Ozempic (semaglutide), a GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management, commonly causes gastrointestinal side effects including nausea, diarrhoea, and constipation. Many patients wonder whether the best probiotic while on Ozempic might help alleviate these symptoms. Whilst no large-scale trials have specifically examined probiotics alongside semaglutide, certain strains show promise for managing digestive complaints. This article explores the evidence, strain selection, timing considerations, and safety aspects of probiotic supplementation during Ozempic therapy, helping patients and clinicians make informed decisions within UK clinical guidance.
Summary: No specific probiotic has been proven best for Ozempic users, but strains like Lactobacillus rhamnosus GG, Saccharomyces boulardii, and Bifidobacterium lactis may help manage gastrointestinal side effects based on broader evidence.
- Ozempic commonly causes nausea, diarrhoea, and constipation by slowing gastric emptying and altering gut motility.
- Probiotic effects are strain-specific; Saccharomyces boulardii may help diarrhoea whilst Bifidobacterium lactis strains may improve constipation.
- No large-scale trials have examined probiotics specifically with GLP-1 receptor agonists like semaglutide.
- Probiotics are generally safe but immunocompromised patients and those with central venous catheters require caution.
- Probiotics do not interact with semaglutide pharmacologically and can be taken daily throughout the weekly dosing cycle.
- Severe or persistent gastrointestinal symptoms require medical review to exclude complications such as gallbladder disease or dehydration.
Table of Contents
- Why Probiotics May Help When Taking Ozempic
- Choosing the Right Probiotic Strains for GLP-1 Medications
- When to Take Probiotics Alongside Ozempic
- Evidence for Probiotics in Managing Digestive Side Effects
- Safety Considerations and Interactions with Semaglutide
- Scientific References
- Frequently Asked Questions
Why Probiotics May Help When Taking Ozempic
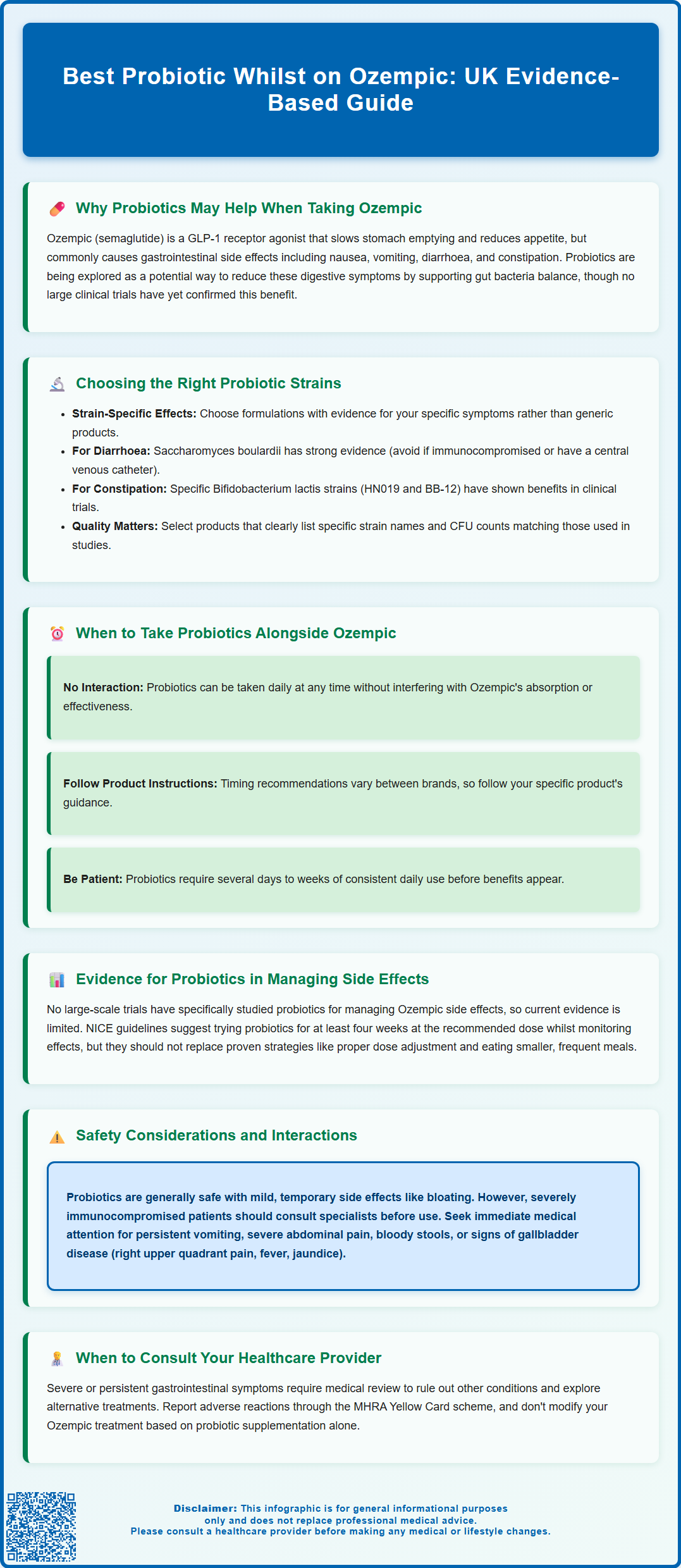
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus and, at higher doses under the brand name Wegovy, for weight management in adults with obesity or overweight with comorbidities. The medication works by mimicking the action of endogenous GLP-1, which slows gastric emptying, enhances insulin secretion in a glucose-dependent manner, and reduces appetite through central nervous system pathways. Whilst these mechanisms contribute to improved glycaemic control and weight reduction, they also frequently result in gastrointestinal adverse effects.
According to the MHRA-approved Summary of Product Characteristics (SmPC), the most commonly reported side effects of semaglutide include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. These symptoms typically emerge during dose titration and may diminish over time as tolerance develops. However, for some patients, gastrointestinal disturbances persist and can significantly impact treatment adherence and quality of life. There is limited evidence suggesting that changes to gut motility may influence the intestinal microbiota, though a direct causal relationship between semaglutide and microbiome disruption has not been firmly established.
Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. There is growing interest in whether probiotic supplementation might help mitigate the gastrointestinal side effects associated with GLP-1 receptor agonists. The theoretical rationale centres on probiotics' potential to support microbial balance, intestinal barrier function, gut transit time, and reduce inflammation within the gastrointestinal tract. Whilst there is no official link established through large-scale clinical trials specifically examining probiotics with Ozempic, the broader evidence base for probiotics in managing various digestive complaints has prompted both patients and clinicians to consider their adjunctive use during semaglutide therapy.
It is important to note that severe gastrointestinal symptoms with Ozempic may lead to dehydration and, in rare cases, acute kidney injury. The SmPC also highlights the risk of gallbladder disorders, including cholelithiasis and cholecystitis. Patients experiencing severe or persistent symptoms should seek medical advice and consider reporting suspected adverse reactions through the MHRA Yellow Card scheme.
Choosing the Right Probiotic Strains for GLP-1 Medications
Not all probiotic products are equivalent, and the clinical effects of probiotics are highly strain-specific. When considering probiotic supplementation alongside Ozempic, it is important to select formulations containing strains with evidence for addressing the particular gastrointestinal symptoms experienced. The most extensively studied probiotic genera include Lactobacillus, Bifidobacterium, and Saccharomyces, each encompassing numerous species and strains with distinct properties.
For nausea and general digestive discomfort, strains such as Lactobacillus rhamnosus GG have shown benefits in various gastrointestinal conditions, though specific data in the context of GLP-1 medications remain limited. For diarrhoea, Saccharomyces boulardii has robust evidence across multiple aetiologies, including antibiotic-associated diarrhoea as demonstrated in Cochrane reviews, and may theoretically help when diarrhoea occurs with semaglutide. However, S. boulardii should be avoided in immunocompromised patients and those with central venous catheters due to rare but serious risks of fungaemia. For constipation—which can also occur with Ozempic due to delayed gastric emptying—specific Bifidobacterium lactis strains (such as HN019 and BB-12) have shown promise in improving stool frequency and consistency in clinical trials of functional constipation.
Multi-strain formulations are widely available, though evidence for their superiority over single-strain products is product-specific rather than universal. When selecting a probiotic, it is advisable to choose products that clearly state the specific strains included and provide colony-forming unit (CFU) counts that match those used in clinical studies for the relevant condition. Rather than focusing on a generic CFU range, patients should follow manufacturer's instructions regarding dosage and storage to ensure viability.
Patients should be aware that probiotic supplements are not regulated as medicines by the MHRA but rather as food supplements, meaning quality and potency can vary between manufacturers. The International Scientific Association for Probiotics and Prebiotics (ISAPP) recommends selecting products with fully specified strain designations and quality assurances. Consulting a pharmacist or healthcare professional can help identify reputable products suited to individual symptom profiles. The NHS website also provides general guidance on probiotic supplements.
When to Take Probiotics Alongside Ozempic
The timing of probiotic administration in relation to Ozempic injections and meals may influence both the survival of probiotic organisms and their potential benefits. Ozempic is administered once weekly via subcutaneous injection, typically on the same day each week, and can be taken with or without food. According to the SmPC, the medication has a half-life of approximately one week, resulting in continuous effects on gastric emptying and gut motility throughout the dosing period, meaning gastrointestinal symptoms may occur at any time, though they are often most pronounced in the days following dose escalation.
Regarding optimal probiotic timing, evidence is mixed and highly variable between products. Some manufacturers recommend taking supplements on an empty stomach or with a small amount of food, while others produce acid-resistant formulations designed to survive gastric acid regardless of food intake. The evidence for specific timing strategies is limited and inconsistent, so patients should follow the specific instructions provided with their chosen probiotic product rather than adhering to generalised recommendations.
There is no known pharmacokinetic interaction that necessitates separation of probiotic intake from the weekly Ozempic injection. Probiotics can be taken daily throughout the week without concern for interfering with semaglutide absorption or action. For individuals experiencing predictable patterns of gastrointestinal symptoms—such as increased nausea in the 24–48 hours following their weekly Ozempic injection—some may choose to ensure consistent probiotic use during this period, though daily supplementation is generally recommended for sustained benefit.
During episodes of acute vomiting, it is practical to temporarily pause oral probiotic supplements until able to tolerate fluids and food again, then resume the regular schedule. It is worth noting that probiotic effects typically require several days to weeks of consistent use before benefits become apparent, so patience and adherence are important. Patients should continue their prescribed Ozempic regimen as directed by their clinician and not alter diabetes or weight management treatment based on probiotic use.
Evidence for Probiotics in Managing Digestive Side Effects
The evidence base for probiotic use specifically in patients taking GLP-1 receptor agonists such as Ozempic remains limited, with no large-scale randomised controlled trials published to date examining this particular clinical scenario. However, extrapolation from the broader literature on probiotics in gastrointestinal disorders provides some theoretical support for their potential utility. Systematic reviews and meta-analyses have demonstrated that certain probiotic strains can reduce the severity and duration of various digestive symptoms, including bloating, abdominal pain, and altered bowel habits in conditions such as irritable bowel syndrome (IBS).
Cochrane reviews examining probiotics for functional bowel disorders have found moderate-quality evidence that specific strains may improve global symptoms and quality of life, though effects varied considerably between studies and strains, with generally small effect sizes and significant heterogeneity. NICE Clinical Guideline 61 on IBS in adults suggests that patients who choose to try probiotics should take the product at the recommended dose for at least four weeks while monitoring the effect. For nausea specifically, the evidence is less robust, with most research focusing on pregnancy-related or chemotherapy-induced nausea rather than medication side effects.
It is important to emphasise that the absence of specific evidence for probiotics with Ozempic means recommendations must be cautious and individualised. NICE guidance on type 2 diabetes management (NG28) and obesity (TA875) does not currently include probiotics as part of standard care pathways. The decision to use probiotics should be made in consultation with healthcare professionals, considering the patient's symptom profile, overall health status, and preferences.
Patients should maintain realistic expectations, understanding that whilst probiotics may offer modest symptomatic relief for some individuals, they are not a substitute for appropriate dose titration, dietary modifications (such as smaller, more frequent meals), and other evidence-based strategies for managing GLP-1 medication side effects as recommended in the NHS guidance and SmPC. If gastrointestinal symptoms are severe or persistent despite conservative measures, medical review is essential to exclude other pathology and consider alternative management approaches.
Safety Considerations and Interactions with Semaglutide
Probiotics are generally considered safe for the majority of individuals, with a well-established safety profile in healthy populations. Common side effects, when they occur, are typically mild and transient, including temporary bloating, flatulence, or changes in bowel habit during the first few days of supplementation as the gut microbiota adjusts. These effects usually resolve with continued use or can be minimised by starting with a lower dose and gradually increasing to the recommended amount.
However, certain patient groups require particular caution when considering probiotic supplementation. Individuals who are severely immunocompromised, including those with HIV/AIDS with low CD4 counts, patients receiving chemotherapy, or those taking high-dose immunosuppressive medications, should consult their specialist before using probiotics due to rare reports of systemic infections caused by probiotic organisms. Patients with central venous catheters should specifically avoid Saccharomyces boulardii due to documented cases of fungaemia. Additionally, individuals with severe acute pancreatitis should avoid probiotics, as evidence from the PROPATRIA trial published in the New England Journal of Medicine suggests potential harm in this specific context.
Regarding interactions with semaglutide itself, there is no known pharmacokinetic or pharmacodynamic interaction between probiotics and Ozempic. Semaglutide is a peptide medication that does not undergo hepatic metabolism via cytochrome P450 enzymes, and probiotics do not affect the absorption or action of subcutaneously administered peptides. The delayed gastric emptying caused by semaglutide theoretically could affect the transit of orally administered probiotics, but this is unlikely to significantly impact their efficacy, as probiotics exert their effects primarily in the lower gastrointestinal tract.
Patients taking Ozempic for diabetes management should continue regular blood glucose monitoring as prescribed, as any changes in diet, including probiotic supplementation, could theoretically influence glycaemic control, though significant effects are unlikely. If new or worsening gastrointestinal symptoms develop after starting probiotics, or if symptoms attributed to Ozempic persist despite probiotic use and other management strategies, patients should contact their GP or diabetes specialist nurse. Severe symptoms such as persistent vomiting, signs of dehydration, severe abdominal pain, or blood in stools require prompt medical assessment to exclude serious complications. Right upper quadrant pain, fever, or jaundice could indicate gallbladder disease, which is a recognised risk with GLP-1 receptor agonists according to the SmPC. For urgent concerns outside of GP hours, patients should contact NHS 111 or seek emergency care as appropriate. Suspected adverse reactions to either Ozempic or probiotics should be reported through the MHRA Yellow Card scheme.
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- Ozempic - European Public Assessment Report.
- Type 2 diabetes in adults: management.
- Overweight and obesity management.
- GLP-1 receptor agonists: reminder of the potential side effects and to be aware of the potential for misuse.
- Utilization of Probiotics in Relieving Post-Colonoscopy Gastrointestinal Symptoms.
Frequently Asked Questions
Can I take probiotics with Ozempic safely?
Yes, probiotics are generally safe to take with Ozempic as there are no known pharmacological interactions between semaglutide and probiotic supplements. However, immunocompromised patients should consult their specialist before starting probiotics.
Which probiotic strains are best for Ozempic side effects?
Lactobacillus rhamnosus GG may help general digestive discomfort, Saccharomyces boulardii has evidence for diarrhoea, and Bifidobacterium lactis strains (HN019, BB-12) may improve constipation. Strain selection should match your specific symptoms.
How long does it take for probiotics to help with Ozempic side effects?
Probiotic effects typically require several days to weeks of consistent daily use before benefits become apparent. NICE guidance suggests trying probiotics for at least four weeks whilst monitoring symptom improvement.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












