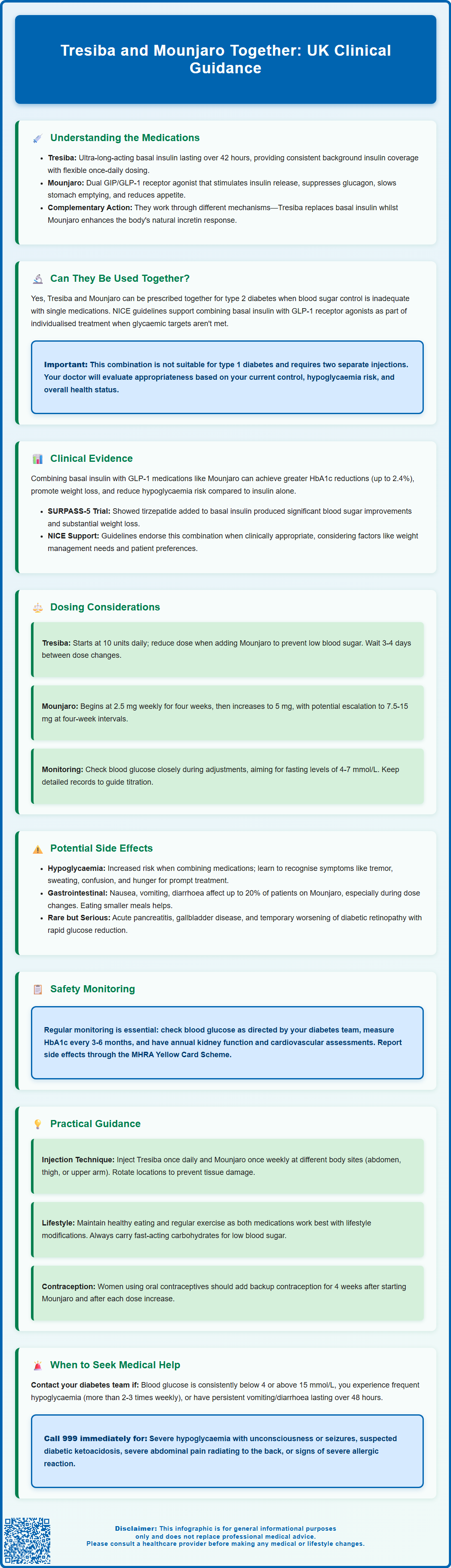
Tresiba (insulin degludec) and Mounjaro (tirzepatide) can be prescribed together for adults with type 2 diabetes when blood glucose control remains inadequate with single-agent therapy. This combination leverages two distinct mechanisms: Tresiba provides ultra-long-acting basal insulin replacement, whilst Mounjaro, a dual GIP/GLP-1 receptor agonist, enhances incretin-mediated glucose control and promotes weight loss. Understanding how these medications work together, appropriate dosing strategies, potential side effects, and practical management considerations is essential for patients and clinicians considering this treatment approach. This article explores the clinical evidence, UK guidance, and practical aspects of combining Tresiba and Mounjaro safely and effectively.
Summary: Tresiba and Mounjaro can be prescribed together for adults with type 2 diabetes when glycaemic control remains inadequate with either medication alone.
- Tresiba is an ultra-long-acting basal insulin providing consistent background glucose control over 42 hours
- Mounjaro is a dual GIP/GLP-1 receptor agonist that stimulates insulin secretion, suppresses glucagon, and promotes weight loss
- The combination addresses both insulin deficiency and impaired incretin function through complementary mechanisms
- Careful dose titration is essential, often requiring Tresiba reduction when adding Mounjaro to minimise hypoglycaemia risk
- Common side effects include hypoglycaemia and gastrointestinal symptoms requiring regular monitoring and clinical supervision
- This combination is not suitable for type 1 diabetes and requires assessment by diabetes specialists
Table of Contents
- Understanding Tresiba and Mounjaro: Mechanisms and Uses
- Can Tresiba and Mounjaro Be Used Together?
- Clinical Evidence and Guidelines for Combined Use
- Dosing Considerations and Adjustments
- Potential Side Effects and Safety Monitoring
- Practical Guidance for Patients Using Both Medications
- Frequently Asked Questions
Understanding Tresiba and Mounjaro: Mechanisms and Uses
Tresiba (insulin degludec) and Mounjaro (tirzepatide) represent two distinct classes of diabetes medications, each with unique mechanisms of action that address different aspects of glucose control.
Tresiba is an ultra-long-acting basal insulin analogue with a duration of action exceeding 42 hours. It works by binding to insulin receptors on cells throughout the body, facilitating glucose uptake from the bloodstream into tissues such as muscle and fat. This reduces blood glucose levels and provides consistent background insulin coverage. Tresiba is licensed in the UK for treating type 1 and type 2 diabetes mellitus in adults, adolescents, and children aged one year and above. Its extended half-life allows for flexible once-daily dosing, making it particularly suitable for patients requiring stable basal insulin replacement.
Mounjaro, by contrast, is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. This novel mechanism stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and promotes satiety. Mounjaro is indicated for adults with type 2 diabetes mellitus only, either as monotherapy when metformin is inappropriate or in combination with other glucose-lowering medications. It is not indicated for type 1 diabetes or for patients under 18 years of age. Clinical trials have demonstrated substantial HbA1c reductions and significant weight loss with tirzepatide therapy.
Whilst both medications lower blood glucose, their complementary mechanisms—Tresiba providing basal insulin replacement and Mounjaro enhancing incretin-mediated glucose control—mean they address different physiological deficits in type 2 diabetes. Understanding these distinct actions is fundamental to appreciating why combination therapy may be considered in certain clinical scenarios.
Can Tresiba and Mounjaro Be Used Together?
Yes, Tresiba and Mounjaro can be prescribed together for adults with type 2 diabetes when glycaemic control remains inadequate with either medication alone or with other oral antidiabetic agents. This combination is increasingly recognised in clinical practice, though it requires careful clinical assessment and monitoring.
The rationale for combining these agents stems from their complementary mechanisms. Patients with advanced type 2 diabetes often have both insulin deficiency (requiring basal insulin like Tresiba) and impaired incretin function (addressed by Mounjaro). When lifestyle modifications, metformin, and single-agent therapy fail to achieve target HbA1c levels, combination therapy may be appropriate.
NICE guidance on type 2 diabetes management (NG28) supports individualised treatment intensification when glycaemic targets are not met. Whilst NICE does not specifically mandate Tresiba-Mounjaro combinations, it acknowledges that basal insulin may be combined with GLP-1 receptor agonists in appropriate circumstances as part of individualised care. Mounjaro, as a dual GIP/GLP-1 receptor agonist, follows similar principles to established GLP-1 therapies that have been successfully combined with basal insulin.
However, this combination is not suitable for everyone. Mounjaro is not indicated for type 1 diabetes. Patients with severe gastrointestinal disease require careful evaluation. The UK product information for Mounjaro includes a precaution regarding thyroid C-cell tumours observed in rodent studies, and clinicians should exercise judgement when considering tirzepatide in patients with relevant thyroid conditions. Additionally, the decision to combine these medications should consider factors such as hypoglycaemia risk, patient preferences, treatment burden (two separate injections), and cost-effectiveness.
Your diabetes specialist or GP will assess whether this combination is appropriate based on your individual circumstances, current glycaemic control, other medications, and overall health status.
Clinical Evidence and Guidelines for Combined Use
The evidence base for combining basal insulin with incretin-based therapies has grown substantially over the past decade, though specific data on Tresiba and Mounjaro together remains limited due to Mounjaro's relatively recent introduction to the UK market.
Established evidence from trials such as DUAL studies (combining insulin degludec with liraglutide, another GLP-1 agonist) demonstrates that basal insulin plus incretin therapy can achieve superior HbA1c reductions compared to basal insulin alone, with additional benefits of weight loss or weight neutrality and reduced hypoglycaemia risk. While these findings provide indirect evidence, they have informed clinical practice regarding insulin-GLP-1 combinations more broadly.
For tirzepatide specifically, the SURPASS clinical trial programme evaluated its efficacy in various combinations, including with basal insulin. SURPASS-5 demonstrated that adding tirzepatide to insulin glargine (another basal insulin) produced significant HbA1c reductions (up to 2.4%) and substantial weight loss compared to placebo. This study used insulin glargine rather than Tresiba, but the principles likely apply across basal insulins given their comparable roles, though this represents indirect evidence for the specific degludec-tirzepatide combination.
NICE guidance NG28 recommends individualised treatment intensification for people with type 2 diabetes. While specific BMI thresholds apply to initiating GLP-1 receptor agonists as part of triple oral therapy, NICE supports combining GLP-1 receptor agonists with insulin where clinically appropriate as part of individualised care. Treatment decisions should consider factors including glycaemic targets, weight management needs, hypoglycaemia risk, and patient preferences.
The MHRA has approved both medications for use in type 2 diabetes, and there is no official contraindication to their combined use. However, prescribers must follow the Summary of Product Characteristics (SmPC) for each medication and exercise clinical judgement regarding appropriateness, monitoring requirements, and dose adjustments. The combination should be initiated and supervised by healthcare professionals experienced in diabetes management.
Dosing Considerations and Adjustments
When combining Tresiba and Mounjaro, careful dose titration and individualisation are essential to optimise glycaemic control whilst minimising adverse effects, particularly hypoglycaemia and gastrointestinal symptoms.
Tresiba dosing: Insulin degludec is typically initiated at 10 units once daily in insulin-naïve patients with type 2 diabetes, or at a unit-to-unit conversion from previous basal insulin. When adding Mounjaro to existing Tresiba therapy, consider reducing the Tresiba dose to mitigate hypoglycaemia risk, as tirzepatide's glucose-lowering effects will contribute to overall glycaemic control. The reduction should be guided by current glucose levels and clinician judgement. Subsequent adjustments should be based on self-monitored blood glucose readings, typically targeting fasting glucose levels of 4–7 mmol/L. Tresiba can be administered at any time of day, though consistency is advisable.
Mounjaro dosing: Tirzepatide follows a structured dose-escalation schedule to improve gastrointestinal tolerability. Treatment begins at 2.5 mg subcutaneously once weekly for four weeks, then increases to 5 mg weekly. Further escalation to 7.5 mg, 10 mg, 12.5 mg, or 15 mg may occur at four-week intervals based on glycaemic response and tolerability. The 2.5 mg dose is for treatment initiation only and is not therapeutic. When adding Mounjaro to existing Tresiba, the standard escalation schedule should be followed.
Key considerations:
-
Both medications are administered subcutaneously but at different frequencies (Tresiba daily, Mounjaro weekly)
-
Injection sites should be rotated to prevent lipohypertrophy
-
Dose adjustments should not be made more frequently than every 3–4 days for Tresiba to allow steady-state achievement
-
Patients should maintain detailed glucose monitoring records during titration
-
For tirzepatide, no specific dose adjustment is needed in renal impairment; for insulin degludec, requirements may decrease in renal impairment—monitor closely and adjust as needed
-
Tirzepatide may reduce the efficacy of oral contraceptives; additional contraception is recommended for 4 weeks after initiation and after each dose increase
Your diabetes team will provide specific dosing instructions tailored to your individual needs, previous treatment response, and glucose monitoring data.
Potential Side Effects and Safety Monitoring
Understanding potential adverse effects and implementing appropriate monitoring strategies are crucial when using Tresiba and Mounjaro together.
Hypoglycaemia represents a significant concern with this combination. While tirzepatide has a glucose-dependent mechanism, when used with insulin the hypoglycaemia risk may increase unless insulin doses are appropriately reduced. Symptoms include tremor, sweating, anxiety, hunger, palpitations, and confusion. Severe hypoglycaemia (requiring third-party assistance) requires immediate treatment with fast-acting carbohydrates or glucagon. Patients should be educated on recognising and managing hypoglycaemia, particularly during dose titration or with changes in diet, exercise, or concurrent illness.
Gastrointestinal side effects are common with Mounjaro, particularly during initiation and dose escalation. These include nausea (reported in up to 20% of patients), vomiting, diarrhoea, constipation, and abdominal discomfort. Symptoms typically diminish over time. Eating smaller, more frequent meals and avoiding high-fat foods may help. Persistent or severe gastrointestinal symptoms warrant medical review, as they may indicate pancreatitis (rare but serious), gallbladder disease, or other complications. Severe gastrointestinal symptoms can lead to dehydration and potential acute kidney injury.
Injection site reactions—including redness, itching, or swelling—can occur with both medications but are generally mild and transient. Rotating injection sites reduces this risk.
Other considerations:
-
Thyroid concerns: The UK product information for Mounjaro includes a precaution regarding thyroid C-cell tumours observed in rodent studies. Clinical significance in humans is unknown, but clinicians should exercise judgement in patients with relevant thyroid conditions
-
Pancreatitis: Acute pancreatitis has been reported with GLP-1 receptor agonists. Persistent severe abdominal pain requires immediate medical attention
-
Gallbladder disease: Tirzepatide may increase the risk of gallstones. Seek medical advice for persistent upper abdominal pain with fever or jaundice
-
Diabetic retinopathy: Rapid glucose reduction may temporarily worsen retinopathy; patients with pre-existing retinopathy require ophthalmological monitoring
-
Weight changes: Mounjaro typically causes weight loss, which is often beneficial but should be monitored
Recommended monitoring includes:
-
Regular blood glucose monitoring (frequency determined by your diabetes team)
-
HbA1c measurement every 3–6 months
-
Annual review of renal function, lipids, and cardiovascular risk factors
-
Regular assessment for hypoglycaemia frequency and severity
-
Monitoring for gastrointestinal symptoms and weight changes
If you experience any suspected side effects, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Practical Guidance for Patients Using Both Medications
Successfully managing diabetes with both Tresiba and Mounjaro requires understanding practical aspects of administration, lifestyle integration, and when to seek medical advice.
Administration technique:
-
Both medications are administered via subcutaneous injection using pre-filled pens
-
Tresiba is injected once daily at the same time each day (though timing can be flexible if needed)
-
Mounjaro is injected once weekly on the same day each week
-
Injection sites include the abdomen, thigh, or upper arm—rotate sites to prevent tissue changes
-
Both medications can be injected at the same time but in different injection sites
-
Storage: Unopened pens should be refrigerated (2–8°C); Tresiba in-use pens can be kept at room temperature (below 30°C) for up to 8 weeks; Mounjaro pens are single-use and can be kept at room temperature (not above 30°C) for up to 30 days—do not freeze either medication
-
Never share injection pens, even if the needle is changed
Lifestyle considerations:
-
Continue following dietary advice from your diabetes team—both medications work best alongside healthy eating patterns
-
Regular physical activity enhances glucose control but may increase hypoglycaemia risk; monitor glucose before, during, and after exercise
-
Alcohol can affect blood glucose levels; consume in moderation and never on an empty stomach
-
Carry fast-acting carbohydrates (glucose tablets, sugary drinks) to treat hypoglycaemia
-
Wear medical identification indicating you have diabetes and use insulin
-
If you drive, be aware of DVLA rules for insulin-treated diabetes and check current guidance regarding monitoring and hypoglycaemia
-
If using oral contraceptives, use additional contraception for 4 weeks after starting Mounjaro and after each dose increase
When to contact your GP or diabetes team:
-
Blood glucose consistently <4 mmol/L or >15 mmol/L
-
Frequent hypoglycaemic episodes (more than 2–3 per week)
-
Severe hypoglycaemia requiring assistance
-
Persistent nausea, vomiting, or diarrhoea lasting more than 48 hours
-
Severe abdominal pain (potential pancreatitis or gallbladder disease)
-
Signs of infection or illness (may require dose adjustments)
-
Pregnancy or planning pregnancy (treatment requires modification)
-
Any concerns about side effects or medication management
Emergency situations requiring immediate medical attention (999 or A&E):
-
Severe hypoglycaemia with loss of consciousness or seizures
-
Suspected diabetic ketoacidosis (persistent high glucose, vomiting, abdominal pain, fruity breath odour)
-
Severe persistent abdominal pain radiating to the back
-
Signs of severe allergic reaction (difficulty breathing, facial swelling)
Regular communication with your diabetes healthcare team ensures optimal management and allows for timely adjustments to your treatment plan based on your individual response and changing needs.
Frequently Asked Questions
Is it safe to use Tresiba and Mounjaro at the same time?
Yes, when prescribed by a diabetes specialist, Tresiba and Mounjaro can be used together safely for type 2 diabetes. Careful monitoring for hypoglycaemia and gastrointestinal side effects is essential, and insulin doses often require adjustment when starting Mounjaro.
How do I inject both Tresiba and Mounjaro?
Tresiba is injected once daily at the same time each day, whilst Mounjaro is injected once weekly on the same day each week. Both can be administered at the same time but must be injected at different sites on the abdomen, thigh, or upper arm.
Will I need to reduce my Tresiba dose when starting Mounjaro?
Often yes—your diabetes team will typically reduce your Tresiba dose when adding Mounjaro to minimise hypoglycaemia risk, as tirzepatide contributes additional glucose-lowering effects. Dose adjustments are individualised based on blood glucose monitoring.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










