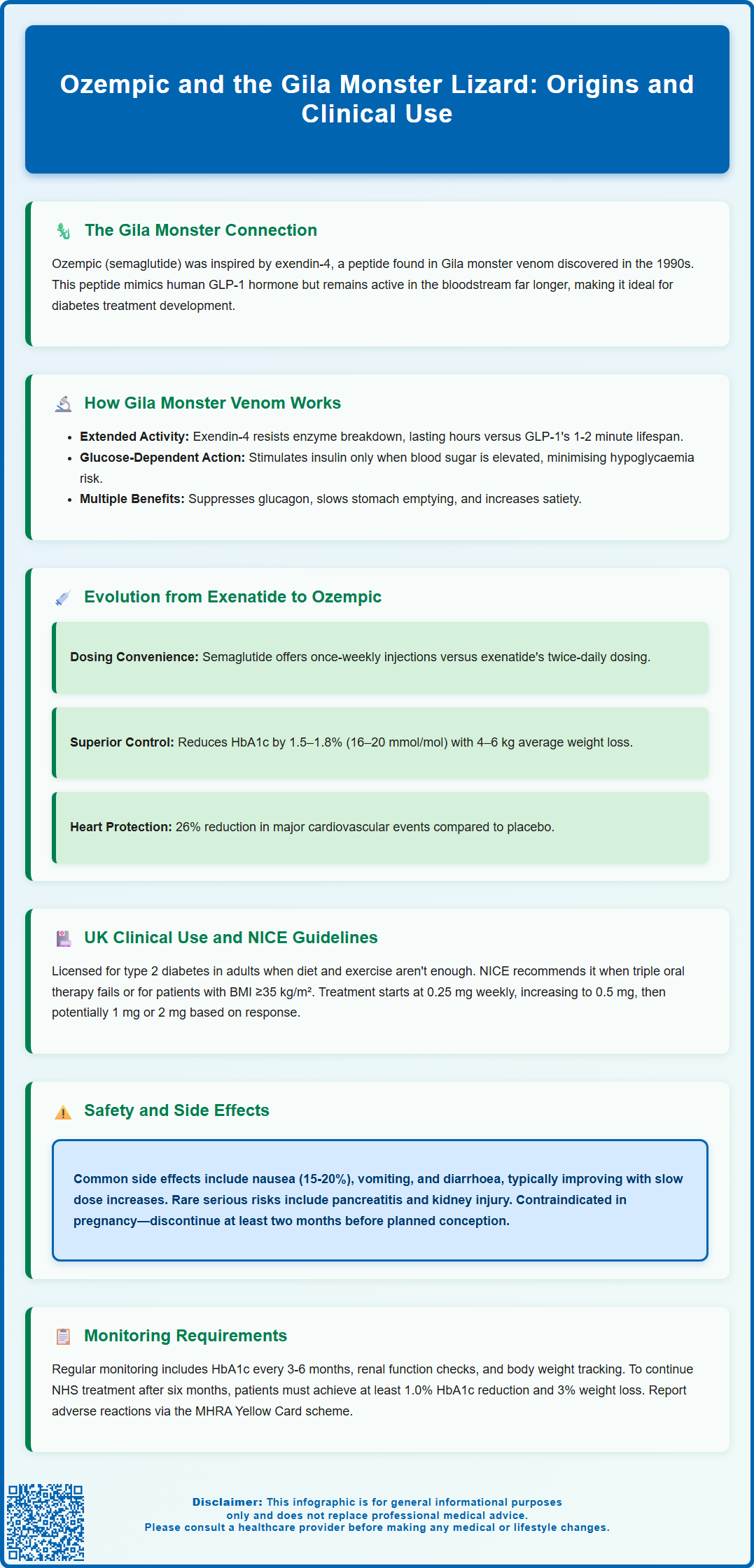
Ozempic (semaglutide), a glucagon-like peptide-1 (GLP-1) receptor agonist used to manage type 2 diabetes, has a fascinating origin linked to the Gila monster lizard. In the 1990s, researchers discovered that venom from this venomous reptile contained exendin-4, a peptide with structural similarities to human GLP-1 but with prolonged activity in the bloodstream. This discovery inspired the development of GLP-1-based diabetes medications, including exenatide and, subsequently, semaglutide. Whilst Ozempic itself is a synthetic modification of human GLP-1 rather than a direct derivative of Gila monster venom, the lizard's biology provided the crucial blueprint for this class of medicines. This article explores the scientific journey from reptile venom to modern diabetes treatment, clinical applications in the UK, and essential safety considerations.
Summary: Ozempic (semaglutide) was inspired by research into Gila monster lizard venom, which contained a long-acting peptide similar to human GLP-1, leading to the development of GLP-1 receptor agonist diabetes medications.
- Gila monster venom contains exendin-4, a peptide with 53% structural similarity to human GLP-1 but resistant to rapid enzymatic breakdown.
- Semaglutide is a synthetic GLP-1 analogue with 94% homology to human GLP-1, modified for once-weekly dosing and enhanced albumin binding.
- Ozempic is licensed in the UK for inadequately controlled type 2 diabetes as monotherapy or combination therapy, following NICE guidance criteria.
- Common adverse effects include gastrointestinal symptoms; rare serious risks include pancreatitis, diabetic retinopathy complications, and gallbladder disease.
- Treatment continuation requires HbA1c reduction of at least 11 mmol/mol and weight loss of at least 3% at six months, with regular monitoring of renal function and glycaemic control.
Table of Contents
- The Connection Between Ozempic and the Gila Monster Lizard
- How Gila Monster Venom Led to Semaglutide Development
- From Exenatide to Ozempic: The Evolution of GLP-1 Medicines
- Clinical Applications and Regulatory Approval in the UK
- Safety Considerations and Monitoring Requirements
- Scientific References
- Frequently Asked Questions
The Connection Between Ozempic and the Gila Monster Lizard
The development of Ozempic (semaglutide) represents a remarkable example of biomimicry in pharmaceutical science, with its origins tracing back to the Gila monster (Heloderma suspectum), a venomous lizard native to the southwestern United States and northwestern Mexico. This connection forms part of the scientific journey that led to certain diabetes medications known as glucagon-like peptide-1 (GLP-1) receptor agonists.
In the 1990s, researchers discovered that Gila monster venom contained a peptide called exendin-4, which shared structural similarities with human GLP-1, a naturally occurring hormone that regulates blood glucose levels. The key observation was that this peptide remained active in the bloodstream for considerably longer than human GLP-1, which is rapidly degraded by enzymes within minutes. This extended duration of action made it an attractive candidate for therapeutic development.
While exendin-4 directly inspired the development of exenatide (Byetta), later GLP-1 receptor agonists including semaglutide are based on modified human GLP-1 structures. Ozempic itself represents a synthetic evolution of GLP-1, refined through pharmaceutical research to optimise efficacy, safety, and patient convenience.
This biological inspiration has transformed diabetes management, offering patients additional treatment options within the NICE treatment pathway and demonstrating how nature continues to provide valuable blueprints for modern medicine.
How Gila Monster Venom Led to Semaglutide Development
The journey from Gila monster venom to semaglutide involved meticulous biochemical analysis and pharmaceutical engineering. Exendin-4, the peptide isolated from Gila monster saliva, demonstrated approximately 53% amino acid sequence homology with human GLP-1 but crucially resisted degradation by the enzyme dipeptidyl peptidase-4 (DPP-4), which normally breaks down GLP-1 within 1–2 minutes of secretion.
Researchers at the Veterans Affairs Medical Centre in the Bronx, New York, first characterised exendin-4 in 1992. They observed that this peptide bound to GLP-1 receptors in pancreatic beta cells, stimulating insulin secretion in a glucose-dependent manner—meaning insulin release occurred only when blood glucose levels were elevated. This mechanism results in a low risk of hypoglycaemia when used alone, though this risk increases when combined with insulin or sulfonylureas. Additionally, exendin-4 suppressed glucagon secretion, slowed gastric emptying, and promoted satiety, all beneficial effects for managing type 2 diabetes.
The pharmaceutical industry recognised the therapeutic potential and began developing synthetic analogues. The first generation resulted in exenatide (marketed as Byetta), a synthetic version of exendin-4 approved for clinical use. However, scientists continued refining the molecular structure to create compounds with even longer half-lives and improved pharmacokinetic profiles.
Semaglutide represents a second-generation GLP-1 receptor agonist with 94% structural homology to native human GLP-1. Through strategic amino acid substitutions and the addition of a fatty acid side chain, researchers created a molecule that binds to albumin in the bloodstream, protecting it from enzymatic degradation and enabling once-weekly dosing. This development pathway exemplifies rational drug design informed by evolutionary biology.
From Exenatide to Ozempic: The Evolution of GLP-1 Medicines
The evolution from exenatide to semaglutide reflects progressive improvements in pharmacology, patient convenience, and clinical outcomes. Exenatide (Byetta), approved by the European Medicines Agency (EMA) in 2006, required twice-daily subcutaneous injections and had a half-life of approximately 2.4 hours. Whilst effective at improving glycaemic control and promoting modest weight loss, the frequent dosing schedule presented adherence challenges for many patients.
Subsequent developments included liraglutide (Victoza), approved in 2009, which offered once-daily dosing with a half-life of approximately 13 hours. This represented a significant advancement in convenience, though patients still required daily injections. The pharmaceutical industry continued pursuing longer-acting formulations, recognising that reduced dosing frequency could improve treatment adherence and patient satisfaction.
Semaglutide, developed by Novo Nordisk and approved by the EMA in 2018, marked a substantial leap forward with its once-weekly dosing schedule. The extended half-life of approximately 165 hours (nearly seven days) results from structural modifications that enhance albumin binding and reduce renal clearance. Clinical trials demonstrated that semaglutide achieved superior HbA1c reductions compared to earlier GLP-1 receptor agonists, with the SUSTAIN clinical trial programme showing mean HbA1c reductions of 1.5–1.8% (approximately 16–20 mmol/mol) from baseline.
Beyond glycaemic control, semaglutide demonstrated significant cardiovascular benefits in the SUSTAIN-6 trial, with a 26% reduction in major adverse cardiovascular events compared to placebo. Weight loss effects were also more pronounced, with patients losing an average of 4–6 kg over 56 weeks. These enhanced outcomes, combined with convenient weekly dosing, have positioned Ozempic as an option within NICE guidelines for type 2 diabetes management when specific criteria are met.
Clinical Applications and Regulatory Approval in the UK
In the United Kingdom, Ozempic (semaglutide) is licensed by the Medicines and Healthcare products Regulatory Agency (MHRA) specifically for the treatment of inadequately controlled type 2 diabetes mellitus in adults. The medication is indicated as an adjunct to diet and exercise, either as monotherapy when metformin is contraindicated or not tolerated, or in combination with other glucose-lowering medications including metformin, sulfonylureas, sodium-glucose co-transporter-2 (SGLT-2) inhibitors, and insulin. Ozempic is not indicated for type 1 diabetes or for the treatment of diabetic ketoacidosis.
NICE guidance (NG28) recommends GLP-1 receptor agonists like semaglutide for adults with type 2 diabetes when:
-
Triple therapy with metformin and two other oral drugs is ineffective, not tolerated, or contraindicated
-
The person has a BMI of 35 kg/m² or higher (adjusted for ethnicity) and specific psychological or medical problems associated with obesity
-
BMI is lower than 35 kg/m² but insulin therapy would have significant occupational implications or weight loss would benefit other obesity-related comorbidities
Ozempic is available in pre-filled, multi-dose pens delivering 0.25 mg, 0.5 mg, 1 mg, or 2 mg doses. The standard initiation protocol involves starting at 0.25 mg once weekly for four weeks (a non-therapeutic dose intended to improve gastrointestinal tolerability), then increasing to 0.5 mg weekly. If additional glycaemic control is required after at least four weeks, the dose may be increased to 1 mg weekly, and subsequently to 2 mg weekly if needed.
Prescribing in the NHS typically occurs through specialist diabetes services or by GPs with appropriate expertise. Treatment continuation requires demonstration of beneficial response , defined by NICE as a reduction of at least 11 mmol/mol (1.0%) in HbA1c and weight loss of at least 3% of initial body weight at six months. Patients not meeting these thresholds should have treatment reviewed and potentially discontinued. The medication is administered via subcutaneous injection into the abdomen, thigh, or upper arm, with injection sites rotated to prevent lipodystrophy.
Safety Considerations and Monitoring Requirements
Whilst Ozempic demonstrates a favourable benefit-risk profile for appropriate patients, healthcare professionals must remain vigilant regarding potential adverse effects and precautions. The most common side effects are gastrointestinal, including nausea (occurring in 15–20% of patients), vomiting, diarrhoea, abdominal pain, and constipation. These effects are typically mild to moderate, most pronounced during dose escalation, and tend to diminish over time. Slow dose titration can help mitigate these symptoms.
Serious but rare adverse effects require particular attention:
-
Pancreatitis: Patients should be counselled to seek immediate medical attention if they experience severe, persistent abdominal pain radiating to the back, as acute pancreatitis has been reported with GLP-1 receptor agonists. Treatment should be discontinued if pancreatitis is confirmed.
-
Diabetic retinopathy complications: Patients with pre-existing diabetic retinopathy should be monitored closely, particularly if they are also on insulin, as rapid improvement in glucose control may be associated with temporary worsening of retinopathy.
-
Renal impairment: Gastrointestinal side effects causing dehydration may precipitate acute kidney injury, particularly in patients with existing renal impairment. Adequate hydration should be emphasised.
-
Hypoglycaemia: Whilst semaglutide alone carries minimal hypoglycaemia risk due to its glucose-dependent mechanism, concurrent use with sulfonylureas or insulin increases this risk. Dose reduction of these agents may be necessary.
-
Gallbladder disease: Cholelithiasis and cholecystitis have been reported. Patients should seek medical attention for symptoms such as right upper abdominal pain, fever, or jaundice.
Ozempic is contraindicated in patients with:
- Hypersensitivity to semaglutide or any of the excipients
Ozempic is not recommended during:
- Pregnancy and breastfeeding (adequate contraception required in women of childbearing potential; discontinue if pregnancy occurs)
Caution is advised in patients with:
-
Severe gastrointestinal disease, including gastroparesis
-
Pre-existing diabetic retinopathy, particularly if on insulin
Monitoring requirements include baseline and regular assessment of HbA1c (every 3–6 months), renal function, body weight, and appropriate retinal examination in at-risk patients. Patients should be advised to contact their GP if they experience persistent vomiting, severe abdominal pain, or signs of dehydration. The medication should be discontinued at least two months before planned pregnancy due to its long half-life. Healthcare professionals should provide comprehensive patient education regarding injection technique, storage requirements (refrigeration before first use), and recognition of adverse effects requiring medical attention.
Suspected adverse reactions should be reported via the MHRA Yellow Card scheme (website or app).
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics (SmPC).
- Ozempic - European Public Assessment Report.
- Type 2 diabetes in adults: management. NICE guideline NG28.
- Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes (SUSTAIN-6).
- Exendin-4 from Heloderma suspectum venom: From discovery to its latest application.
Frequently Asked Questions
Is Ozempic made from Gila monster venom?
No, Ozempic (semaglutide) is not made from Gila monster venom. It is a synthetic modification of human GLP-1, though its development was inspired by the discovery of exendin-4, a long-acting peptide found in Gila monster saliva that led to earlier GLP-1 medications like exenatide.
How does Ozempic differ from the original Gila monster-derived medication?
Ozempic (semaglutide) is structurally based on human GLP-1 with modifications for extended half-life, allowing once-weekly dosing. The original Gila monster-derived medication, exenatide (Byetta), was a synthetic version of exendin-4 requiring twice-daily injections with a shorter duration of action.
Who can be prescribed Ozempic in the UK?
Ozempic is prescribed for adults with inadequately controlled type 2 diabetes following NICE guidance, typically when triple oral therapy is ineffective or when specific BMI and comorbidity criteria are met. It requires demonstration of beneficial response (HbA1c reduction ≥11 mmol/mol and ≥3% weight loss) at six months for continuation.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










