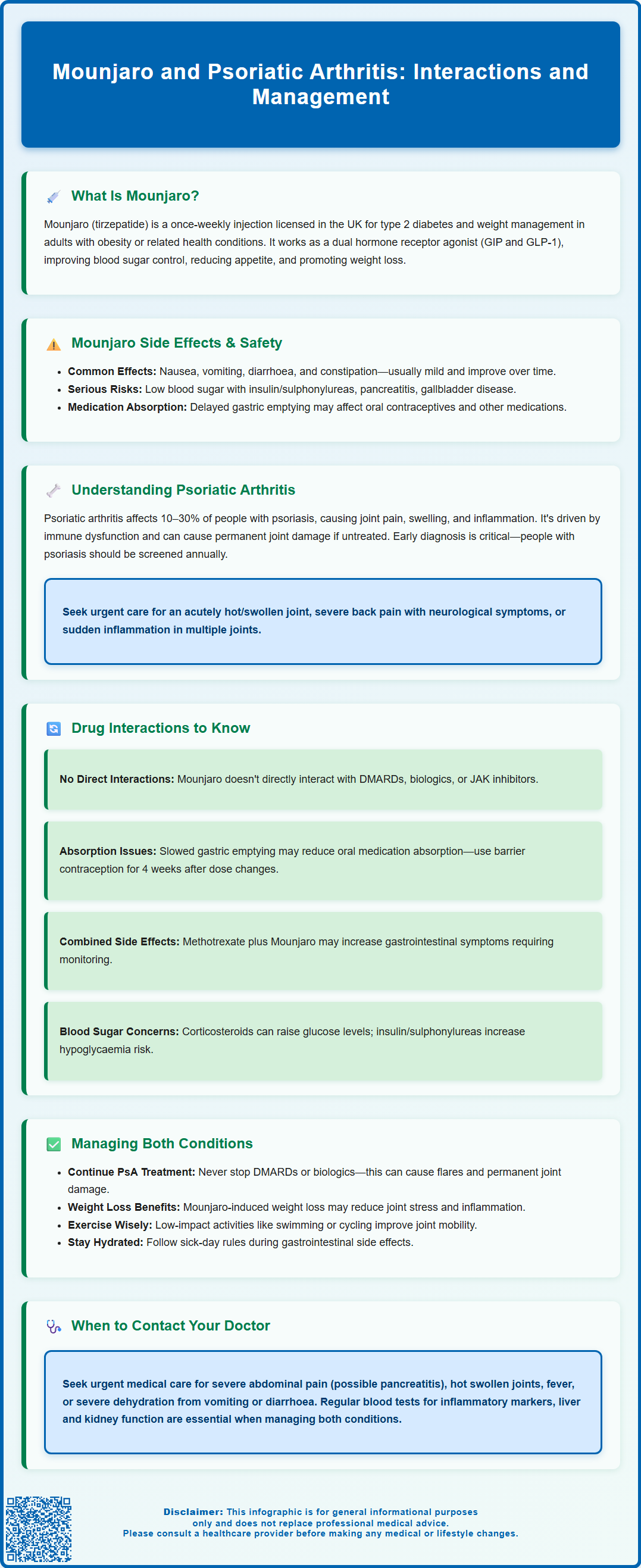
Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management, not for inflammatory conditions such as psoriatic arthritis. Psoriatic arthritis (PsA) is a chronic inflammatory arthropathy affecting joints, entheses, and the spine in people with psoriasis, requiring disease-modifying treatments to prevent irreversible damage. Whilst Mounjaro and PsA medications do not have direct pharmacokinetic interactions, managing both conditions concurrently requires careful coordination between specialists. This article explores the mechanisms of Mounjaro, the nature of psoriatic arthritis, potential medication considerations, and practical guidance for patients managing both conditions under medical supervision.
Summary: Mounjaro (tirzepatide) is not licensed to treat psoriatic arthritis and has no direct interactions with PsA medications, but concurrent use requires specialist coordination and monitoring.
- Mounjaro is a dual GIP/GLP-1 receptor agonist licensed for type 2 diabetes and weight management, not inflammatory arthritis.
- Psoriatic arthritis requires disease-modifying drugs or biologics targeting TNF-α, IL-17, or IL-23 to prevent joint damage.
- No direct pharmacokinetic interactions exist between tirzepatide and DMARDs, biologics, or JAK inhibitors used for PsA.
- Mounjaro delays gastric emptying, potentially affecting oral medication absorption including contraceptives and narrow therapeutic index drugs.
- Patients must continue prescribed PsA treatments and report severe abdominal pain, hot swollen joints, or persistent vomiting urgently to healthcare providers.
Table of Contents
What Is Mounjaro and How Does It Work?
Mounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. It is administered as a once-weekly subcutaneous injection and is available through the NHS for eligible patients who meet specific criteria outlined by the National Institute for Health and Care Excellence (NICE). For weight management, this typically includes a BMI threshold and treatment within specialist weight management services.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist. This means it mimics the action of two naturally occurring incretin hormones that play crucial roles in glucose regulation and appetite control. By activating GIP receptors, Mounjaro enhances insulin secretion and may improve insulin sensitivity. Simultaneously, GLP-1 receptor activation stimulates insulin release in response to elevated blood glucose, suppresses glucagon secretion (which reduces glucose production by the liver), slows gastric emptying, and promotes satiety—leading to reduced caloric intake.
The combined action on both receptor pathways results in improved glycaemic control and significant weight loss. Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, which are typically mild to moderate and diminish over time. Patients are advised to start at a low dose with gradual titration to minimise these effects.
Important safety considerations include:
-
Risk of hypoglycaemia when used with insulin or sulfonylureas (dose adjustments may be needed)
-
Pancreatitis risk (seek urgent medical attention for severe abdominal pain)
-
Gallbladder disease (including cholelithiasis and cholecystitis)
-
Delayed gastric emptying affecting absorption of oral medicines, particularly oral contraceptives
-
Caution in diabetic retinopathy, especially with rapid improvement in glucose control
-
Not recommended during pregnancy or breastfeeding
It is important to note that Mounjaro is not licensed for the treatment of inflammatory conditions such as psoriatic arthritis. Its use is specifically indicated for metabolic conditions, and any off-label use should be discussed thoroughly with a healthcare professional.
Understanding Psoriatic Arthritis: Symptoms and Causes
Psoriatic arthritis (PsA) is a chronic inflammatory arthropathy that occurs in approximately 10–30% of individuals with psoriasis, a skin condition characterised by red, scaly plaques. PsA is classified as a seronegative spondyloarthropathy, meaning it typically does not produce rheumatoid factor antibodies. The condition can affect peripheral joints, the spine, and entheses (sites where tendons and ligaments attach to bone), leading to pain, stiffness, swelling, and progressive joint damage if left untreated.
Common symptoms of psoriatic arthritis include:
-
Joint pain and swelling, often asymmetric and affecting fingers, toes, knees, and ankles
-
Dactylitis (sausage-like swelling of entire digits)
-
Enthesitis (inflammation at tendon and ligament insertion points, such as the Achilles tendon or plantar fascia)
-
Axial involvement with inflammatory back pain and stiffness
-
Nail changes, including pitting, onycholysis, and hyperkeratosis
-
Fatigue and reduced quality of life
The aetiology of PsA is multifactorial, involving genetic predisposition (particularly HLA-B27 and other HLA alleles), environmental triggers, and immune dysregulation. The pathophysiology centres on aberrant activation of the immune system, with elevated levels of pro-inflammatory cytokines such as tumour necrosis factor-alpha (TNF-α), interleukin-17 (IL-17), and interleukin-23 (IL-23). These cytokines drive synovial inflammation, bone erosion, and new bone formation.
Early diagnosis and treatment are essential to prevent irreversible joint damage. NICE recommends urgent referral to a rheumatologist if PsA is suspected, with local services typically aiming for assessment within 3 weeks of referral. People with psoriasis should be screened annually for PsA using validated tools such as the Psoriasis Epidemiology Screening Tool (PEST).
Diagnosis is primarily clinical, supported by imaging (X-rays, ultrasound, or MRI) and exclusion of other arthropathies. There is no single diagnostic test for PsA, and inflammatory markers (ESR, CRP) may be normal in some patients.
Red flags requiring immediate medical attention include:
-
Acute hot, swollen joint (possible septic arthritis)
-
Severe back pain with neurological symptoms
-
Sudden onset of multiple joint inflammation
Potential Interactions Between Mounjaro and Arthritis Medications
Patients with psoriatic arthritis often require disease-modifying antirheumatic drugs (DMARDs), biologic therapies, or Janus kinase (JAK) inhibitors to control inflammation and prevent joint damage. While there are no known direct pharmacokinetic interactions between tirzepatide and commonly used PsA treatments, several considerations are important when using these medications concurrently.
Conventional DMARDs such as methotrexate, sulfasalazine, and leflunomide are metabolised primarily by the liver and kidneys. Mounjaro does not significantly affect hepatic enzyme activity or renal clearance pathways. However, both methotrexate and Mounjaro can cause gastrointestinal side effects, which may be additive. Patients should be monitored for nausea, vomiting, or diarrhoea, and dose adjustments or symptomatic management may be required.
Biologic agents targeting TNF-α (such as adalimumab, etanercept, infliximab), IL-17 (secukinumab, ixekizumab), or IL-23 (guselkumab, risankizumab) work via immune modulation and do not share metabolic pathways with tirzepatide. There is no known pharmacokinetic interaction. Both biologics and GLP-1 receptor agonists have been associated with injection site reactions, and patients using multiple injectable therapies should rotate sites appropriately.
JAK inhibitors (tofacitinib, upadacitinib) are oral medications metabolised by cytochrome P450 enzymes. Mounjaro does not induce or inhibit these enzymes, so interactions are not anticipated.
Important interaction considerations:
-
Delayed gastric emptying: Mounjaro slows gastric emptying, which may affect the absorption of oral medications. This is particularly important for drugs with a narrow therapeutic index or those requiring rapid absorption for efficacy. Oral contraceptives may have reduced effectiveness; additional barrier contraception is advised for 4 weeks after starting Mounjaro and after each dose increase.
-
Hypoglycaemia risk: If used with insulin or sulfonylureas, there is an increased risk of hypoglycaemia. Dose reductions of these medications may be necessary, and blood glucose should be monitored closely.
-
Corticosteroids (prednisolone, dexamethasone) are sometimes used for short-term control of PsA flares. These can raise blood glucose levels, potentially counteracting the glycaemic benefits of Mounjaro. Patients with diabetes taking both medications should monitor blood glucose closely.
Overall, while direct interactions are unlikely, polypharmacy increases the complexity of care. Patients should maintain an up-to-date medication list and ensure all prescribers are aware of concurrent treatments. Report any suspected adverse drug reactions to the MHRA via the Yellow Card scheme (yellowcard.mhra.gov.uk).
Managing Psoriatic Arthritis While Taking Mounjaro
Effective management of psoriatic arthritis in patients taking Mounjaro requires a multidisciplinary approach involving rheumatologists, GPs, diabetes or weight management specialists, and allied health professionals. The primary goals are to control inflammation, preserve joint function, optimise metabolic health, and maintain quality of life.
Medication adherence is paramount. Patients should continue their prescribed DMARD or biologic therapy as directed, even if they experience weight loss or improved metabolic parameters on Mounjaro. Discontinuing anti-inflammatory treatment prematurely can lead to disease flares and irreversible joint damage. If gastrointestinal side effects from Mounjaro are troublesome, discuss strategies such as dose titration, dietary modifications, or anti-emetic medications with your healthcare provider rather than stopping treatment abruptly.
Lifestyle modifications play a crucial role in managing both conditions. Weight loss achieved through Mounjaro may reduce mechanical stress on weight-bearing joints and decrease systemic inflammation, potentially improving PsA symptoms. Regular low-impact exercise such as swimming, cycling, or yoga can enhance joint mobility, strengthen supporting muscles, and improve cardiovascular health without exacerbating joint pain. Physiotherapy referrals should be considered for tailored exercise programmes.
Dietary considerations are also important. A balanced diet such as a Mediterranean-style eating pattern with plenty of fruits, vegetables, whole grains, lean proteins, and healthy fats may support both metabolic and joint health, though evidence for specific anti-inflammatory effects varies. Limiting processed foods, refined sugars, and saturated fats can help optimise weight management. Patients should be cautious with alcohol, as it can interact with methotrexate and other DMARDs, and may affect blood glucose control.
Hydration and sick-day management are essential, particularly if experiencing gastrointestinal side effects. Maintain adequate fluid intake to prevent dehydration and acute kidney injury. During episodes of severe vomiting or diarrhoea, follow local sick-day rules, which may include temporarily pausing certain medications (such as methotrexate, ACE inhibitors, or diuretics) as advised by your healthcare team.
Monitoring and follow-up are essential. Regular blood tests to assess inflammatory markers (CRP, ESR), liver and kidney function, and metabolic parameters (HbA1c, lipid profile) should be conducted as recommended by your healthcare team.
When to seek medical advice:
- Urgent medical attention needed for:
- Severe, persistent abdominal pain (especially radiating to the back) which could indicate pancreatitis
- Acute hot, swollen joint (possible infection)
- Signs of infection (fever, chills, unexplained malaise)
-
Severe dehydration from persistent vomiting or diarrhoea
-
Routine follow-up for:
- Worsening joint pain or swelling
- Persistent mild to moderate gastrointestinal issues
- Difficulty managing blood glucose levels
- Questions about family planning (Mounjaro is not recommended during pregnancy)
Patients should feel empowered to discuss any concerns with their GP or specialist. There is no evidence that Mounjaro worsens psoriatic arthritis, but individualised care and open communication are key to achieving optimal outcomes in managing both conditions concurrently. Report any suspected side effects via the MHRA Yellow Card scheme.
Frequently Asked Questions
Can Mounjaro be used to treat psoriatic arthritis?
No, Mounjaro (tirzepatide) is not licensed for psoriatic arthritis. It is approved in the UK only for type 2 diabetes and weight management in adults with obesity or overweight with weight-related comorbidities.
Does Mounjaro interact with biologic medications for psoriatic arthritis?
There are no known direct pharmacokinetic interactions between Mounjaro and biologic therapies such as TNF-α, IL-17, or IL-23 inhibitors. However, patients using multiple injectable therapies should rotate injection sites appropriately and maintain regular monitoring with their healthcare team.
Should I stop my psoriatic arthritis medication if I start Mounjaro?
No, you should continue your prescribed DMARD or biologic therapy as directed by your rheumatologist. Discontinuing anti-inflammatory treatment can lead to disease flares and irreversible joint damage, even if you experience weight loss or improved metabolic health on Mounjaro.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript