Saxenda and ADHD medication can both play important roles in managing distinct health conditions, but many patients wonder whether these treatments can be safely combined. Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed for weight management, whilst ADHD medications—including stimulants like methylphenidate and non-stimulants such as atomoxetine—help control attention, impulsivity, and hyperactivity. There is no absolute contraindication to using these medications together, but concurrent use requires careful medical supervision due to overlapping effects on appetite, cardiovascular function, and metabolic parameters. This article examines the mechanisms of both medication classes, potential interactions, safety considerations, and guidance for patients considering or currently using Saxenda alongside ADHD treatment.
Summary: Saxenda can be used alongside ADHD medication with no absolute contraindication, but concurrent use requires individualised medical assessment and close monitoring due to overlapping effects on appetite and cardiovascular function.
- Saxenda is a GLP-1 receptor agonist that reduces appetite and promotes weight loss through brain receptors controlling hunger.
- ADHD medications include stimulants (methylphenidate, lisdexamfetamine) and non-stimulants (atomoxetine, guanfacine) that modulate dopamine and noradrenaline.
- Both medication classes can suppress appetite and affect cardiovascular parameters, necessitating monitoring of nutritional intake, heart rate, and blood pressure.
- Saxenda slows gastric emptying, which may theoretically alter absorption of oral ADHD medications, though clinically significant interactions have not been established.
- Treatment decisions must be individualised by healthcare professionals, with coordination between GP, ADHD specialist, and weight management services where appropriate.
- Regular monitoring should include cardiovascular parameters, nutritional adequacy, ADHD symptom control, and adverse effects from either medication.
Table of Contents
- What Is Saxenda and How Does It Work?
- Common ADHD Medications and Their Mechanisms
- Can You Take Saxenda with ADHD Medication?
- Potential Interactions Between Saxenda and ADHD Drugs
- Safety Considerations and Medical Guidance
- Managing Weight and ADHD: Treatment Options
- Scientific References
- Frequently Asked Questions
What Is Saxenda and How Does It Work?
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, such as type 2 diabetes or hypertension. It is also licensed for adolescents aged 12 years and above with obesity under specific criteria. Saxenda is administered as a once-daily subcutaneous injection and is intended to be used alongside a reduced-calorie diet and increased physical activity.
Saxenda belongs to a class of medicines called glucagon-like peptide-1 (GLP-1) receptor agonists. It works by mimicking the action of GLP-1, a naturally occurring hormone that regulates appetite and food intake. The medication acts on specific receptors in the brain—particularly in areas that control appetite—to increase feelings of fullness and reduce hunger. This mechanism helps patients consume fewer calories, leading to gradual weight loss over time.
Treatment with Saxenda begins with a dose titration schedule, starting at 0.6 mg daily and increasing by 0.6 mg weekly until reaching the maintenance dose of 3.0 mg daily. Treatment is typically reviewed after 12 weeks at the 3.0 mg dose, and continuation depends on achieving at least 5% weight loss during this period.
Saxenda received European authorisation via the European Medicines Agency (EMA) in 2015 and is available in the UK. NHS access is governed by NICE Technology Appraisal 664, which specifies that it should be prescribed by specialist weight management services for adults with a BMI of at least 35 kg/m² (or 32.5 kg/m² for certain ethnic groups) and at least one weight-related comorbidity, who have engaged with a weight management programme for at least 12 weeks. NHS treatment is typically limited to a maximum of 2 years.
Common side effects include nausea, diarrhoea, constipation, and vomiting, which often improve as the body adjusts to the medication. Patients should be aware of the risk of pancreatitis and gallbladder disease. Saxenda should not be used concurrently with other GLP-1 receptor agonists. It is important to note that Saxenda is not a quick fix for weight loss. Adherence to dietary changes and physical activity remains essential for optimal outcomes.
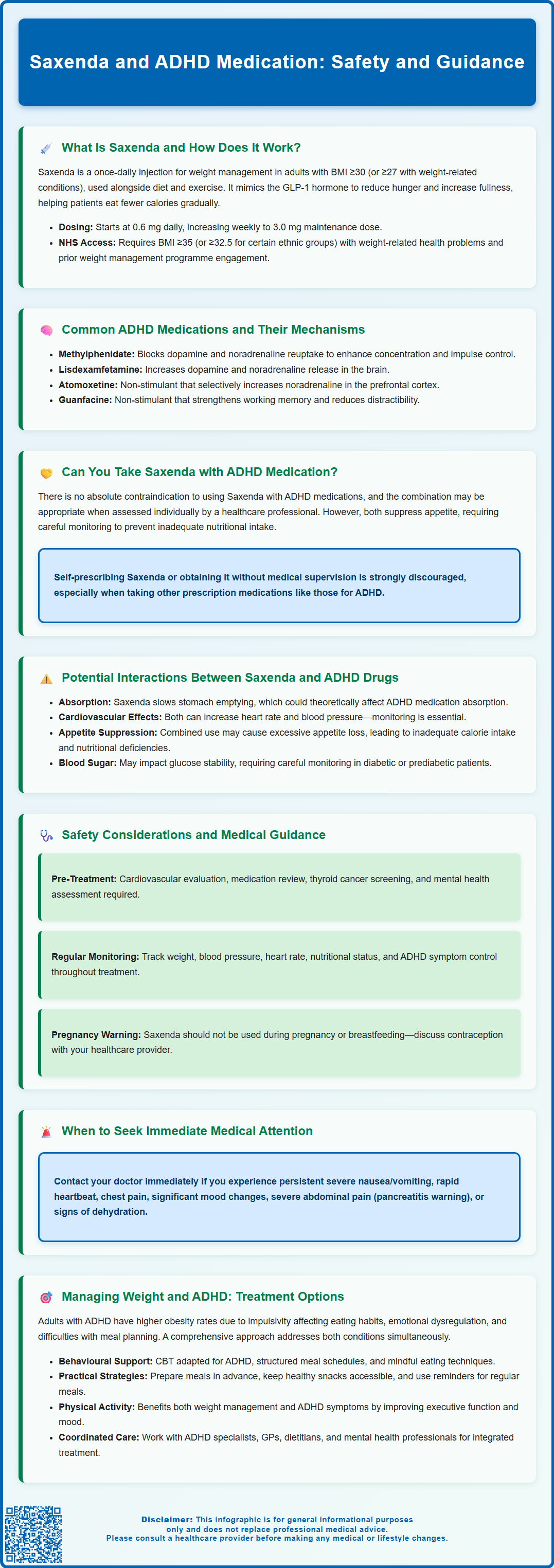
Common ADHD Medications and Their Mechanisms
Attention deficit hyperactivity disorder (ADHD) is managed in the UK with several classes of medication, each working through distinct mechanisms to improve symptoms such as inattention, hyperactivity, and impulsivity. The choice of medication depends on individual patient factors, symptom severity, and response to treatment.
Stimulant medications are the most commonly prescribed ADHD treatments and include:
-
Methylphenidate (e.g., Concerta XL, Medikinet, Equasym): Works by blocking the reuptake of dopamine and noradrenaline in the brain, increasing the availability of these neurotransmitters in the synaptic cleft. This enhances concentration, attention, and impulse control.
-
Lisdexamfetamine (Elvanse): A prodrug that is converted to dexamfetamine in the body. It primarily increases dopamine and noradrenaline levels through enhanced release of these neurotransmitters, with reuptake inhibition as a secondary mechanism.
Non-stimulant medications are alternatives for patients who do not respond to or cannot tolerate stimulants:
-
Atomoxetine (Strattera): A selective noradrenaline reuptake inhibitor that increases noradrenaline levels in the prefrontal cortex, improving attention and reducing impulsivity without the stimulant effects.
-
Guanfacine (Intuniv): An alpha-2A adrenergic receptor agonist that strengthens working memory and reduces distractibility by modulating neurotransmitter activity in the prefrontal cortex.
According to NICE guidelines (NG87), medication should be offered as part of a comprehensive treatment plan that includes psychological, behavioural, and educational interventions. Regular monitoring for efficacy and adverse effects—including cardiovascular parameters, growth in children, and mental health—is essential throughout ADHD treatment.
Can You Take Saxenda with ADHD Medication?
Many patients with ADHD also struggle with weight management, leading to questions about whether Saxenda can be safely used alongside ADHD medications. There is no absolute contraindication to using Saxenda with ADHD medications, and concurrent use may be appropriate in certain clinical situations. The Summary of Product Characteristics (SmPC) for Saxenda does not list ADHD medications as contraindicated, and there are no formal warnings against their combined use. Similarly, the prescribing information for most ADHD medications does not specifically prohibit concurrent use with GLP-1 receptor agonists like Saxenda.
However, this decision must be made on an individual basis by a healthcare professional who can assess the specific circumstances, medications involved, and overall health status.
Both medication classes can affect appetite, cardiovascular function, and metabolic parameters, which necessitates careful consideration. Some ADHD medications, particularly stimulants, are known to suppress appetite and may contribute to weight loss, whilst Saxenda is specifically designed to reduce appetite and promote weight loss. The combined appetite-suppressing effects could potentially lead to inadequate nutritional intake if not properly monitored.
Before starting Saxenda whilst taking ADHD medication, patients should have a thorough discussion with their prescribing doctor or specialist. This conversation should cover:
-
Current ADHD medication regimen and dosage
-
Weight management goals and previous attempts
-
Cardiovascular health status
-
Eating patterns and nutritional adequacy
-
Potential monitoring requirements
Optimal care involves coordination between the patient's GP, ADHD specialist, and weight management service where NHS care is involved. Self-prescribing or obtaining Saxenda without medical supervision is strongly discouraged, particularly when taking other prescription medications.
Potential Interactions Between Saxenda and ADHD Drugs
Whilst there are no well-documented direct pharmacological interactions between Saxenda and ADHD medications, several considerations warrant attention when these treatments are used together. Understanding potential indirect effects and overlapping side effect profiles is essential for safe concurrent use.
Gastrointestinal effects and medication absorption: Saxenda slows gastric emptying, which is part of its mechanism for promoting satiety. This effect could theoretically alter the absorption rate of oral ADHD medications, particularly immediate-release formulations. However, the Saxenda SmPC notes that clinically significant interactions affecting the absorption of oral medications have not been established in studies. Modified-release preparations of methylphenidate or lisdexamfetamine are designed to release medication over extended periods and may be less susceptible to absorption changes.
Cardiovascular considerations: Both stimulant ADHD medications and Saxenda can affect heart rate and blood pressure. Stimulants typically increase heart rate and may elevate blood pressure, whilst Saxenda has been associated with modest increases in resting heart rate (average 2–3 beats per minute in clinical trials). Guanfacine, however, may lower blood pressure and heart rate, which could potentially mask some cardiovascular effects of other medications. When used together, cardiovascular monitoring becomes particularly important, especially in patients with pre-existing cardiovascular conditions or risk factors.
Appetite suppression and nutritional intake: The combined appetite-suppressing effects of both medication classes could lead to inadequate caloric or nutritional intake. This is particularly relevant with stimulant ADHD medications, which are well known for reducing appetite. Patients may experience:
-
Difficulty consuming adequate calories
-
Unintentional excessive weight loss
-
Nutritional deficiencies
-
Fatigue or weakness
Blood glucose effects: Saxenda can lower blood glucose levels, and whilst ADHD medications do not typically have direct effects on glucose metabolism, the combined impact on eating patterns could affect blood sugar stability. Patients with diabetes or prediabetes require particularly careful monitoring.
Regular follow-up appointments are essential to assess tolerance, efficacy, and any emerging concerns when these medications are used concurrently.
Safety Considerations and Medical Guidance
When considering or using Saxenda alongside ADHD medication, several important safety considerations must be addressed to minimise risks and optimise treatment outcomes. Close medical supervision is essential throughout the treatment period.
Pre-treatment assessment should include:
-
Comprehensive cardiovascular evaluation, including blood pressure and heart rate measurement
-
Assessment of eating patterns, nutritional status, and weight history
-
Review of all current medications and supplements
-
Screening for hypersensitivity to liraglutide or any excipients (the only absolute contraindication in the UK SmPC)
-
Consideration of precautions including personal or family history of medullary thyroid carcinoma and multiple endocrine neoplasia syndrome type 2
-
Evaluation of renal and hepatic function (caution is advised in severe impairment)
-
Mental health assessment, as both ADHD and obesity can be associated with mood disorders
-
Discussion of contraception for women of childbearing potential, as Saxenda should not be used during pregnancy and is not recommended during breastfeeding
Ongoing monitoring should encompass:
-
Regular weight and BMI measurements
-
Cardiovascular parameters (blood pressure and heart rate) at each visit
-
Assessment of nutritional adequacy and eating patterns
-
Monitoring for adverse effects from either medication
-
Evaluation of ADHD symptom control
-
Blood glucose monitoring if diabetic or at risk
When to contact your GP or healthcare provider:
-
Persistent or severe nausea, vomiting, or abdominal pain
-
Signs of dehydration (dark urine, dizziness, reduced urination)
-
Rapid or irregular heartbeat, chest pain, or shortness of breath
-
Significant mood changes, depression, or suicidal thoughts
-
Symptoms of pancreatitis (severe upper abdominal pain radiating to the back)
-
Signs of gallbladder problems (right upper quadrant pain, fever, jaundice)
-
Difficulty maintaining adequate food or fluid intake
-
Unintentional excessive weight loss
NICE guidance on obesity management (CG189) emphasises the importance of a multidisciplinary approach. Patients using Saxenda should continue to receive support for dietary modification, physical activity, and behavioural strategies. Similarly, ADHD management should continue to include appropriate psychological and educational interventions alongside medication.
Patients should never adjust doses of either medication without consulting their healthcare provider, and any new symptoms should be reported promptly. Suspected adverse reactions can be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Managing Weight and ADHD: Treatment Options
The relationship between ADHD and weight management is complex, and individuals with ADHD face unique challenges that may require tailored approaches. Research suggests that adults with ADHD have higher rates of obesity compared to the general population, potentially due to factors such as impulsivity affecting eating behaviours, emotional dysregulation, and executive function difficulties with meal planning and routine.
Comprehensive weight management strategies for people with ADHD should address both conditions holistically:
Behavioural and psychological interventions: Cognitive behavioural therapy (CBT) adapted for ADHD can help address impulsive eating, emotional eating, and difficulties with planning and organisation. Structured meal planning, regular eating schedules, and mindful eating techniques may be particularly beneficial. NICE recommends multicomponent interventions that include behavioural change strategies as first-line treatment for obesity (CG189).
Dietary approaches: Working with a dietitian who understands ADHD can help develop practical, sustainable eating plans. NHS weight management services may provide access to dietetic support. Strategies might include:
-
Preparing meals in advance to reduce impulsive food choices
-
Keeping healthy snacks readily available
-
Using reminders and timers for regular meals
-
Addressing any nutritional deficiencies that may affect ADHD symptoms
Physical activity: Regular exercise benefits both weight management and ADHD symptoms. Finding enjoyable activities and building them into routine can improve adherence. Exercise has been shown to improve executive function, attention, and mood in people with ADHD.
Medication considerations: When lifestyle interventions alone are insufficient, pharmacological options may be considered. The choice between different weight management medications should account for the presence of ADHD and current ADHD treatment. Alternatives to Saxenda include orlistat (which works by reducing fat absorption) or, in specific circumstances, other GLP-1 receptor agonists such as semaglutide (where available under NICE guidance). For those with severe obesity, bariatric surgery may be considered according to NICE criteria.
Coordinated care: Optimal outcomes are achieved when ADHD specialists, GPs, dietitians, and mental health professionals work together. Referral to NHS Tier 3 or Tier 4 weight management services may be appropriate for specialist multidisciplinary support. This integrated approach ensures that treatment for one condition does not inadvertently worsen the other and that all aspects of the patient's health are considered.
Patients should be empowered to discuss their weight concerns openly with their ADHD healthcare team and explore which interventions are most appropriate for their individual circumstances.
Scientific References
Frequently Asked Questions
Is it safe to take Saxenda with stimulant ADHD medications?
There is no absolute contraindication to using Saxenda with stimulant ADHD medications, but concurrent use requires individualised medical assessment. Both medication classes can suppress appetite and affect cardiovascular function, so close monitoring of nutritional intake, heart rate, and blood pressure is essential throughout treatment.
Will Saxenda affect how my ADHD medication works?
Saxenda slows gastric emptying, which could theoretically alter the absorption rate of oral ADHD medications, particularly immediate-release formulations. However, clinically significant interactions affecting medication absorption have not been established in studies, and modified-release preparations are less likely to be affected.
What monitoring is needed when taking Saxenda and ADHD medication together?
Regular monitoring should include cardiovascular parameters (blood pressure and heart rate), nutritional adequacy and eating patterns, weight measurements, ADHD symptom control, and assessment for adverse effects from either medication. Patients with diabetes or cardiovascular conditions require particularly careful supervision.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










