitoring, and an understanding of individual health status. The following strategies can help minimise risks and optimise outcomes:
1. Choose an appropriate fasting regimen For most individuals, intermittent fasting protocols (e.g., 16:8 or 5:2 diets) are safer and more sustainable than prolonged fasting. These approaches allow regular nutrient intake while still providing potential metabolic benefits. Prolonged fasting (beyond 24–48 hours) should only be undertaken with medical supervision, particularly in individuals with pre-existing health conditions.
2. Maintain adequate hydration During fasting, continue to drink water regularly. For fasts longer than 24 hours, seek medical advice before considering electrolyte supplementation. Do not self-administer potassium or magnesium supplements unless specifically advised by a healthcare professional, as these can be dangerous. If concerned about dehydration, consult your GP who may recommend appropriate oral rehydration solutions if indicated.
3. Preserve muscle mass To minimise protein catabolism:
-
Engage in resistance exercise to stimulate muscle protein synthesis and signal the body to preserve lean mass.
-
Ensure adequate protein intake during eating windows. The UK Reference Nutrient Intake (RNI) is 0.75g/kg body weight per day, though active individuals and older adults may benefit from higher intakes (up to 1.2–1.6g/kg) under dietitian guidance.
-
Avoid combining fasting with severe calorie restriction, which accelerates muscle loss.
4. Monitor for warning signs Contact your GP or NHS 111 if you experience:
-
Severe fatigue, weakness, or dizziness
-
Persistent nausea or vomiting
-
Rapid or irregular heartbeat
-
Confusion or difficulty concentrating
-
Signs of hypoglycaemia (in individuals with diabetes)
Call 999 immediately for chest pain, collapse, severe confusion, seizures, or signs of severe dehydration.
5. Plan refeeding carefully After prolonged fasting, reintroduce food gradually, starting with small, easily digestible meals. Prioritise foods rich in natural electrolytes and avoid large, high-carbohydrate meals initially. Individuals at risk of refeeding syndrome (those with BMI <18.5, unintentional weight loss >10% in past 3-6 months, little or no nutritional intake for >5 days, or history of alcohol misuse or certain medications) should be monitored by healthcare professionals, with blood tests to check electrolyte levels and thiamine supplementation before refeeding begins, in line with NICE Clinical Guideline 32.
6. Consult healthcare professionals Before embarking on any fasting regimen, particularly if you have diabetes, cardiovascular disease, a history of eating disorders, or are taking medications, consult your GP or a registered dietitian. NICE guidance emphasises individualised approaches to weight management and metabolic health, and fasting may not be suitable for everyone. People with type 1 diabetes or those taking SGLT2 inhibitors should seek specific advice from their diabetes team, as fasting increases ketoacidosis risk. Regular follow-up can help ensure that fasting is conducted safely and effectively, with adjustments made as needed based on clinical monitoring.
If you experience any adverse effects that you suspect may be related to medicines or medical devices, please report them via the MHRA Yellow Card scheme (https://yellowcard.mhra.gov.uk/).
Frequently Asked Questions
How long does it take to enter a catabolic state during fasting?
The body begins breaking down glycogen stores within 12–24 hours of fasting, transitioning to fat breakdown and ketone production after 24–72 hours as glycogen depletes.
Does fasting always cause muscle loss?
Short-term intermittent fasting typically preserves muscle mass, especially with adequate protein intake and resistance exercise. Prolonged fasting without proper management increases the risk of muscle protein breakdown and loss of lean body mass.
Who should avoid fasting due to catabolic risks?
Pregnant or breastfeeding women, children, people with type 1 diabetes, those with eating disorders, individuals who are underweight or frail, and anyone with chronic health conditions should not fast without medical supervision due to increased risks from catabolic processes.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript