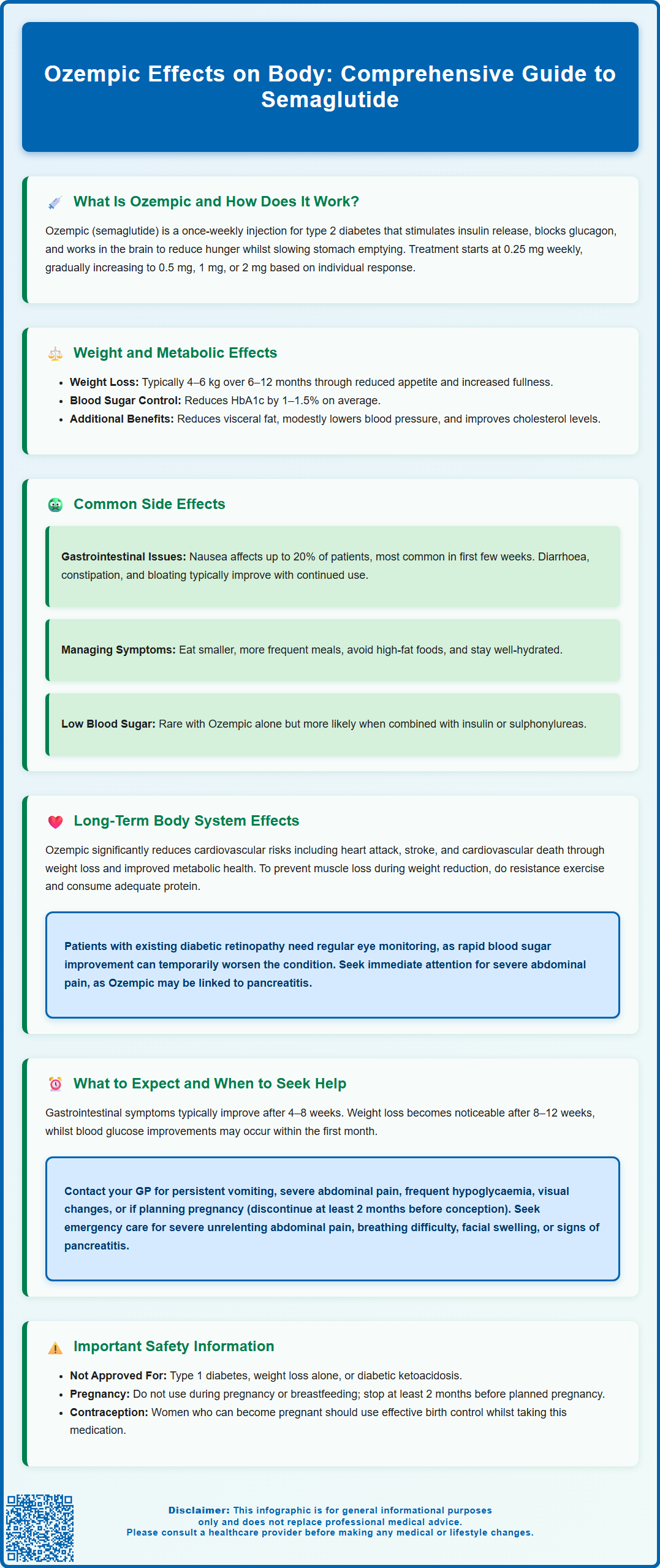
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for treating type 2 diabetes mellitus in adults. Administered as a once-weekly subcutaneous injection, Ozempic exerts multiple effects throughout the body by binding to GLP-1 receptors in the pancreas, brain, and gastrointestinal tract. It enhances glucose-dependent insulin secretion, suppresses glucagon release, slows gastric emptying, and influences appetite regulation. These mechanisms improve glycaemic control and often lead to weight reduction as a secondary effect. Understanding how Ozempic affects various body systems helps patients and clinicians optimise treatment outcomes whilst managing potential side effects. This article explores the comprehensive bodily effects of Ozempic, from metabolic changes to long-term system impacts.
Summary: Ozempic affects the body by stimulating insulin secretion, suppressing glucagon, slowing gastric emptying, and reducing appetite, leading to improved blood glucose control and weight reduction in adults with type 2 diabetes.
- Ozempic is a GLP-1 receptor agonist licensed by the MHRA for type 2 diabetes management, not weight loss.
- It works through glucose-dependent insulin release, glucagon suppression, delayed gastric emptying, and appetite regulation.
- Common side effects include gastrointestinal symptoms (nausea, diarrhoea, constipation), particularly during dose initiation.
- Long-term benefits include cardiovascular risk reduction and potential renoprotective effects in appropriate patients.
- Hypoglycaemia risk increases when combined with insulin or sulphonylureas; dose adjustments may be required.
- Patients should seek urgent medical attention for severe abdominal pain, persistent vomiting, or signs of pancreatitis.
Table of Contents
What Is Ozempic and How Does It Work in the Body?
Ozempic (semaglutide) is a prescription medication licensed by the Medicines and Healthcare products Regulatory Agency (MHRA) for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists, which mimic the action of a naturally occurring hormone in the body.
The mechanism of action of Ozempic involves binding to GLP-1 receptors found throughout the body, particularly in the pancreas, brain, and gastrointestinal tract. When administered as a once-weekly subcutaneous injection, semaglutide stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner—meaning it only promotes insulin release when blood glucose levels are elevated. Simultaneously, it suppresses the release of glucagon, a hormone that raises blood sugar, thereby helping to maintain glycaemic control.
Beyond its effects on glucose regulation, Ozempic influences appetite and satiety centres in the hypothalamus, leading to reduced hunger and increased feelings of fullness. It also slows gastric emptying, which means food remains in the stomach for longer periods. These combined actions contribute to both improved blood sugar management and, as a secondary effect, weight reduction.
Ozempic is initiated at 0.25 mg weekly for 4 weeks, which is a starter dose not intended for glycaemic control. The dose is then increased to 0.5 mg weekly, with further increases to 1 mg or 2 mg weekly possible for additional glycaemic control, depending on individual response and tolerability. The MHRA has approved Ozempic specifically for diabetes management, not for weight loss (which would be an off-label use), though its sister product Wegovy (also semaglutide) is licensed for weight management.
Importantly, Ozempic is not indicated for type 1 diabetes or for the treatment of diabetic ketoacidosis. It should not be used during pregnancy or breastfeeding, and treatment should be discontinued at least 2 months before a planned pregnancy. Effective contraception is advised for women of childbearing potential. Caution is also recommended in patients with severe gastrointestinal disease, such as gastroparesis.
Physical Effects of Ozempic on Weight and Metabolism
One of the most notable physical effects of Ozempic is its impact on body weight and metabolic parameters. Clinical trials in the SUSTAIN programme have demonstrated that patients with type 2 diabetes taking Ozempic experience significant weight reduction, typically ranging from 4–6 kg over 6–12 months, though individual responses vary considerably depending on baseline characteristics and dose used.
The weight loss associated with Ozempic occurs through multiple mechanisms. The medication's effect on appetite regulation leads to reduced caloric intake, as patients report feeling satisfied with smaller portions and experiencing fewer cravings. The delayed gastric emptying contributes to prolonged satiety after meals. There is also evidence suggesting that GLP-1 receptor agonists may influence energy expenditure and fat metabolism, though these effects are generally secondary to weight loss rather than direct mechanisms.
Metabolic improvements extend beyond weight reduction. Ozempic has been shown to:
-
Reduce HbA1c (a measure of long-term blood glucose control) by 1–1.5% on average, with variations depending on baseline levels and dose
-
Improve insulin sensitivity, primarily as a consequence of weight reduction
-
Reduce visceral adiposity (fat around internal organs) as part of overall weight loss, which is particularly beneficial for cardiovascular health
-
Lower blood pressure modestly in many patients
-
Improve lipid profiles, including reductions in triglycerides
It is important to note that weight loss is not universal—some patients experience minimal weight change whilst still achieving improved glycaemic control. The National Institute for Health and Care Excellence (NICE) recommends GLP-1 receptor agonists like Ozempic for patients who require additional glucose-lowering therapy when further treatment intensification is needed, particularly where weight loss would be beneficial. Local prescribing criteria may apply. Patients should maintain realistic expectations and understand that Ozempic works best when combined with dietary modifications and increased physical activity.
Common Side Effects and Bodily Changes with Ozempic
Like all medications, Ozempic can cause side effects, with gastrointestinal symptoms being the most frequently reported. Understanding these common effects helps patients distinguish between expected bodily changes and symptoms requiring medical attention.
Gastrointestinal effects are experienced by a significant proportion of patients, particularly during dose initiation and escalation:
-
Nausea (affecting up to 20% of patients) is typically most pronounced in the first few weeks and often diminishes with continued use
-
Diarrhoea or constipation may occur as the digestive system adjusts to slower gastric emptying
-
Abdominal discomfort, bloating, or indigestion are common but usually mild
-
Vomiting occurs less frequently but may necessitate dose adjustment
These gastrointestinal symptoms can be minimised by eating smaller, more frequent meals, avoiding high-fat foods, and ensuring adequate hydration. The gradual dose escalation protocol is specifically designed to improve tolerability. Persistent vomiting or diarrhoea can lead to dehydration and potential acute kidney injury, so prompt medical review is essential if unable to maintain adequate fluid intake.
Other common bodily changes include:
-
Injection site reactions such as redness, itching, or mild swelling, which typically resolve spontaneously
-
Fatigue during the initial weeks as the body adjusts to metabolic changes
-
Dizziness, particularly if blood glucose drops too low when Ozempic is combined with other diabetes medications
Hypoglycaemia (low blood sugar) is uncommon with Ozempic alone due to its glucose-dependent mechanism, but the risk increases when used alongside insulin or sulphonylureas. Doses of these medications may need to be reduced when starting or increasing Ozempic. Symptoms include trembling, sweating, confusion, and palpitations—patients should be educated on recognition and management.
Most side effects are mild to moderate and improve over time. However, persistent or severe symptoms warrant discussion with a healthcare professional, who may adjust the dose or recommend supportive measures. Patients should not discontinue Ozempic without medical advice, as this may lead to deterioration in glycaemic control.
Patients are encouraged to report suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Long-Term Effects of Ozempic on Body Systems
As Ozempic is used for extended periods in chronic disease management, understanding its long-term effects on various body systems is essential for both patients and clinicians.
Cardiovascular system: One of the most significant long-term benefits demonstrated in clinical trials is cardiovascular risk reduction. The SUSTAIN-6 trial showed that Ozempic reduced the risk of major adverse cardiovascular events (heart attack, stroke, or cardiovascular death) in patients with type 2 diabetes at high cardiovascular risk. This cardioprotective effect likely results from multiple factors including weight loss, blood pressure reduction, and improved metabolic parameters. While Ozempic does not have a specific cardiovascular prevention indication in the UK, NICE guidance acknowledges these cardiovascular benefits when recommending GLP-1 receptor agonists for appropriate patients.
Renal system: Emerging evidence suggests potential renoprotective effects, with some studies indicating slower progression of diabetic kidney disease. No dose adjustment is required in renal impairment according to the UK SmPC, though renal function should be monitored, especially if significant gastrointestinal adverse effects or dehydration occur.
Pancreatic considerations: There has been ongoing discussion regarding a potential association between GLP-1 receptor agonists and pancreatitis (inflammation of the pancreas). Whilst there is no definitive causal link established, patients should be aware of symptoms such as severe, persistent abdominal pain radiating to the back, and seek immediate medical attention if these occur. Treatment should be discontinued if pancreatitis is suspected. The MHRA continues to monitor this potential risk.
Thyroid effects: Animal studies identified an increased risk of thyroid C-cell tumours with GLP-1 receptor agonists, though the relevance to humans is unknown. Standard vigilance regarding thyroid symptoms is advised as per routine clinical practice.
Gallbladder effects: Rapid weight loss associated with Ozempic may increase the risk of gallstone formation. Cholelithiasis and cholecystitis have been reported with GLP-1 receptor agonists. Patients experiencing right upper abdominal pain, particularly after meals, should consult their GP.
Retinopathy considerations: Rapid improvement in blood glucose control has been associated with temporary worsening of diabetic retinopathy. Patients with pre-existing retinopathy should ensure appropriate ophthalmological monitoring when initiating or intensifying treatment.
Bone health and body composition: Some research suggests that weight loss with GLP-1 receptor agonists may include loss of lean muscle mass alongside fat mass. Patients are encouraged to engage in resistance exercise and ensure adequate protein intake to preserve muscle tissue during treatment.
Managing Ozempic's Effects: What to Expect and When to Seek Help
Successfully managing Ozempic therapy requires understanding what to expect during treatment and recognising when professional medical input is needed.
Initial expectations: During the first 4–8 weeks, patients commonly experience gastrointestinal adjustment symptoms. These typically improve as the body adapts. Weight loss, if it occurs, usually becomes noticeable after 8–12 weeks of treatment. Blood glucose improvements may be evident sooner, often within the first month.
Practical management strategies include:
-
Dietary modifications: Eating smaller portions, choosing low-fat options, and avoiding trigger foods can minimise nausea and digestive discomfort
-
Hydration: Maintaining adequate fluid intake helps manage constipation and supports overall wellbeing
-
Injection technique: Rotating injection sites (abdomen, thigh, or upper arm) reduces local reactions
-
Timing: Injections can be given at any time of day, with or without food. Some patients find that injecting before bed may reduce daytime nausea, though this is optional and should be based on individual preference. Maintaining a consistent weekly schedule is important.
-
Medication review: Discussing all medications with a GP or pharmacist ensures appropriate adjustments, particularly for other diabetes treatments
When to contact your GP or diabetes specialist:
-
Persistent vomiting preventing adequate fluid or food intake
-
Severe abdominal pain, especially if radiating to the back
-
Signs of hypoglycaemia occurring frequently
-
Unexplained persistent fatigue or weakness
-
Visual changes or symptoms of diabetic retinopathy worsening
-
Symptoms of dehydration (dark urine, dizziness, reduced urination)
-
If you become pregnant or are planning pregnancy (Ozempic should be discontinued at least 2 months before a planned pregnancy)
When to seek urgent medical attention (A&E or call 999):
-
Severe, unrelenting abdominal pain
-
Signs of severe allergic reaction (difficulty breathing, facial swelling, widespread rash)
-
Symptoms of severe hypoglycaemia with confusion or loss of consciousness
-
Symptoms suggesting pancreatitis or gallbladder inflammation
Regular follow-up appointments are essential for monitoring treatment response, adjusting doses, and screening for complications. People with pre-existing diabetic retinopathy should inform their clinician and ensure appropriate retinal monitoring when initiating or intensifying therapy. NICE recommends ongoing review of glycaemic control, weight, cardiovascular risk factors, and treatment tolerability. Patients should maintain open communication with their healthcare team and report any concerns promptly. Ozempic can be highly effective when properly managed, but success depends on collaborative care between patient and clinician, realistic expectations, and appropriate lifestyle modifications alongside pharmacotherapy.
Frequently Asked Questions
How quickly does Ozempic start affecting the body?
Blood glucose improvements may be evident within the first month of treatment, whilst weight loss typically becomes noticeable after 8–12 weeks. Gastrointestinal side effects are most common during the first 4–8 weeks as the body adjusts to the medication.
Does Ozempic affect organs other than the pancreas?
Yes, Ozempic affects multiple body systems including the cardiovascular system (reducing heart attack and stroke risk), kidneys (potential renoprotective effects), gastrointestinal tract (slowing gastric emptying), and brain (influencing appetite centres in the hypothalamus).
Can Ozempic's effects on the body be reversed if I stop taking it?
Most effects of Ozempic are reversible upon discontinuation, with blood glucose levels and appetite typically returning to pre-treatment states. However, stopping Ozempic without medical advice may lead to deterioration in glycaemic control, so any treatment changes should be discussed with your healthcare professional.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript