Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with related health conditions. Whilst the medication has well-documented side effects—primarily gastrointestinal disturbances—vaginal bleeding or spotting is not listed as a recognised adverse reaction in MHRA or EMA prescribing information. If you experience vaginal spotting whilst taking Saxenda, it is essential to seek medical assessment, as this symptom warrants investigation to identify the underlying cause and exclude other important conditions, rather than assuming a link to the medication.
Summary: Vaginal bleeding or spotting is not a recognised side effect of Saxenda according to UK regulatory data.
- Saxenda (liraglutide) is a GLP-1 receptor agonist licensed for weight management in adults with obesity or overweight with related conditions
- The medication has no established direct effect on sex hormone regulation or the reproductive system
- Weight loss itself can influence menstrual patterns and potentially cause changes in bleeding, independent of medication
- Any unexplained vaginal bleeding requires medical assessment to exclude pregnancy, infection, structural abnormalities, or other underlying causes
- Postmenopausal bleeding or persistent intermenstrual bleeding warrants urgent referral according to NICE guidance
Table of Contents
Understanding Saxenda and Potential Side Effects
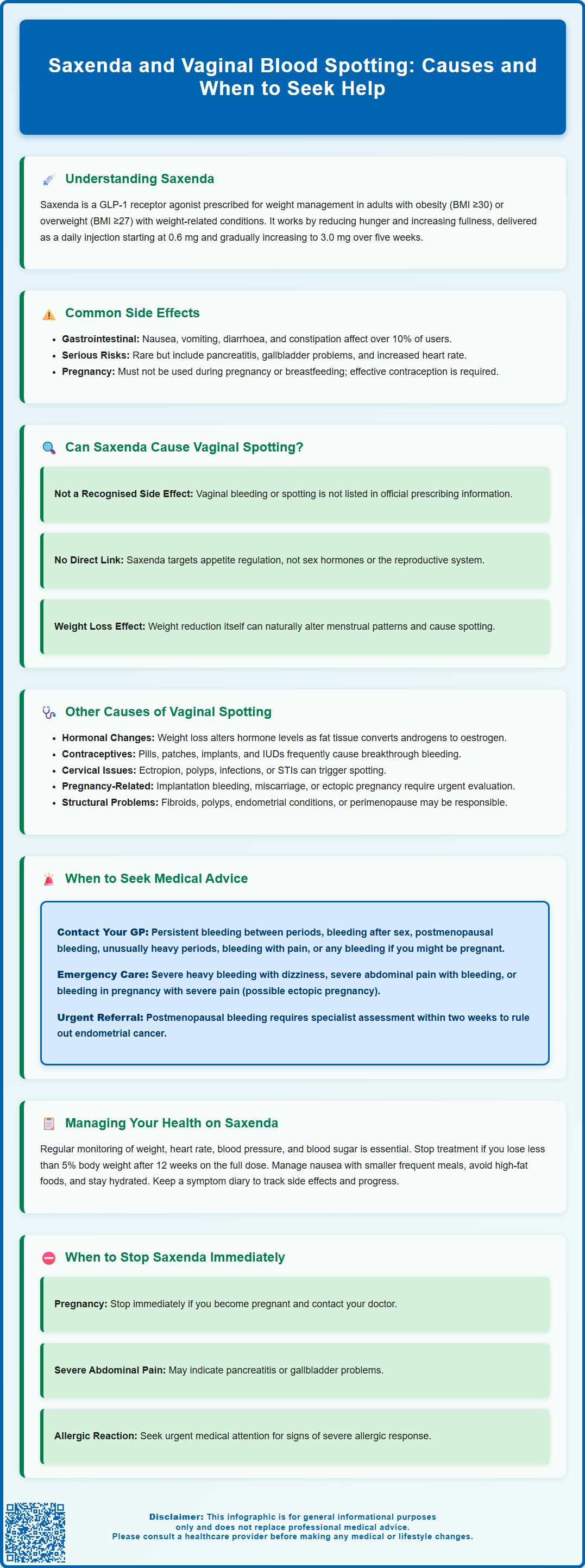
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with weight-related health conditions such as type 2 diabetes, hypertension, or dyslipidaemia. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking a naturally occurring hormone that regulates appetite and food intake.
The mechanism of action involves binding to GLP-1 receptors in the brain, particularly in areas that control appetite and satiety. This leads to reduced hunger, increased feelings of fullness after eating, delayed gastric emptying, and consequently lower calorie intake. Saxenda is administered as a once-daily subcutaneous injection, typically starting at a low dose (0.6 mg) and gradually increasing over five weeks to the maintenance dose of 3.0 mg daily. This titration schedule helps minimise gastrointestinal side effects.
Common side effects of Saxenda include nausea, vomiting, diarrhoea, constipation, headache, and injection site reactions. These effects are usually mild to moderate and tend to improve as the body adjusts to the medication. According to the MHRA-approved Summary of Product Characteristics, gastrointestinal disturbances are the most frequently reported adverse reactions, affecting more than 10% of users.
Less common but more serious side effects can include pancreatitis, gallbladder problems, increased heart rate, and hypoglycaemia (particularly in patients taking insulin or sulfonylureas). The medicine also carries warnings regarding thyroid tumours based on animal studies, though the relevance to humans remains uncertain.
Saxenda should not be used during pregnancy or breastfeeding. If you become pregnant while taking Saxenda, the medication should be discontinued. Women of childbearing potential should use effective contraception while on treatment. Patients should be counselled about recognising symptoms of serious adverse effects and the importance of regular monitoring whilst on treatment.
Can Saxenda Cause Vaginal Bleeding or Spotting?
Vaginal bleeding or spotting is not listed as a recognised side effect in the official prescribing information for Saxenda approved by the MHRA or EMA. The Summary of Product Characteristics does not identify menstrual disturbances, intermenstrual bleeding, or vaginal spotting among the documented adverse reactions associated with liraglutide use for weight management.
It is important to understand that there is no established causal link between Saxenda and vaginal bleeding. The absence of this side effect in clinical trial data and post-marketing surveillance suggests that it is not a recognised adverse reaction to the medication.
GLP-1 receptor agonists like Saxenda primarily affect the gastrointestinal system and central nervous system pathways involved in appetite regulation. The medication has no established direct effect on sex hormone regulation or the reproductive system in the way that hormonal contraceptives or other endocrine medications do. The drug's mechanism of action does not involve known interaction with oestrogen, progesterone, or other sex hormones that regulate menstruation.
That said, weight loss itself can influence menstrual patterns and potentially cause changes in bleeding patterns, which may be mistakenly attributed to the medication rather than the weight reduction process. Additionally, any new symptom occurring during treatment should be evaluated properly to rule out other underlying causes. If you experience vaginal bleeding or spotting whilst taking Saxenda, it is essential to consult your GP for appropriate assessment, including a pregnancy test if pregnancy is possible, as this symptom warrants investigation regardless of whether you are taking weight loss medication.
Other Causes of Vaginal Spotting During Weight Loss Treatment
When experiencing vaginal spotting during weight loss treatment, it is crucial to consider alternative explanations that may be more likely than a direct medication effect. Significant weight loss, regardless of the method used to achieve it, can have profound effects on reproductive hormones and menstrual function.
Hormonal changes associated with weight loss are well-documented. Adipose (fat) tissue plays an active role in hormone metabolism, particularly in the conversion of androgens to oestrogens through the enzyme aromatase. As body fat decreases, this can alter circulating hormone levels, potentially leading to irregular bleeding, spotting between periods, or changes in menstrual flow and frequency. Women with polycystic ovary syndrome (PCOS) may notice particular changes in their cycles as weight loss improves insulin sensitivity and hormonal balance.
Other common causes of vaginal spotting include:
-
Contraceptive methods: Hormonal contraceptives (pills, patches, implants, or intrauterine systems) frequently cause breakthrough bleeding or spotting, especially during the first few months of use or when doses are missed
-
Cervical causes: Cervical ectropion, polyps, or inflammation can cause spotting, particularly after intercourse
-
Infection: Sexually transmitted infections or pelvic inflammatory disease may present with abnormal bleeding
-
Pregnancy-related causes: Implantation bleeding, miscarriage, or ectopic pregnancy must be considered in women of reproductive age
-
Structural abnormalities: Uterine fibroids, endometrial polyps, or adenomyosis can cause intermenstrual bleeding
-
Endometrial causes: Endometrial hyperplasia or, rarely, endometrial cancer should be considered, particularly in women over 45 or those with risk factors
-
Perimenopause: Hormonal fluctuations during perimenopause commonly cause irregular bleeding patterns
-
Medications: Anticoagulants, antithrombotics, and certain other medications can contribute to abnormal bleeding
-
Thyroid dysfunction: Both hypothyroidism and hyperthyroidism can affect menstrual patterns
-
Bleeding disorders: Underlying coagulation abnormalities may present with abnormal bleeding
A thorough medical assessment is necessary to identify the underlying cause of any abnormal vaginal bleeding, ensuring appropriate management and excluding serious conditions.
When to Seek Medical Advice About Vaginal Bleeding
Prompt medical evaluation is essential for any unexplained vaginal bleeding or spotting, particularly if it represents a change from your normal pattern. Whilst occasional light spotting may not always indicate a serious problem, certain features warrant urgent assessment.
You should contact your GP if you experience:
-
Vaginal bleeding between periods that is persistent or recurrent
-
Bleeding after sexual intercourse (post-coital bleeding)
-
Bleeding after menopause (any vaginal bleeding occurring 12 months or more after your last period)
-
Unusually heavy periods or bleeding that soaks through sanitary protection within one to two hours
-
Bleeding accompanied by abdominal or pelvic pain
-
Any bleeding if you could be pregnant or have a positive pregnancy test
Seek emergency care (call 999 or go to A&E) if you have:
-
Severe, heavy bleeding with signs of shock (dizziness, fainting, rapid heartbeat)
-
Severe abdominal pain with bleeding
-
Bleeding in pregnancy with severe pain (possible ectopic pregnancy)
According to NICE guidance (NG12), postmenopausal bleeding should be referred urgently (within two weeks) for specialist assessment to exclude endometrial cancer. Similarly, persistent intermenstrual bleeding in women aged 45 years or over, or in younger women with additional risk factors, may require investigation including pelvic examination, cervical screening (if due), and potentially transvaginal ultrasound or endometrial biopsy.
When consulting your doctor, be prepared to provide information about:
-
The timing, duration, and amount of bleeding
-
Your menstrual history and last menstrual period
-
Current medications, including Saxenda and any contraceptives
-
Sexual history and contraceptive use
-
Associated symptoms such as pain, discharge, or systemic features
Your GP will conduct an appropriate assessment, which may include physical examination, pregnancy testing, cervical screening, blood tests, or imaging studies to determine the cause and guide management. They may refer you to a sexual health clinic, gynaecology service, or advise contacting NHS 111 or an urgent treatment centre if needed. Do not assume that bleeding is related to your weight loss medication without proper medical evaluation to exclude other important causes.
Managing Side Effects and Monitoring Your Health on Saxenda
Effective management of Saxenda treatment requires regular monitoring and open communication with your healthcare team. Patients prescribed weight loss medications should receive ongoing support and review to assess treatment response, tolerability, and overall health.
Regular monitoring should include:
-
Weight and BMI measurements: Typically assessed monthly initially, then at least every three months. According to the Saxenda Summary of Product Characteristics, treatment should be discontinued if less than 5% weight loss is achieved after 12 weeks on the maintenance dose of 3.0 mg daily
-
Blood pressure and heart rate: Saxenda can increase heart rate, so cardiovascular parameters should be monitored regularly
-
Blood glucose levels: Particularly important for patients with type 2 diabetes or prediabetes, as weight loss and GLP-1 agonist effects can improve glycaemic control
-
Lipid profile and other metabolic markers: To assess improvement in cardiovascular risk factors
-
Mental health and wellbeing: Weight loss can affect mood, and any concerns about depression or suicidal thoughts should be reported immediately
Managing common gastrointestinal side effects involves eating smaller, more frequent meals, avoiding high-fat foods, staying well-hydrated, and allowing time for your body to adjust to each dose increase. If nausea is severe, your doctor may recommend slowing the dose escalation or prescribing short-term anti-sickness medication.
Important safety considerations:
-
Saxenda should not be used during pregnancy or breastfeeding. If you become pregnant, stop the medication and inform your GP immediately
-
Women of childbearing potential should use effective contraception while taking Saxenda
-
Saxenda should not be used in combination with other GLP-1 receptor agonists
-
Be alert for symptoms of pancreatitis (severe, persistent abdominal pain radiating to the back), gallbladder problems (right upper abdominal pain, particularly after eating), or allergic reactions
-
If you suspect you are experiencing side effects from Saxenda, you can report them via the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk or through the Yellow Card app
Maintaining a symptom diary can be helpful for tracking side effects, identifying patterns, and discussing concerns with your healthcare team. This should include details of any unusual symptoms, including changes in menstrual patterns or vaginal bleeding, even if they seem unrelated to the medication. Remember that Saxenda is most effective when combined with a reduced-calorie diet and increased physical activity, and your healthcare team can provide support with lifestyle modifications alongside medication management.
Frequently Asked Questions
Is vaginal spotting a known side effect of Saxenda?
No, vaginal bleeding or spotting is not listed as a recognised side effect in the MHRA or EMA prescribing information for Saxenda. There is no established causal link between liraglutide and vaginal bleeding.
Can weight loss from Saxenda affect my menstrual cycle?
Yes, significant weight loss can influence menstrual patterns through hormonal changes, as adipose tissue plays an active role in hormone metabolism. This may lead to irregular bleeding or spotting independent of the medication itself.
When should I see a doctor about vaginal spotting whilst taking Saxenda?
You should contact your GP for any unexplained vaginal bleeding between periods, post-coital bleeding, postmenopausal bleeding, or bleeding accompanied by pain. Seek emergency care for severe heavy bleeding with signs of shock or severe abdominal pain.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










