Mounjaro and Lantus together can be an effective combination for managing type 2 diabetes when blood glucose control remains suboptimal with basal insulin alone. Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist that enhances glucose-dependent insulin secretion and promotes weight loss, whilst Lantus (insulin glargine) is a long-acting basal insulin providing steady background glucose control. These medications work through complementary mechanisms and are increasingly prescribed together under specialist supervision. This combination requires careful dose adjustment, particularly of insulin, to minimise hypoglycaemia risk whilst optimising glycaemic control. Understanding how these medications interact, appropriate monitoring requirements, and when to seek medical advice is essential for safe and effective diabetes management.
Summary: Mounjaro and Lantus can be prescribed together under medical supervision for type 2 diabetes, with insulin dose reduction typically required to minimise hypoglycaemia risk.
- Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist; Lantus (insulin glargine) is a long-acting basal insulin with complementary mechanisms of action.
- Combination therapy requires careful insulin dose adjustment, typically around 20% reduction when Mounjaro is added, with individualised titration based on glucose monitoring.
- Hypoglycaemia is the most significant risk, primarily from the insulin component, requiring regular blood glucose monitoring and prompt treatment of low readings below 4 mmol/L.
- Gastrointestinal side effects (nausea, vomiting, diarrhoea) are common with Mounjaro, particularly during dose escalation, and usually diminish over time.
- Regular monitoring includes HbA1c every 3–6 months, renal function, weight, blood pressure, injection sites, and diabetic retinopathy screening.
- Contact your diabetes team for recurrent hypoglycaemia, persistent hyperglycaemia, severe abdominal pain, or before pregnancy, surgery, or starting new medications.
Table of Contents
Can You Take Mounjaro and Lantus Together?
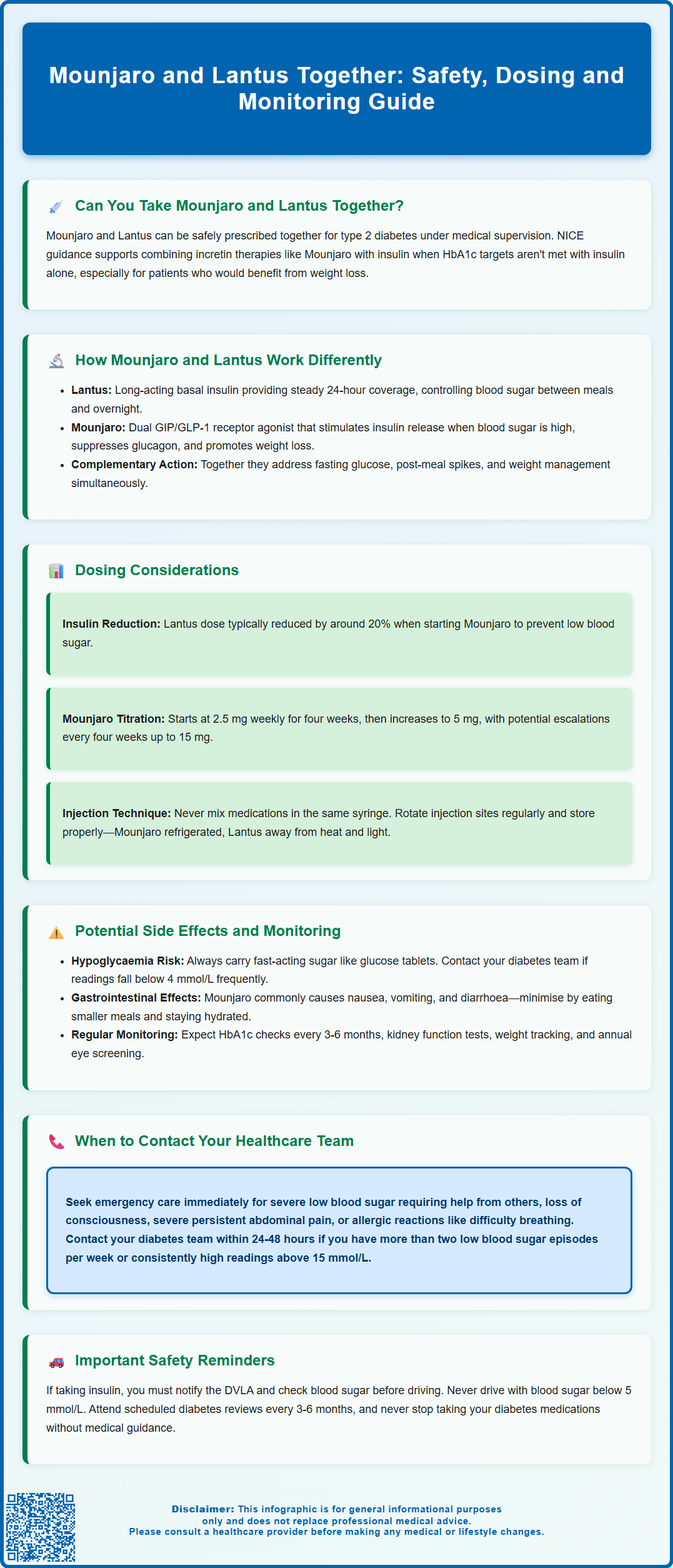
Yes, Mounjaro (tirzepatide) and Lantus (insulin glargine) can be prescribed together under appropriate medical supervision. Mounjaro is licensed for adults with type 2 diabetes and can be used with insulin according to its UK product licence. This combination is increasingly used in the management of type 2 diabetes when blood glucose control remains suboptimal with basal insulin alone. The decision to combine these medications is made on an individual basis by your diabetes specialist or GP, taking into account your current glycaemic control, weight, cardiovascular risk factors, and treatment goals.
Mounjaro is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, whilst Lantus is a long-acting basal insulin analogue. These medications work through complementary mechanisms, which can provide additive benefits for glucose management. NICE guidance (NG28) supports the use of incretin therapies alongside insulin in specific contexts and under specialist advice when HbA1c targets are not achieved with insulin therapy alone, particularly in individuals who would benefit from weight loss.
When initiating this combination, your healthcare team will carefully assess your current insulin requirements, recent blood glucose patterns, and any history of hypoglycaemia. The addition of Mounjaro to an existing Lantus regimen typically requires adjustment of your insulin dose to reduce the risk of low blood sugar episodes. It is essential that you do not start, stop, or adjust either medication without consulting your prescriber, as both drugs significantly affect blood glucose levels and require coordinated management. Your diabetes team will provide specific guidance on dose titration, monitoring schedules, and what to expect during the initial weeks of combination therapy.
How Mounjaro and Lantus Work Differently
Understanding the distinct mechanisms of action of Mounjaro and Lantus helps explain why they can be used effectively together. Lantus (insulin glargine) is a long-acting basal insulin that provides a steady, peakless release of insulin over approximately 24 hours. It works by directly replacing or supplementing the body's natural background insulin production, helping to control blood glucose levels between meals and overnight. Lantus acts by binding to insulin receptors on cells throughout the body, facilitating glucose uptake from the bloodstream into tissues such as muscle and fat, whilst also suppressing excessive glucose production by the liver.
Mounjaro (tirzepatide) operates through an entirely different mechanism. As a dual GIP/GLP-1 receptor agonist, it mimics the action of incretin hormones that are naturally released by the gut in response to food intake. Mounjaro enhances glucose-dependent insulin secretion from pancreatic beta cells, meaning it stimulates insulin release only when blood glucose levels are elevated, thereby reducing hypoglycaemia risk. Additionally, it suppresses glucagon secretion (a hormone that raises blood glucose), slows gastric emptying to moderate post-meal glucose spikes, and acts on brain appetite centres to promote satiety and weight loss.
The complementary nature of these mechanisms means that Mounjaro addresses both fasting and post-meal glucose control whilst promoting weight loss, whereas Lantus primarily targets fasting and between-meal glucose levels. Mounjaro's glucose-dependent action provides a safety advantage, as it does not typically cause hypoglycaemia when used alone. However, when combined with Lantus, the insulin component can still cause low blood sugar, necessitating careful dose adjustment. This combination approach aligns with contemporary diabetes management strategies that address multiple pathophysiological defects simultaneously, potentially improving overall glycaemic control whilst managing weight—a significant concern for many individuals with type 2 diabetes.
Dosing Considerations When Combining Mounjaro and Lantus
When Mounjaro is added to an existing Lantus regimen, insulin dose reduction is typically considered to minimise hypoglycaemia risk. UK diabetes specialists often suggest an empiric basal insulin reduction (around 20%, particularly if your HbA1c is near target), though individual adjustments vary based on current glycaemic control, insulin sensitivity, and hypoglycaemia history. Your diabetes team will provide specific instructions tailored to your circumstances, and these initial reductions are provisional—further adjustments will be made based on your blood glucose monitoring results.
Mounjaro is initiated at a starting dose of 2.5 mg once weekly via subcutaneous injection, administered on the same day each week. This dose serves primarily as a tolerability step rather than a therapeutic dose. After four weeks, the dose is increased to 5 mg weekly, with subsequent escalations every four weeks (to 7.5 mg, 10 mg, 12.5 mg, and potentially 15 mg) based on glycaemic response and tolerability. Lantus dosing is highly individualised, typically administered once daily at the same time each day, with doses ranging from 10 units to over 100 units depending on individual insulin requirements.
Important: Mounjaro delays gastric emptying and may reduce the absorption of oral medications, including oral contraceptives. If you use oral contraceptives, you should use additional contraception for 4 weeks after starting Mounjaro and for 4 weeks after each dose increase.
Self-monitoring of blood glucose becomes particularly important during the initial combination period and following any dose adjustments. Your healthcare team will advise on testing frequency, but typically this includes fasting glucose measurements and periodic pre-meal or bedtime checks. Keep a record of your readings, noting any patterns of hypoglycaemia or persistent hyperglycaemia. Both medications are administered by subcutaneous injection and require rotation of injection sites to prevent lipohypertrophy (fatty lumps under the skin) which can affect medication absorption. Mounjaro is typically injected in the abdomen, thigh, or upper arm, whilst Lantus is commonly administered in the abdomen or thigh. Never mix these medications in the same syringe, and store both according to manufacturer instructions—unused Mounjaro pens in the refrigerator (in-use pens up to 30 days at room temperature), and Lantus (in-use pens up to 4 weeks at room temperature) away from direct heat and light.
Potential Side Effects and Monitoring Requirements
The most significant risk when combining Mounjaro and Lantus is hypoglycaemia (low blood sugar), primarily attributable to the Lantus component. Symptoms include trembling, sweating, confusion, palpitations, hunger, and irritability. Severe hypoglycaemia can lead to loss of consciousness or seizures. Your diabetes team will provide guidance on recognising and treating hypoglycaemia with fast-acting carbohydrates (such as glucose tablets, sugary drinks, or jellies), followed by a longer-acting carbohydrate once symptoms resolve. Always carry a form of fast-acting sugar and ensure family members or colleagues know how to assist you if needed. If you experience recurrent hypoglycaemia (more than one episode requiring assistance, or frequent readings below 4 mmol/L), contact your diabetes team promptly for dose adjustment.
Gastrointestinal side effects are common with Mounjaro, particularly during dose escalation. These include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. These effects are usually mild to moderate and tend to diminish over time as your body adjusts to the medication. To minimise gastrointestinal symptoms, eat smaller, more frequent meals, avoid high-fat foods, and stay well hydrated. If vomiting or diarrhoea is severe or persistent, contact your healthcare team, as dehydration can affect kidney function.
Diabetic retinopathy caution: Rapid improvement in blood glucose control may be associated with temporary worsening of diabetic retinopathy, particularly in people already taking insulin. If you have pre-existing retinopathy, ensure you attend regular eye screening and report any visual changes promptly.
Gallbladder disease: Mounjaro has been associated with an increased risk of gallbladder problems, including gallstones and inflammation of the gallbladder. Seek medical advice if you develop symptoms such as severe abdominal pain in the upper right side, fever, or yellowing of the skin or eyes.
Regular monitoring is essential when taking this combination. Your healthcare team will schedule periodic reviews to assess:
-
HbA1c levels (typically every 3–6 months) to evaluate overall glucose control
-
Renal function (eGFR and creatinine) – insulin requirements may decrease with declining kidney function, and kidney function should be monitored if severe gastrointestinal side effects occur with Mounjaro
-
Weight and body mass index, as Mounjaro typically promotes weight loss
-
Blood pressure and cardiovascular risk factors
-
Injection site examination for signs of lipohypertrophy or infection
-
Eye screening for diabetic retinopathy
Additional considerations include potential pancreatitis risk with Mounjaro. Seek immediate medical attention if you develop severe, persistent abdominal pain that may radiate to the back, accompanied by nausea and vomiting. There is also a theoretical risk of thyroid C-cell tumours based on animal studies, though no definitive link has been established in humans. Report any neck lumps, hoarseness, or difficulty swallowing to your GP. Both medications can cause injection site reactions such as redness, itching, or swelling, which are usually mild and self-limiting.
If you experience any suspected side effects, you can report them via the Yellow Card Scheme at yellowcard.mhra.gov.uk.
When to Contact Your Healthcare Team
Certain situations require prompt communication with your diabetes team or GP. Contact them within 24–48 hours if you experience recurrent hypoglycaemia (more than two episodes per week with blood glucose below 4 mmol/L), persistent hyperglycaemia (blood glucose consistently above 15 mmol/L despite medication adherence), or if you're uncertain about dose adjustments during illness or changes in routine. Your team can provide guidance on temporary insulin dose modifications and sick-day rules, which are particularly important when combining these medications.
Seek same-day medical advice or attend A&E if you develop:
-
Severe hypoglycaemia requiring assistance from another person, loss of consciousness, or seizures
-
Diabetic ketoacidosis symptoms: excessive thirst, frequent urination, fruity-smelling breath, confusion, or rapid breathing (though less common in type 2 diabetes, it can occur)
-
Severe abdominal pain that is persistent and may indicate pancreatitis or gallbladder disease
-
Signs of severe dehydration: dizziness, reduced urine output, confusion, or rapid heartbeat
-
Allergic reactions: difficulty breathing, facial swelling, or widespread rash
Routine situations that warrant scheduled contact include:
-
Planning pregnancy or discovering you are pregnant, as both medications require specialist review and potential adjustment
-
Scheduling surgery or procedures requiring fasting, as medication timing and doses need modification
-
Starting new medications that may interact with glucose control (such as corticosteroids, certain antibiotics, or other diabetes medications)
-
Experiencing persistent gastrointestinal side effects that affect your quality of life or ability to maintain adequate nutrition
-
Noticing unexplained weight loss beyond expected effects, persistent fatigue, or other concerning symptoms
DVLA and driving advice: If you are taking insulin, you must inform the DVLA. Check your blood glucose before driving and every 2 hours on longer journeys. Do not drive if your blood glucose is below 5 mmol/L. Always carry hypo treatment in the vehicle and take breaks on longer journeys. Be aware of the legal requirements for insulin-treated drivers, which your diabetes team can explain.
Maintain regular contact with your diabetes team through scheduled reviews, typically every 3–6 months, or more frequently during initial combination therapy. These appointments allow for medication optimisation, complication screening, and discussion of treatment goals. Keep an up-to-date list of all medications, including over-the-counter products and supplements, and bring your blood glucose monitoring records to appointments. Never discontinue either medication without medical guidance, as abrupt cessation can lead to dangerous glucose fluctuations. Your diabetes team is your partner in managing this combination therapy safely and effectively, so maintain open communication about your experiences, concerns, and treatment goals.
Frequently Asked Questions
Do I need to reduce my Lantus dose when starting Mounjaro?
Yes, insulin dose reduction is typically recommended when adding Mounjaro to Lantus, often around 20% reduction, though this varies individually. Your diabetes team will provide specific guidance based on your current glycaemic control and hypoglycaemia history, with further adjustments made according to your blood glucose monitoring results.
What is the main risk of taking Mounjaro and Lantus together?
The most significant risk is hypoglycaemia (low blood sugar below 4 mmol/L), primarily from the Lantus component. Regular blood glucose monitoring is essential, and you should carry fast-acting carbohydrates at all times and contact your diabetes team if you experience recurrent low readings.
Can I inject Mounjaro and Lantus at the same time?
Whilst both are subcutaneous injections, they must never be mixed in the same syringe and should be administered as separate injections. You should rotate injection sites to prevent lipohypertrophy, and both medications can be given on the same day according to their respective schedules (Mounjaro weekly, Lantus daily).
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript