Some patients taking GLP-1 receptor agonists for type 2 diabetes or weight management report changes in sweating patterns, prompting questions about whether these medications directly cause increased perspiration. Whilst sweating is not listed as a common side effect in official prescribing information for GLP-1 medications such as semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), or liraglutide (Victoza, Saxenda), several indirect factors may explain this phenomenon. Understanding the relationship between GLP-1 treatment and sweating helps patients recognise when symptoms require medical attention and how to manage them effectively. This article examines the mechanisms, potential causes, and practical management strategies for sweating during GLP-1 therapy.
Summary: GLP-1 receptor agonists do not directly cause sweating, but some patients report changes in perspiration patterns due to indirect factors such as gastrointestinal side effects, hypoglycaemia when combined with other diabetes medications, or autonomic responses to nausea.
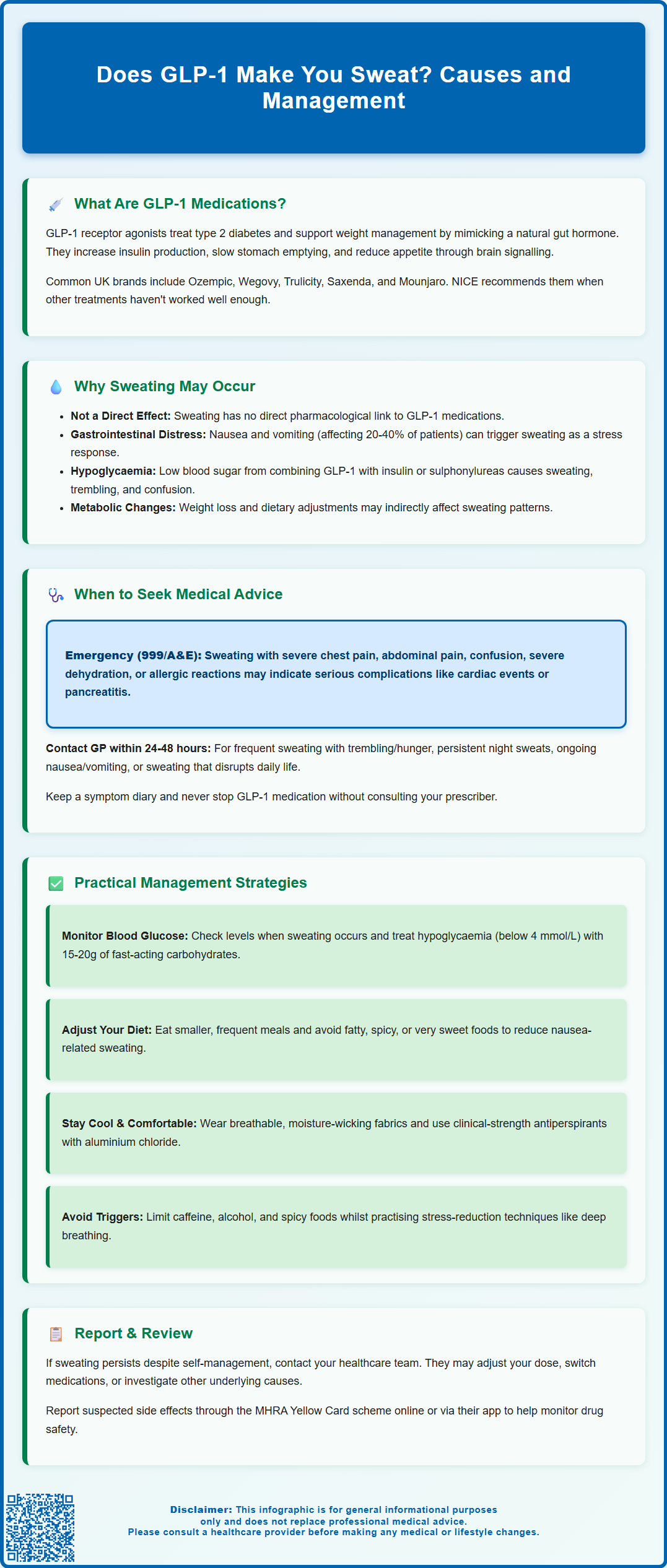
- GLP-1 receptor agonists mimic natural GLP-1 hormone to enhance insulin secretion, suppress glucagon, slow gastric emptying, and reduce appetite through central nervous system effects.
- Sweating is not listed as a common adverse effect in official prescribing information for GLP-1 medications including semaglutide, dulaglutide, and liraglutide.
- Gastrointestinal side effects (nausea, vomiting, diarrhoea) affecting 20–40% of patients may trigger autonomic sweating responses as a physiological stress reaction.
- Hypoglycaemia risk increases when GLP-1 medications are combined with insulin or sulfonylureas, with sweating being a classic warning sign requiring blood glucose monitoring.
- Seek urgent medical attention for sweating accompanied by severe chest pain, persistent abdominal pain (potential pancreatitis), confusion, or signs of severe allergic reaction.
- Management strategies include monitoring blood glucose levels, addressing gastrointestinal symptoms through dietary modifications, and consulting healthcare teams for potential dose adjustments or medication review.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily prescribed for type 2 diabetes management and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. Common examples available in the UK include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and tirzepatide (Mounjaro), which is a dual GLP-1 and GIP receptor agonist.
These medications work by mimicking the action of naturally occurring GLP-1, a hormone released by the intestine in response to food intake. The primary mechanisms of action include:
-
Enhancing insulin secretion from pancreatic beta cells in a glucose-dependent manner, which helps lower blood glucose levels without causing excessive hypoglycaemia
-
Suppressing glucagon release from pancreatic alpha cells, reducing hepatic glucose production
-
Slowing gastric emptying, which prolongs the feeling of fullness after meals
-
Acting on appetite centres in the brain, particularly the hypothalamus, to reduce hunger and food intake
Most GLP-1 receptor agonists are administered via subcutaneous injection, with dosing frequencies ranging from once daily to once weekly depending on the specific formulation. Oral semaglutide (Rybelsus) is also available as a tablet taken once daily. NICE guidelines recommend GLP-1 receptor agonists as part of the treatment algorithm for type 2 diabetes when metformin and other oral agents have not achieved adequate glycaemic control. For weight management, specific NICE criteria must be met to access these treatments through specialist services.
Some GLP-1 medications have demonstrated cardiovascular benefits in clinical trials, though this varies by specific agent and is not a universal class effect. Understanding how these medications work throughout the body helps contextualise potential side effects, including changes in sweating patterns that some patients report.
Why Might You Experience Sweating on GLP-1 Treatment?
Sweating is not listed as a common adverse effect in the official prescribing information for most GLP-1 receptor agonists, and there is no established direct pharmacological mechanism linking these medications to increased perspiration. However, some patients do report changes in sweating patterns during treatment, and several indirect factors may explain this phenomenon.
Gastrointestinal side effects represent the most common adverse reactions to GLP-1 medications, with frequencies varying by agent but often affecting 20-40% of patients according to product information. These include:
-
Nausea and vomiting
-
Diarrhoea
-
Abdominal discomfort
-
Constipation
When patients experience significant nausea or gastrointestinal distress, the body's autonomic nervous system may respond with sweating, particularly cold sweats or diaphoresis. This represents a physiological stress response rather than a direct drug effect.
Hypoglycaemia (low blood glucose) can occur when GLP-1 medications are used in combination with insulin or sulfonylureas, though the risk is lower with GLP-1 agents alone due to their glucose-dependent mechanism. Sweating is a classic warning sign of hypoglycaemia, often accompanied by trembling, palpitations, confusion, and hunger. Patients taking combination therapy should be particularly vigilant for these symptoms.
Weight loss during GLP-1 treatment may be associated with changes in how some people experience sweating, though this varies between individuals and scientific evidence for direct effects on thermoregulation is limited.
Dietary changes often accompany GLP-1 treatment, as patients naturally consume smaller portions and may alter their food choices. Changes in meal timing, composition, or caloric intake can influence blood glucose fluctuations and autonomic responses, potentially affecting perspiration.
It is important to note that sweating is typically a secondary effect related to other factors rather than a direct effect of GLP-1 medications themselves. If sweating occurs, investigating underlying causes and contributing factors is essential for appropriate management.
When to Seek Medical Advice About Sweating on GLP-1
Whilst mild changes in sweating patterns may not require immediate medical attention, certain symptoms warrant prompt evaluation by your GP or healthcare team. Understanding when sweating represents a potentially serious issue is crucial for patient safety.
Seek urgent medical attention (contact 999 or attend A&E) if you experience:
-
Profuse sweating accompanied by severe chest pain, chest tightness, or pain radiating to the jaw or arm, which may indicate a cardiac event
-
Sweating with severe abdominal pain, particularly if persistent or worsening, as this could signal pancreatitis—a rare but serious complication of GLP-1 medications
-
Confusion, loss of consciousness, or inability to swallow alongside sweating, suggesting severe hypoglycaemia
-
Signs of severe dehydration including reduced urine output, extreme thirst, dizziness, or rapid heartbeat
-
Severe allergic reaction with swelling of the face/tongue, difficulty breathing, or widespread rash
-
Upper right abdominal pain with fever or yellowing of the skin/eyes, which could indicate gallbladder problems (a known risk with GLP-1 medications)
Contact your GP or diabetes specialist nurse within 24–48 hours if you notice:
-
Frequent episodes of sweating accompanied by trembling, hunger, or palpitations, which may indicate recurrent hypoglycaemia requiring medication adjustment
-
Night sweats that are new, persistent, or drenching, as these warrant investigation for other underlying conditions
-
Sweating associated with persistent nausea, vomiting, or inability to tolerate food or fluids, which may require dose adjustment or additional support
-
Unexplained fever with sweating, which could indicate infection
-
Any sweating pattern that significantly impacts your quality of life or daily activities
If you're unsure about the urgency of your symptoms, NHS 111 can provide guidance. Routine monitoring should include discussing any new or changed symptoms at your regular diabetes or weight management reviews. Your healthcare team can assess whether symptoms relate to your GLP-1 medication, require investigation for alternative causes, or necessitate treatment modification. Keeping a symptom diary noting when sweating occurs, associated activities, food intake, and any other symptoms can provide valuable information for clinical assessment. Never discontinue GLP-1 medication without consulting your prescriber, as abrupt cessation may affect glycaemic control or weight management progress.
If you suspect your medication is causing side effects, you can report these through the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Managing Sweating While Taking GLP-1 Medications
If you experience sweating whilst taking GLP-1 medications, several practical strategies can help manage symptoms whilst your healthcare team investigates any underlying causes.
Address potential hypoglycaemia:
-
Monitor blood glucose levels if you have a glucose meter, particularly when sweating occurs
-
If hypoglycaemia occurs (typically below 4 mmol/L), take 15-20g of fast-acting carbohydrate such as glucose tablets, 150-200ml of non-diet sugary drink, or 4-5 jelly babies
-
Recheck glucose after 10-15 minutes and repeat treatment if still low
-
Follow with a longer-acting carbohydrate snack (e.g., sandwich, piece of fruit, or biscuits) once glucose begins to rise
-
Discuss with your GP whether dose adjustments to other diabetes medications may be appropriate
-
Ensure regular meal timing and avoid prolonged fasting periods
Manage gastrointestinal side effects:
-
Eat smaller, more frequent meals rather than large portions, which can help reduce nausea-related sweating
-
Avoid trigger foods that worsen nausea, such as fatty, spicy, or very sweet items
-
Stay well-hydrated with small, frequent sips of water throughout the day
-
If nausea is significant, speak to your GP about prescription antiemetic options—these should only be used after medical assessment and with awareness of potential restrictions (some antiemetics have limitations on duration of use or specific contraindications)
-
Allow adequate time after dose escalation for side effects to settle, typically 4–6 weeks
General comfort measures:
-
Wear breathable, moisture-wicking fabrics made from natural fibres like cotton or specialist athletic materials
-
Consider clinical-strength antiperspirants containing aluminium chloride if appropriate, but avoid applying to irritated or broken skin
-
Maintain a cool environment, particularly at night if experiencing night sweats
-
Layer clothing to allow easy adjustment to temperature changes
-
Ensure adequate hydration, aiming for 6–8 glasses of fluid daily unless otherwise advised
Lifestyle modifications:
-
Avoid known sweating triggers such as caffeine, alcohol, and spicy foods if these worsen symptoms
-
Practice stress-reduction techniques including deep breathing exercises or mindfulness, as anxiety can exacerbate sweating
-
Maintain regular physical activity, but exercise in cooler parts of the day if heat sensitivity is problematic
Medical review:
If sweating persists despite these measures, your healthcare team may consider dose adjustment, switching to an alternative GLP-1 formulation, or investigating other potential causes unrelated to your medication. Any changes to your treatment should be clinician-led and based on a thorough assessment of your individual circumstances. Regular communication with your diabetes team ensures optimal management of both your underlying condition and any treatment-related symptoms.
Scientific References
Frequently Asked Questions
Is sweating a common side effect of GLP-1 medications?
Sweating is not listed as a common adverse effect in official prescribing information for GLP-1 receptor agonists. When patients experience sweating, it typically results from indirect factors such as gastrointestinal side effects, hypoglycaemia when combined with other diabetes medications, or autonomic responses to nausea rather than a direct pharmacological effect of the medication.
When should I seek medical help for sweating whilst taking GLP-1 medications?
Seek urgent medical attention (999 or A&E) if sweating occurs with severe chest pain, persistent severe abdominal pain (potential pancreatitis), confusion or loss of consciousness, or signs of severe allergic reaction. Contact your GP within 24–48 hours for frequent sweating episodes with trembling or palpitations (suggesting hypoglycaemia), persistent night sweats, or sweating that significantly impacts daily life.
How can I manage sweating whilst taking GLP-1 treatment?
Monitor blood glucose levels if sweating occurs, particularly if taking GLP-1 medications alongside insulin or sulfonylureas. Manage gastrointestinal side effects through smaller, frequent meals and adequate hydration. Wear breathable fabrics, maintain a cool environment, and avoid known triggers such as caffeine or spicy foods. Discuss persistent symptoms with your healthcare team, who may consider dose adjustments or alternative formulations.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












