Mounjaro®
Dual-agonist support that helps curb appetite, hunger, and cravings to drive substantial, sustained weight loss.
- ~22.5% average body weight loss
- Significant weight reduction
- Improves blood sugar levels
- Clinically proven weight loss

Recent reports have raised concerns about potential links between GLP-1 medications and vision problems, prompting questions about whether people are going blind from GLP-1 treatments. GLP-1 receptor agonists—including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda)—are widely prescribed for type 2 diabetes and weight management. Whilst research has identified a small increased risk of diabetic retinopathy progression in certain patients, particularly those with pre-existing eye disease, complete vision loss remains rare. Understanding the evidence, recognising who may be at higher risk, and maintaining appropriate eye screening can help patients benefit from these medications whilst protecting their sight.
Summary: GLP-1 medications are associated with a small increased risk of diabetic retinopathy progression in some patients, but complete vision loss is rare and most eye complications are manageable with early detection.
Glucagon-like peptide-1 (GLP-1) receptor agonists have become increasingly prescribed medications for managing type 2 diabetes and, more recently, for weight management. These medicines—including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda)—work by mimicking a natural hormone that regulates blood glucose levels and appetite. They stimulate insulin secretion when blood sugar is elevated, slow gastric emptying, and reduce appetite, leading to improved glycaemic control and often significant weight loss.
Recent media reports and emerging research have raised concerns about potential links between GLP-1 medications and certain eye conditions, particularly diabetic retinopathy—a complication of diabetes that can lead to vision loss if left untreated. People with diabetes already face an elevated risk of eye problems due to the underlying disease itself, which can damage the small blood vessels in the retina over time.
Researchers are investigating whether GLP-1 medications might influence the progression of existing eye disease. Additionally, there have been rare reports of non-arteritic anterior ischaemic optic neuropathy (NAION) in observational studies of semaglutide, though a causal relationship has not been established and regulatory authorities continue to monitor this signal.
The term "going blind" requires careful context. Complete vision loss is rare, and most eye complications associated with diabetes are manageable when detected early. Diabetic retinopathy progresses through stages, from mild background changes to more severe proliferative disease, and modern treatments including laser therapy and intravitreal injections can preserve vision in many cases. Understanding the nuanced relationship between GLP-1 medications and eye health helps patients and clinicians make informed decisions about treatment whilst maintaining appropriate monitoring.
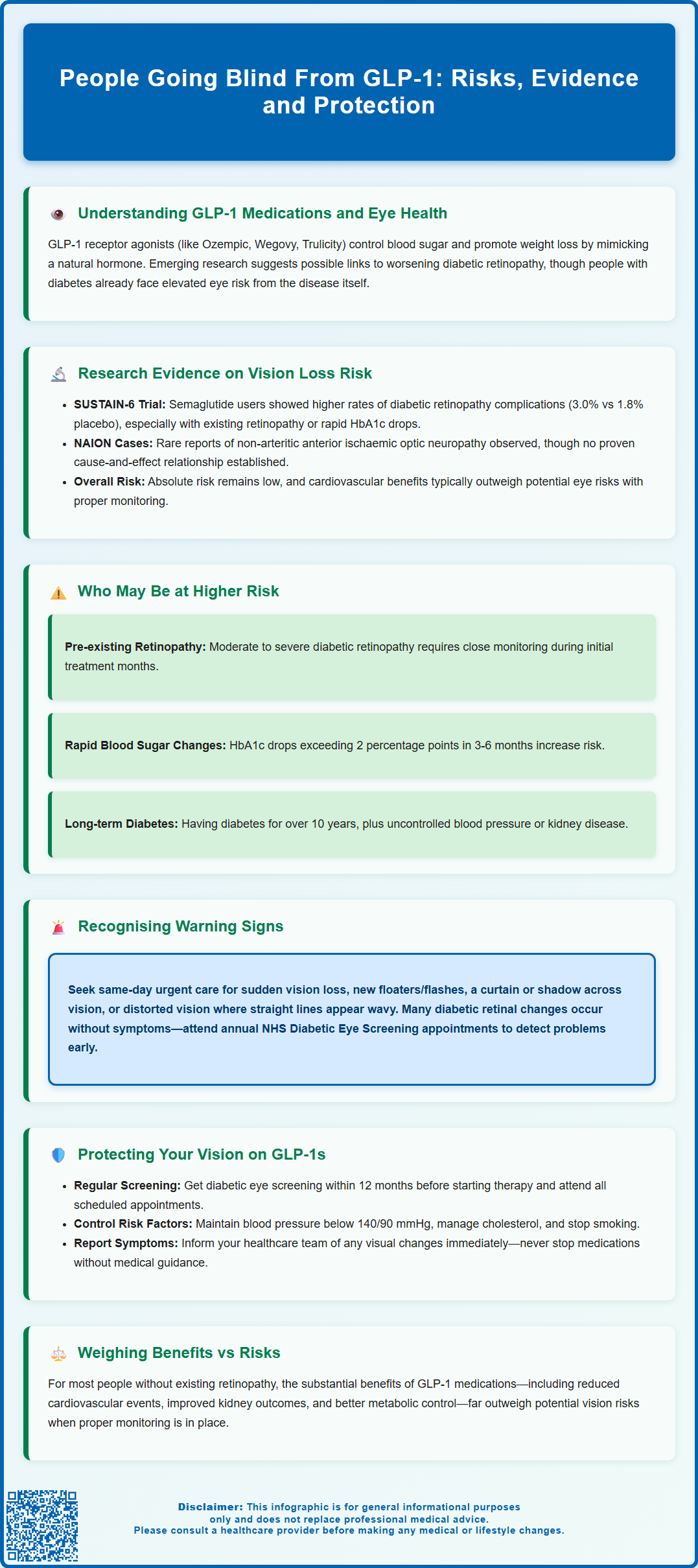
The primary evidence linking GLP-1 medications to eye complications comes from clinical trials and observational studies examining diabetic retinopathy progression. The SUSTAIN-6 trial, published in the New England Journal of Medicine in 2016, found that participants taking semaglutide had a higher rate of diabetic retinopathy complications compared to placebo (3.0% versus 1.8%). This risk was particularly concentrated in patients with pre-existing retinopathy and those experiencing rapid reductions in HbA1c.
Researchers have proposed that rapid improvement in blood glucose control—a therapeutic benefit of GLP-1 medications—may paradoxically worsen pre-existing diabetic retinopathy in the short term. This phenomenon, known as "early worsening," has been documented with intensive insulin therapy as well. When blood sugar levels drop quickly after prolonged periods of poor control, changes in retinal blood flow and increased vascular permeability may temporarily exacerbate retinal damage before longer-term benefits emerge.
A 2023 study published in JAMA Ophthalmology examined over 16,000 patients and found a small but statistically significant increased risk of certain retinal complications in those prescribed semaglutide compared to other diabetes medications. However, the absolute risk remained low, and the study's observational design could not definitively establish causation. Other research has shown conflicting results, with some studies suggesting neutral or even protective effects of GLP-1 medications on diabetic eye disease over longer follow-up periods.
Separately, observational studies have reported rare cases of non-arteritic anterior ischaemic optic neuropathy (NAION) in patients using semaglutide. While this signal is being monitored by the MHRA and EMA, causality has not been established.
The semaglutide Summary of Product Characteristics (SmPC) notes the diabetic retinopathy findings from SUSTAIN-6 and recommends appropriate monitoring for patients with diabetic retinopathy. The overall cardiovascular and metabolic benefits of GLP-1 therapy often outweigh potential risks when appropriate monitoring is in place.
Not everyone taking GLP-1 medications faces the same level of risk for eye complications. Individuals with pre-existing diabetic retinopathy appear to be the primary group requiring heightened vigilance. Those with moderate to severe non-proliferative diabetic retinopathy or proliferative disease at baseline may experience progression, particularly during the initial months of treatment when glycaemic control improves rapidly.
Other risk factors that may increase vulnerability include:
Long duration of diabetes (typically more than 10 years)
Poor glycaemic control prior to starting GLP-1 therapy (HbA1c significantly above target)
Rapid reduction in HbA1c (a drop of more than 2 percentage points [≈22 mmol/mol] within 3–6 months)
Concurrent hypertension, especially if poorly controlled
Diabetic kidney disease (nephropathy), which often correlates with retinopathy severity
Previous history of retinal treatment (laser photocoagulation or intravitreal injections)
People with type 2 diabetes but no retinopathy appear to have minimal risk of retinopathy progression based on current evidence. Those using GLP-1 medications solely for weight management (without diabetes) are not at risk for diabetic retinopathy progression, though they should report any visual symptoms promptly given the ongoing investigation of rare non-retinopathy eye events.
Anyone with diabetes should undergo regular diabetic eye screening regardless of medication type, as retinopathy can develop and progress silently without symptoms until advanced stages. The NHS Diabetic Eye Screening Programme provides annual screening for all people with diabetes aged 12 and over.
Clinicians often assess baseline retinopathy status before initiating GLP-1 therapy in high-risk individuals. NICE guidance recommends annual diabetic eye screening for all people with diabetes, with the frequency of ophthalmological review potentially adjusted based on individual clinical factors such as existing retinopathy and anticipated speed of glycaemic improvement.
Early detection of diabetic retinopathy progression is essential for preventing permanent vision loss. Many retinal changes occur without noticeable symptoms, which is why regular screening is vital. However, certain warning signs should prompt immediate medical attention, regardless of when your next scheduled eye examination is due.
Seek urgent assessment via NHS 111, eye casualty/A&E, or your GP if you experience:
Sudden vision loss or significant deterioration in either eye
Floaters (new dark spots or strings drifting through your vision), especially if numerous or increasing
Flashes of light in your peripheral vision
A curtain or shadow moving across your visual field
Distorted vision where straight lines appear wavy or bent
Difficulty reading or recognising faces that develops rapidly
Blurred vision that doesn't improve with blinking or resting your eyes
Eye pain with vision changes or a red, painful eye
These symptoms may indicate complications such as vitreous haemorrhage (bleeding into the gel-filled centre of the eye), retinal detachment, or diabetic macular oedema (swelling of the central retina). For sudden vision loss, a new 'curtain' over vision, or many new floaters/flashes, seek same-day urgent care.
For non-urgent concerns—such as gradual changes in vision, difficulty with night driving, or needing frequent prescription changes—contact your optometrist or GP within a few days. They can arrange appropriate referral to ophthalmology services if needed. If you're taking GLP-1 medications and notice any visual changes, inform your prescribing clinician, as they may wish to coordinate care with eye specialists. Remember that the NHS Diabetic Eye Screening Programme provides annual digital retinal photography for all people with diabetes aged 12 and over—ensure you attend these appointments, as they detect changes before symptoms develop.
If you're taking or considering GLP-1 therapy, several strategies can help protect your vision whilst benefiting from these medications' metabolic effects. Proactive monitoring and optimising overall diabetes management are key to minimising any potential risks.
Before starting GLP-1 medications:
Ensure you've had a recent diabetic eye screening (within the past 12 months)
Discuss your retinopathy status with your prescribing clinician
If you have known retinopathy, consider ophthalmology review before initiation
Understand that gradual dose titration may help avoid very rapid changes in blood glucose, which is a general principle in diabetes management
During treatment:
Attend all scheduled diabetic eye screening appointments without fail
If you have pre-existing retinopathy, your diabetes team may consider more frequent monitoring based on your individual clinical situation
Control blood pressure to target levels (below 140/90 mmHg, or below 130/80 mmHg if you have kidney, eye or cerebrovascular damage, if tolerated)
Maintain good overall glycaemic control whilst avoiding excessively rapid HbA1c reductions when possible
Stop smoking if applicable, as tobacco significantly worsens diabetic eye disease
Manage cholesterol levels according to NICE guidance for cardiovascular risk reduction
Communicate openly with your healthcare team about any visual symptoms, even if they seem minor. Report suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
The benefits of specific GLP-1 medications—including reduced cardiovascular events, improved kidney outcomes, and better quality of life—are substantial for many patients. For most people, particularly those without pre-existing retinopathy, these benefits far outweigh theoretical risks to vision.
If you have advanced diabetic retinopathy, your clinician may discuss alternative treatment options or ensure close collaboration between diabetes and ophthalmology services. Never discontinue GLP-1 medications without medical advice, as abrupt cessation may lead to deteriorating glycaemic control with its own risks. Instead, work with your healthcare team to develop an individualised monitoring plan that safeguards both your metabolic health and your vision for the long term.
GLP-1 medications are associated with a small increased risk of diabetic retinopathy progression in patients with pre-existing eye disease, particularly during rapid blood glucose improvement. Complete blindness is rare, and most complications are manageable with early detection through regular diabetic eye screening.
Individuals with pre-existing diabetic retinopathy, long diabetes duration (typically over 10 years), poor prior glycaemic control, and those experiencing rapid HbA1c reductions face the highest risk. People without diabetes using GLP-1s for weight management are not at risk for diabetic retinopathy progression.
Seek same-day urgent care for sudden vision loss, numerous new floaters, flashes of light, a curtain or shadow across your visual field, or distorted vision where straight lines appear wavy. These may indicate serious complications such as vitreous haemorrhage or retinal detachment requiring immediate assessment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
Unordered list
Bold text
Emphasis
Superscript
Subscript