Protein shakes for Ozempic users have become an important nutritional consideration as semaglutide treatment often reduces appetite and food intake. Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, whilst Wegovy (higher-dose semaglutide) is approved for weight management. Both medications slow gastric emptying and suppress appetite, which can make consuming adequate protein through whole foods challenging. Maintaining sufficient protein intake during treatment is essential for preserving lean muscle mass, supporting metabolic health, and preventing sarcopenia. This article examines evidence-based strategies for incorporating protein shakes safely and effectively into the dietary regimen of patients taking Ozempic.
Summary: Protein shakes can help Ozempic users meet daily protein requirements when appetite suppression makes consuming adequate protein through whole foods difficult.
- Ozempic (semaglutide) is a GLP-1 receptor agonist that reduces appetite and slows gastric emptying, making adequate protein intake challenging for many patients.
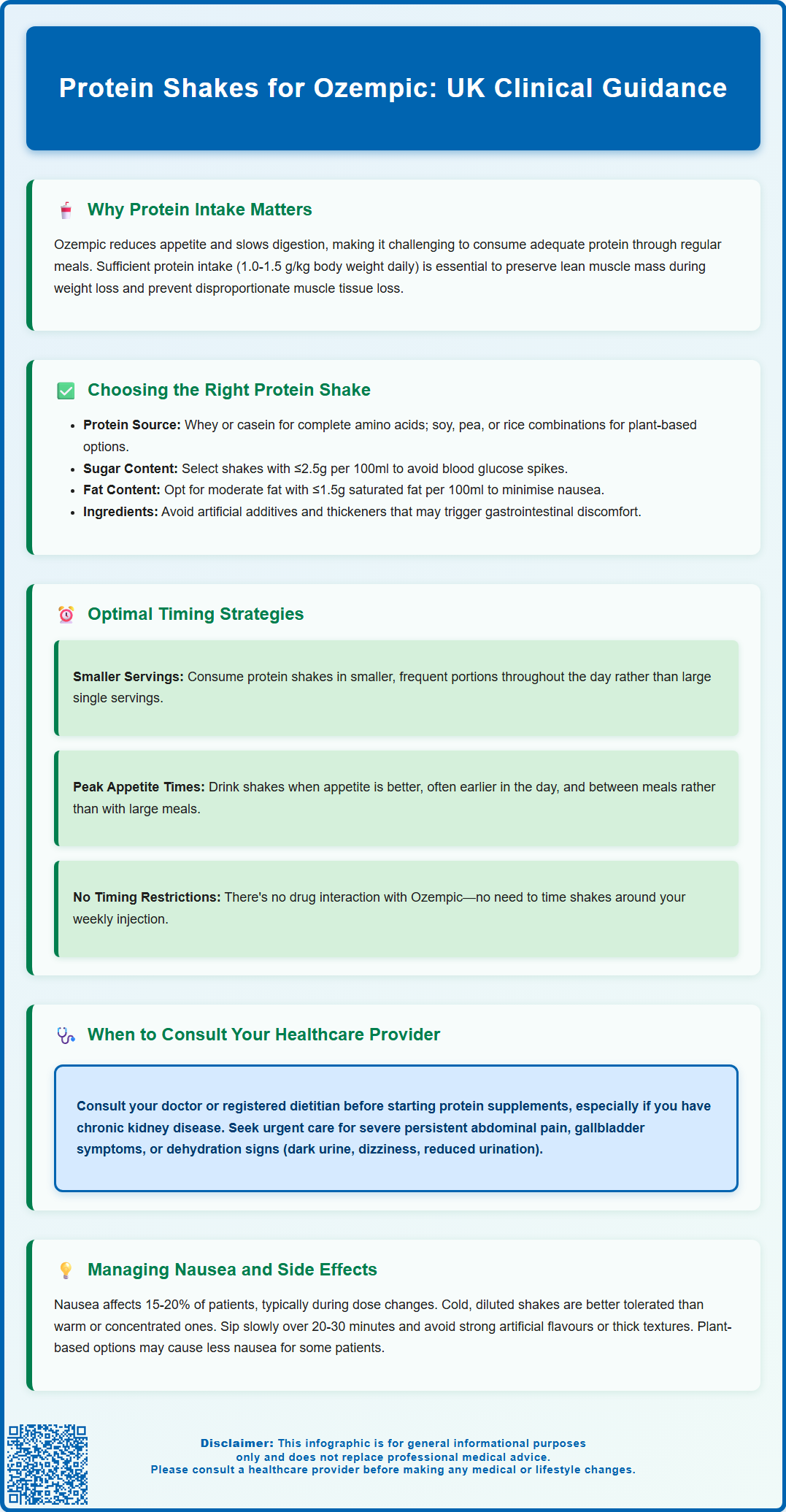
- UK guidance recommends 0.75g protein per kg body weight daily for adults, with higher intakes of 1.0-1.5g/kg/day beneficial during weight loss to preserve muscle mass.
- Choose protein shakes with minimal added sugars (≤2.5g per 100ml), moderate fat content, and complete amino acid profiles from whey, casein, or plant-based sources.
- Consume protein shakes slowly in small, frequent portions throughout the day rather than large single servings to minimise nausea and gastrointestinal discomfort.
- Patients with chronic kidney disease should consult healthcare providers before increasing protein intake, and persistent nausea may require dose adjustment or medical review.
Table of Contents
Why Protein Intake Matters When Taking Ozempic
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. At higher doses, under the brand name Wegovy, it is licensed for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, as per NICE TA875. The medication works by mimicking the action of endogenous GLP-1, which slows gastric emptying, reduces appetite, and enhances insulin secretion in response to meals. These mechanisms contribute to improved glycaemic control and, in many patients, reduced food intake and weight loss.
Maintaining adequate protein intake during Ozempic treatment is clinically important for several reasons. Protein is essential for preserving lean muscle mass during periods of caloric restriction and weight loss. Research indicates that individuals losing weight without sufficient protein intake may lose a higher proportion of muscle tissue relative to fat mass, which can adversely affect metabolic rate, physical function, and long-term weight maintenance. The UK Reference Nutrient Intake (RNI) for protein is 0.75 grams per kilogram of body weight daily for adults. However, during periods of weight loss or for older adults, higher intakes of 1.0-1.5 g/kg/day may be beneficial, as recommended by the European Society for Clinical Nutrition and Metabolism (ESPEN) and the British Dietetic Association (BDA).
Patients taking Ozempic often report early satiety and reduced appetite, making it challenging to consume adequate protein through whole foods alone. This is particularly relevant for individuals experiencing gastrointestinal side effects such as nausea or reduced gastric capacity. Protein also plays a crucial role in immune function, wound healing, and the synthesis of enzymes and hormones. For patients with type 2 diabetes, including protein as part of a balanced meal may help manage overall dietary patterns and glycaemic response. Healthcare professionals should consider discussing protein requirements with patients initiating Ozempic therapy, particularly those at risk of malnutrition or sarcopenia, and recommend resistance exercise alongside adequate protein intake to help preserve muscle mass.
Choosing the Right Protein Shake While on Ozempic
When selecting a protein shake to supplement dietary intake during Ozempic treatment, several factors warrant consideration to ensure the product aligns with therapeutic goals and minimises potential adverse effects. The primary consideration is the protein source and quality. Whey protein, derived from milk, is rapidly absorbed and contains all essential amino acids, making it a complete protein source. Casein protein, also milk-derived, is absorbed more slowly and may provide sustained amino acid release. Plant-based alternatives such as soy protein provide a complete amino acid profile, while others like pea or rice protein may have lower levels of certain amino acids and are sometimes combined to provide a more balanced profile. These alternatives are suitable for individuals with lactose intolerance or those following vegan diets.
The carbohydrate and sugar content of protein shakes requires careful evaluation, particularly for patients using Ozempic for diabetes management. According to UK traffic-light labelling guidance, products with ≤5g of sugar per 100g (for solids) or ≤2.5g per 100ml (for liquids) are classified as low in sugar. Patients should be advised to select products with minimal added sugars, as these may affect blood glucose levels. Products formulated specifically for diabetes management often use low-glycaemic sweeteners or are unsweetened, allowing patients to control sweetness according to preference.
Fat content is another important consideration. Whilst some dietary fat is necessary for satiety and absorption of fat-soluble vitamins, high-fat protein shakes may theoretically exacerbate the delayed gastric emptying caused by Ozempic, potentially worsening nausea or feelings of fullness. Products with moderate fat content and lower saturated fat (≤1.5g per 100ml according to UK traffic-light labelling) are generally preferable. Patients should also examine the ingredient list for artificial additives, thickeners, or emulsifiers that may cause gastrointestinal discomfort in sensitive individuals.
Patients with chronic kidney disease should consult their healthcare provider before increasing protein intake through supplements, as higher protein intake may not be appropriate. Consulting with a registered dietitian can provide personalised guidance based on individual nutritional needs, comorbidities, and tolerance. Resources from Diabetes UK and the NHS can help patients understand food labelling and make appropriate choices. There is no official guidance from NICE specifically addressing protein shake selection for patients on GLP-1 receptor agonists, so clinical judgement and individualised assessment remain paramount.
When to Drink Protein Shakes During Ozempic Treatment
The timing of protein shake consumption can significantly influence tolerability and nutritional benefit for patients taking Ozempic. Given that semaglutide delays gastric emptying and reduces appetite, strategic timing may help optimise protein intake whilst minimising gastrointestinal discomfort. Many patients find that consuming smaller, more frequent protein-containing meals or supplements throughout the day is better tolerated than attempting to consume large amounts of protein in single sittings.
For individuals using protein shakes as meal replacements, consuming them during periods of relatively better appetite may be advantageous. Some patients report that appetite suppression varies throughout the day, with many finding earlier in the day more favourable for protein supplementation. However, this pattern varies considerably between individuals, and patients should be encouraged to identify their own tolerance patterns. Consuming protein shakes between meals, rather than with large mixed meals, may reduce the cumulative volume of gastric contents and associated feelings of excessive fullness.
Patients engaging in physical activity or resistance training should consider their overall daily protein intake, which is generally more important than precise timing for most individuals. Consuming protein within the hours following exercise may support muscle recovery, though evidence suggests total daily protein intake is the primary factor for muscle maintenance. For those experiencing significant morning nausea—a common side effect during the initial weeks of Ozempic therapy—delaying protein shake consumption until symptoms subside may improve tolerance.
It is important to note that there is no pharmacological interaction between Ozempic and dietary protein, and no specific timing requirements relative to injection. Ozempic is administered subcutaneously once weekly and does not require specific timing relative to meals, as stated in the MHRA product information. Patients should maintain consistent hydration when increasing protein intake, as adequate fluid consumption supports renal function and helps prevent constipation, another potential side effect of GLP-1 receptor agonists. If patients experience persistent difficulty tolerating any oral intake, inability to keep fluids down for more than 24-48 hours, or signs of dehydration, they should contact their GP or diabetes specialist nurse promptly, as this may indicate excessive dose escalation or an underlying complication requiring medical attention.
Managing Side Effects: Protein Shakes and Nausea
Nausea is one of the most frequently reported adverse effects of Ozempic, occurring in approximately 15 to 20 per cent of patients according to the MHRA Summary of Product Characteristics, with higher rates observed at the higher doses used for weight management (Wegovy). This side effect typically emerges during dose initiation or escalation and often diminishes over several weeks as physiological adaptation occurs. However, for some patients, nausea persists and can significantly impact nutritional intake, including the ability to consume protein shakes. Understanding strategies to minimise nausea whilst maintaining adequate protein intake is therefore clinically relevant.
The composition and temperature of protein shakes can influence their tolerability in patients experiencing nausea. Cold or chilled protein shakes are often better tolerated than room-temperature or warm preparations, as lower temperatures may reduce the perception of strong flavours or odours that can trigger nausea. Diluting protein powder with a larger volume of liquid creates a less concentrated mixture that may be easier to consume in small, frequent sips rather than drinking quickly. Some patients find that plant-based protein shakes cause less nausea than dairy-based alternatives, possibly due to lactose content or the different digestion kinetics of plant proteins.
Patients should be advised to consume protein shakes slowly, taking small sips over 20 to 30 minutes rather than drinking rapidly. This approach reduces the rate of gastric filling and may prevent triggering the nausea reflex. Avoiding protein shakes with strong artificial flavours, excessive sweetness, or thick, creamy textures may also improve tolerance. Adding natural flavourings such as a small amount of fresh fruit, vanilla extract, or cocoa powder can make shakes more palatable without significantly increasing sugar content.
Patients should seek urgent medical attention if they experience severe persistent abdominal pain (which may indicate pancreatitis), symptoms of gallbladder disease, or signs of dehydration such as dark urine, dizziness, or reduced urine output. These are potential serious adverse effects associated with GLP-1 receptor agonists that require prompt assessment. Persistent nausea may indicate the need for dose adjustment, such as temporarily reducing the Ozempic dose or delaying dose escalation as per the product information. Monitoring renal function is important if prolonged vomiting or dehydration occurs, particularly in patients with pre-existing chronic kidney disease. NICE guidance (NG28) on diabetes management emphasises the importance of individualising treatment and monitoring for adverse effects. Healthcare professionals should regularly review nutritional status and consider referral to dietetic services for patients struggling to maintain adequate protein and overall nutritional intake during Ozempic therapy.
Scientific References
- Semaglutide for managing overweight and obesity.
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group.
- The Eatwell Guide.
- Food guidelines and food labels - How to read food labels.
Frequently Asked Questions
Can I drink protein shakes whilst taking Ozempic?
Yes, protein shakes are safe to consume with Ozempic and can help meet daily protein requirements when appetite suppression makes eating whole foods difficult. Choose products with minimal added sugars and consume slowly in small portions to improve tolerance.
How much protein should I consume daily on Ozempic?
The UK Reference Nutrient Intake is 0.75g per kg body weight daily, but during weight loss, higher intakes of 1.0-1.5g/kg/day may be beneficial to preserve muscle mass. Consult a registered dietitian for personalised recommendations based on your individual needs.
What type of protein shake is best for Ozempic users?
Select protein shakes with complete amino acid profiles (whey, casein, or soy), low sugar content (≤2.5g per 100ml), and moderate fat levels. Cold, diluted preparations consumed slowly are often better tolerated than thick, concentrated shakes.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript