Do you feel that weight loss is a constant uphill battle, even while taking GLP-1 medications like Wegovy? Join Bolt Pharmacy as we peel back the layers on these intriguing treatments and uncover how they support weight management and metabolic health. If your stomach's still growling despite your best efforts, hold tight. We’re about to explore these hunger pangs and offer some trustworthy insights on GLP-1 treatments. Dive into our exciting voyage through the land of lasting weight control.
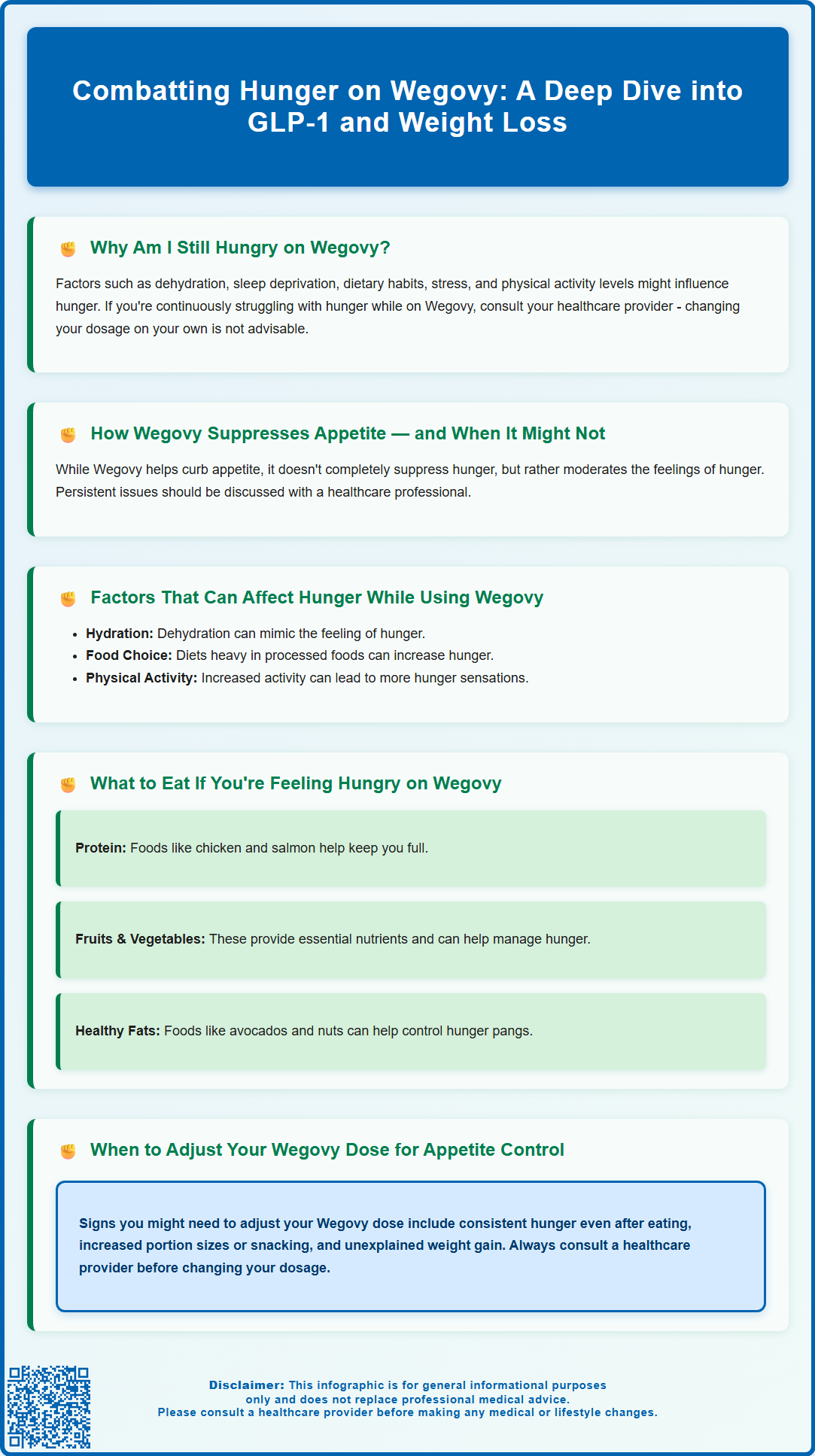
Summary: Feeling hungry on Wegovy is not uncommon; the drug reduces, not eradicates, appetite and other factors may affect hunger levels.
- Wegovy (semaglutide) imitates the hormone GLP-1 which controls appetite, but does not completely eliminate hunger.
- Your hydration levels, sleep quality, diet, stress levels and amount of physical activity can impact hunger, even when using Wegovy.
- Persistent or uncomfortable hunger on Wegovy should be discussed with a healthcare provider rather than adjusting dosage alone.
- Consuming a balanced diet of protein-rich, fibre-rich and healthy-fat foods can help manage feelings of hunger on Wegovy.
- Persistent hunger might indicate a need to review Wegovy dosage with a healthcare provider.
Table of Contents
Why Am I Still Hungry on Wegovy?
Wegovy (semaglutide 2.4mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. Whilst clinical trials demonstrate significant appetite suppression in most patients, some individuals report persistent or breakthrough hunger during treatment, which can be both frustrating and concerning.
Experiencing continued hunger on Wegovy does not necessarily indicate treatment failure. The medication's appetite-suppressing effects vary considerably between individuals due to differences in metabolism, hormonal regulation, lifestyle factors, and the stage of dose escalation. During the initial titration phase—which typically follows a 16-week schedule (0.25, 0.5, 1.0, 1.7, 2.4 mg at 4-week intervals), with slower escalation if needed due to side effects—appetite suppression may be incomplete or inconsistent.
It is important to recognise that Wegovy is designed to work alongside dietary modification and increased physical activity, not as a standalone solution. The medication reduces hunger signals and affects gastric emptying, but it cannot override all physiological and psychological drivers of eating. Factors such as stress, inadequate sleep, emotional eating patterns, and insufficient protein or fibre intake can all contribute to persistent hunger sensations.
Understanding why hunger persists requires consideration of both pharmacological and behavioural elements. Some patients may experience genuine physiological hunger, whilst others may be responding to habitual eating cues, thirst misinterpreted as hunger, or psychological factors. Distinguishing between these can help guide appropriate management strategies and realistic expectations for treatment outcomes.
How Wegovy Affects Appetite and Hunger Signals
Wegovy's active ingredient, semaglutide, mimics the action of naturally occurring GLP-1, a hormone released by the intestine in response to food intake. GLP-1 receptor agonists work through multiple complementary mechanisms to reduce appetite and promote weight loss. Understanding these pathways helps explain both the medication's effectiveness and why some patients may still experience hunger.
Central nervous system effects: Semaglutide acts on GLP-1 receptors in key appetite-regulating areas of the hypothalamus and brainstem. This central action reduces hunger signals, increases feelings of satiety, and diminishes food reward responses. The medication essentially influences the brain's perception of fullness, making smaller portions feel more satisfying.
Gastric emptying: Wegovy can slow the rate at which food leaves the stomach and enters the small intestine, particularly early in treatment. This delayed gastric emptying may prolong the sensation of fullness after meals and reduce the frequency of hunger between eating occasions. However, this effect can diminish over time (tachyphylaxis) and varies in intensity throughout the treatment course.
Hormonal effects: Semaglutide increases glucose-dependent insulin secretion and decreases inappropriate glucagon secretion. It reduces energy intake and may influence other appetite-related hormones. These interconnected hormonal changes work together to reduce overall caloric intake. Weight loss itself can lead to improved insulin sensitivity as a secondary benefit.
The appetite-suppressing effects of Wegovy typically become more pronounced as the dose increases during the titration schedule. Peak effects are generally observed at the maintenance dose of 2.4mg weekly, though individual responses vary considerably based on genetic factors, baseline metabolic health, and concurrent medications.
Common Reasons for Continued Hunger During Wegovy Treatment
Several factors can contribute to persistent hunger whilst taking Wegovy, and identifying the underlying cause is essential for effective management.
Insufficient dose or early treatment phase: Patients in the initial titration stages (0.25mg to 1.7mg weekly) commonly experience less appetite suppression than at the full maintenance dose. The gradual dose escalation is designed to minimise gastrointestinal side effects, but it means that optimal hunger control may not be achieved for several months. Some individuals may also require dose adjustments or extended time at maintenance dose before experiencing full benefits.
Inadequate dietary composition: Hunger on Wegovy can persist if meals lack sufficient protein, fibre, or healthy fats—nutrients that promote satiety independent of medication effects. Diets high in refined carbohydrates and sugars can cause rapid blood glucose fluctuations, triggering hunger even when caloric needs are met. The quality of food consumed matters as much as quantity when managing appetite.
Dehydration and thirst confusion: The body's thirst signals can be misinterpreted as hunger, particularly in individuals who are chronically under-hydrated. Wegovy can occasionally cause mild dehydration through gastrointestinal effects, and insufficient fluid intake may manifest as persistent hunger sensations.
Psychological and habitual eating patterns: Emotional eating, stress-related food seeking, and deeply ingrained eating habits can override pharmacological appetite suppression. Wegovy addresses physiological hunger but does not eliminate psychological drivers of eating behaviour. Boredom, anxiety, depression, and social eating cues can all trigger the desire to eat despite adequate caloric intake.
Sleep deprivation and circadian disruption: Poor sleep quality or insufficient sleep duration disrupts appetite-regulating hormones, particularly increasing ghrelin and decreasing leptin. This hormonal imbalance can counteract Wegovy's appetite-suppressing effects and lead to increased hunger, especially for high-calorie foods.
Medication interactions and medical conditions: Certain medications (including some antidepressants, antipsychotics, and corticosteroids) can increase appetite and potentially reduce Wegovy's effectiveness. The risk of hypoglycaemia is increased when semaglutide is used with insulin or sulfonylureas. Underlying conditions such as insulin resistance, polycystic ovary syndrome (PCOS), thyroid disorders, or poorly controlled diabetes may also influence hunger levels during treatment.
Managing Hunger While Taking Wegovy
Addressing persistent hunger on Wegovy requires a multifaceted approach combining dietary strategies, lifestyle modifications, and behavioural techniques.
Optimise meal composition and timing:
-
Include a source of protein with each meal to enhance satiety and preserve lean muscle mass during weight loss
-
Choose high-fibre foods such as vegetables, pulses, and whole grains to promote fullness and slow digestion
-
Incorporate healthy fats from sources like nuts, seeds, avocados, and olive oil, which can help you feel fuller for longer
-
Consider eating smaller, more frequent meals if large meals cause discomfort
-
Avoid ultra-processed foods and refined carbohydrates that can trigger rapid hunger return
Maintain adequate hydration: Aim for 6-8 glasses of fluid daily (approximately 1.5-2 litres), distributed throughout the day, unless advised otherwise by your healthcare provider. People with certain heart or kidney conditions may need to restrict fluids. Begin meals with a drink and keep water readily available. Herbal teas and sugar-free beverages can contribute to fluid intake. If uncertain whether you're experiencing hunger or thirst, drink water first and reassess after 15–20 minutes.
Address sleep and stress: Prioritise 7–9 hours of quality sleep nightly, as sleep deprivation significantly undermines appetite regulation. Establish consistent sleep-wake times and create a conducive sleep environment. Implement stress-management techniques such as mindfulness, meditation, regular physical activity, or cognitive behavioural strategies to reduce stress-related eating.
Mindful eating practices: Eat slowly and without distractions (television, phones, computers) to allow satiety signals to register properly. It takes approximately 20 minutes for fullness signals to reach the brain. Chew thoroughly and pause between bites. Keep a food diary to identify patterns, triggers, and distinguish between physical hunger and emotional eating.
Physical activity: Regular exercise helps regulate appetite hormones and can reduce stress-related eating. Aim for at least 150 minutes of moderate-intensity activity weekly, plus muscle-strengthening activities on two days per week, as recommended by the UK Chief Medical Officers' Physical Activity Guidelines. Both aerobic exercise and resistance training offer benefits.
Behavioural support: Consider referral to a dietitian or weight management service for personalised guidance. Psychological support through cognitive behavioural therapy (CBT) or counselling can address emotional eating patterns and develop healthier coping strategies.
When to Speak to Your GP About Hunger on Wegovy
Whilst some hunger during Wegovy treatment can be normal, particularly in early treatment phases, certain situations warrant medical review to ensure treatment optimisation and exclude underlying issues.
Contact your GP or prescribing clinician if:
-
You experience persistent, severe hunger despite reaching the maintenance dose of 2.4mg weekly for at least 8–12 weeks
-
You have severe, persistent abdominal pain (with or without vomiting), especially if radiating to the back (possible pancreatitis) – seek urgent medical care
-
You develop right upper quadrant pain, fever, or yellowing of the skin/eyes (possible gallbladder disease) – seek urgent medical care
-
Hunger is accompanied by other concerning symptoms such as excessive thirst, frequent urination, unexplained weight gain, or fatigue (which may indicate inadequate diabetes control or other metabolic issues)
-
You have gained weight or stopped losing weight despite adherence to dietary and lifestyle recommendations
-
You experience symptoms of hypoglycaemia (low blood sugar), particularly if you have type 2 diabetes or take insulin or sulfonylureas (these medications may need dose adjustment)
-
You experience severe gastrointestinal symptoms (persistent nausea, vomiting, or abdominal pain) that prevent adequate nutritional intake
-
You suspect medication interactions with other prescribed treatments
-
Psychological factors such as depression, anxiety, or disordered eating patterns are significantly impacting your relationship with food
Your healthcare provider can assess whether dose adjustment is appropriate, review your overall treatment plan, and investigate potential underlying causes. They may consider checking thyroid function, HbA1c (if diabetic), or other relevant blood tests. In some cases, referral to specialist weight management services, dietetics, or psychological support may be beneficial.
It is important to maintain realistic expectations: Wegovy typically produces 10–15% body weight reduction over 68 weeks in clinical trials, but individual responses vary. The medication is most effective when combined with comprehensive lifestyle changes. In the NHS, semaglutide for weight management is provided via specialist services and usually for a limited duration as per NICE guidance (TA875).
Never adjust your Wegovy dose independently or discontinue treatment without medical guidance. Evidence from clinical trials shows that weight regain commonly occurs after stopping treatment. Open communication with your healthcare team ensures you receive appropriate support throughout your weight management journey.
Frequently Asked Questions
Why am I still feeling hungry while using Wegovy for weight loss?
Wegovy, a GLP-1 receptor agonist, aids in managing your appetite by mimicking the functions of natural hormones. However, it's possible to still experience hunger as it doesn’t completely eliminate this feeling. The medication slows down digestion and helps you feel full faster, but you may still feel hunger, especially when your body needs nutrition. Other contributing factors, such as hydration levels, sleep, dietary habits, stress and physical activity level, can also affect your hunger levels while on Wegovy.
Should I adjust my Wegovy dosage if I'm feeling constantly hungry?
If you’re consistently battling hunger on Wegovy, it’s crucial to talk with your healthcare provider. Never independently adjust your dosage, as your doctor or medical professional should make that decision based on a comprehensive assessment of your needs and responses to the medication. Constant hunger could indicate that your dosage needs adjustment, or it could be an indication of other factors influencing your hunger levels.
Are there ways to manage feeling hungry when using Wegovy?
If you feel hungry while using Wegovy, you may benefit from small, frequent meals or snacks composed of protein, fibre, and healthy fats to provide sustained energy and satiety. Drinking plenty of water can also help, as dehydration can often be mistaken for hunger. Make sure to get enough sleep and manage stress levels, as these factors can influence hunger. Talk with your healthcare provider for personalised advice on healthy eating and hunger management while on Wegovy.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript