GLP-1 receptor agonists are increasingly prescribed for type 2 diabetes and weight management, but is GLP-1 safe for seniors? Older adults often have multiple health conditions, take several medications, and experience age-related physiological changes that can influence drug safety and tolerability. Whilst clinical evidence suggests GLP-1 medications can be used effectively in many older people, careful patient selection, appropriate dosing, and vigilant monitoring are essential. This article examines the safety profile of GLP-1 therapy in elderly patients, exploring potential risks, monitoring requirements, and key clinical considerations to support informed decision-making for older adults and their healthcare teams.
Summary: GLP-1 receptor agonists can be safe for seniors when prescribed with careful patient selection, appropriate dose titration, and regular monitoring of tolerability and comorbidities.
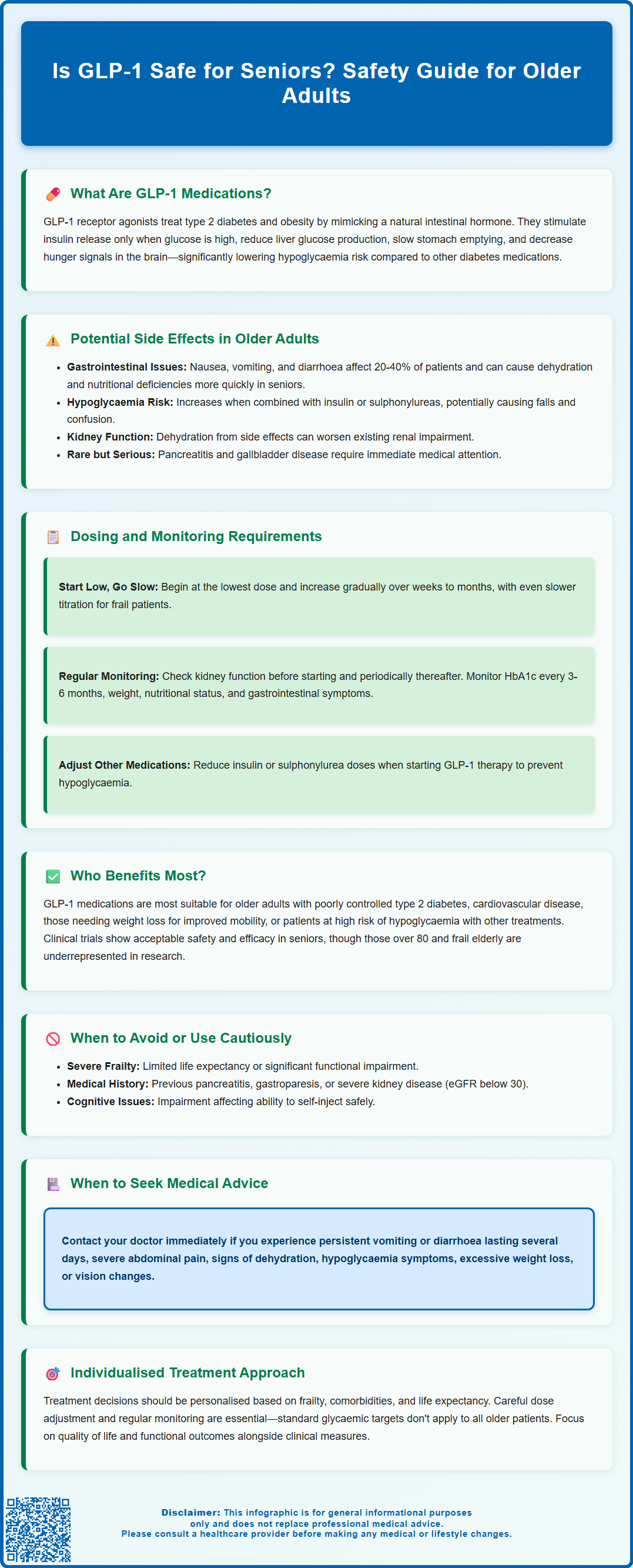
- GLP-1 medications work by enhancing insulin secretion, suppressing glucagon, delaying gastric emptying, and regulating appetite through glucose-dependent mechanisms.
- Common side effects include gastrointestinal symptoms (nausea, vomiting, diarrhoea), which may lead to dehydration and electrolyte imbalances more rapidly in older adults.
- Hypoglycaemia risk increases when GLP-1 agonists are combined with insulin or sulphonylureas, requiring careful medication review and dose adjustment.
- Initiation should follow a 'start low, go slow' approach with gradual dose titration, and renal function should be assessed before starting treatment.
- NICE guidance supports individualised glycaemic targets for older adults based on frailty, comorbidities, and hypoglycaemia risk rather than fixed targets.
- Patients should seek medical advice for persistent gastrointestinal symptoms, severe abdominal pain, dehydration, hypoglycaemia, or vision changes.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, obesity. These medicines mimic the action of naturally occurring GLP-1, a hormone produced in the intestine that plays a crucial role in glucose regulation and appetite control.
Mechanism of Action
GLP-1 receptor agonists work through several complementary pathways:
-
Enhanced insulin secretion: They stimulate the pancreas to release insulin in response to elevated blood glucose levels, but only when glucose is present—this glucose-dependent mechanism reduces the risk of hypoglycaemia.
-
Suppressed glucagon release: By inhibiting glucagon secretion from the pancreas, these medications prevent the liver from releasing excess glucose into the bloodstream.
-
Delayed gastric emptying: GLP-1 agonists slow the rate at which food leaves the stomach, leading to more gradual glucose absorption and increased satiety.
-
Appetite regulation: They act on centres in the brain that control hunger and fullness, helping to reduce overall caloric intake.
Available Preparations
In the UK, several GLP-1 receptor agonists are licensed and available through the NHS, including:
-
Semaglutide (Ozempic, Wegovy, and oral Rybelsus)
-
Dulaglutide (Trulicity)
-
Liraglutide (Victoza, Saxenda)
-
Exenatide (Byetta, Bydureon)
-
Lixisenatide (Lyxumia)
Most are administered via subcutaneous injection, with dosing frequencies ranging from twice daily to once weekly, depending on the specific formulation. Semaglutide is also available as an oral tablet (Rybelsus).
NICE guidance (NG28) supports their use in type 2 diabetes when glycaemic control is inadequate with other therapies. For weight management, NICE has approved semaglutide (Wegovy) for adults with a BMI of at least 35 kg/m² (or ≥30 kg/m² with weight-related comorbidities) within specialist weight management services. These medications are not indicated for type 1 diabetes or diabetic ketoacidosis.
Potential Side Effects and Risks in Older Adults
Whilst GLP-1 receptor agonists are generally well tolerated, older adults may experience certain adverse effects more acutely due to age-related physiological changes, polypharmacy, and comorbid conditions. Understanding these potential risks is essential for informed decision-making and appropriate monitoring.
Gastrointestinal Effects
The most commonly reported adverse effects are gastrointestinal in nature, including:
-
Nausea and vomiting (affecting 20-40% of patients initially, varying by agent and dose)
-
Diarrhoea or constipation
-
Abdominal discomfort and bloating
-
Reduced appetite
In elderly patients, persistent nausea and vomiting can lead to dehydration and electrolyte imbalances more rapidly than in younger adults. Frail older people may be particularly vulnerable to nutritional deficiencies if appetite suppression is excessive, potentially contributing to unintentional weight loss and sarcopenia.
Hypoglycaemia Risk
Whilst GLP-1 agonists alone carry a low intrinsic risk of hypoglycaemia due to their glucose-dependent mechanism, the risk increases substantially when combined with insulin or sulphonylureas—medications commonly prescribed to older adults with longstanding diabetes. Hypoglycaemic episodes in older adults can result in falls, confusion, and cardiovascular events.
Cardiovascular and Renal Considerations
Several GLP-1 receptor agonists (specifically liraglutide, semaglutide, and dulaglutide) have demonstrated cardiovascular benefits in clinical trials. However, older adults with severe heart failure or significant renal impairment require careful assessment, as dehydration from gastrointestinal side effects may exacerbate kidney function decline and increase acute kidney injury risk.
Diabetic Retinopathy Considerations
Rapid improvement in blood glucose control, particularly with semaglutide, has been associated with temporary worsening of diabetic retinopathy in some patients. Older adults with pre-existing retinopathy should have appropriate eye monitoring when starting treatment.
Other Potential Concerns
Rare but serious adverse effects include pancreatitis (presenting as severe abdominal pain), gallbladder disease, and potential thyroid effects. There is no established link between GLP-1 use and thyroid cancer in humans, though preclinical animal studies raised theoretical concerns. Older patients should be counselled to report persistent abdominal pain, jaundice, or unexplained symptoms promptly to their GP.
Suspected adverse reactions should be reported via the MHRA Yellow Card scheme.
Dosing and Monitoring Requirements for Elderly Patients
Appropriate dosing and vigilant monitoring are fundamental to maximising the benefits of GLP-1 therapy whilst minimising risks in older adults. Age-related changes in drug metabolism, renal function, and body composition necessitate a tailored approach.
Initiation and Dose Titration
GLP-1 receptor agonists should be initiated at the lowest available dose, with gradual titration over several weeks to months. This 'start low, go slow' approach helps mitigate gastrointestinal side effects, which are typically most pronounced during the initial weeks of therapy. For example:
-
Semaglutide: Usually started at 0.25 mg once weekly, increased to 0.5 mg after four weeks, with further escalation to 1 mg if required and tolerated.
-
Liraglutide: Commenced at 0.6 mg daily, with weekly increments of 0.6 mg up to the maintenance dose.
In frail elderly patients or those with multiple comorbidities, clinicians may opt for even slower titration schedules or lower maintenance doses to balance efficacy with tolerability.
Renal Function Assessment
Kidney function naturally declines with age, and renal considerations vary by agent. Baseline renal function (estimated glomerular filtration rate, eGFR) should be assessed before initiation, with periodic monitoring thereafter—particularly during intercurrent illness or dehydration:
-
Semaglutide, dulaglutide, and liraglutide do not require dose adjustment in renal impairment
-
Exenatide should be avoided in severe renal impairment (eGFR <30 mL/min/1.73m²)
-
All agents require caution if significant dehydration occurs due to gastrointestinal side effects
Ongoing Monitoring
Regular follow-up should include:
-
Glycaemic control: HbA1c monitoring every 3–6 months to assess diabetes management.
-
Weight and nutritional status: Ensuring weight loss is appropriate and not excessive, particularly in those at risk of malnutrition.
-
Gastrointestinal symptoms: Reviewing tolerance and adjusting doses if side effects persist.
-
Concomitant medications: Reviewing and potentially reducing doses of insulin or sulphonylureas to minimise hypoglycaemia risk.
-
Eye monitoring: For patients with pre-existing diabetic retinopathy, particularly when starting semaglutide.
-
Treatment response: As per NICE guidance, assess response after 6 months and continue only if adequate benefit is demonstrated (HbA1c reduction of at least 11 mmol/mol [1%] and/or 3% weight loss from initial body weight).
Patients should be educated on self-injection technique (if applicable), proper storage of medication, and recognition of adverse effects requiring medical attention. During periods of significant illness or dehydration, patients should seek medical advice and may need to temporarily interrupt treatment.
Is GLP-1 Safe for Older Adults? Key Safety Considerations
The safety of GLP-1 receptor agonists in older adults is a nuanced question that depends on individual patient characteristics, comorbidities, and careful clinical assessment. Evidence from clinical trials and real-world data suggests these medications can be used safely in many older people, but certain precautions are essential.
Evidence Base in Older Populations
Whilst landmark cardiovascular outcome trials included substantial numbers of older participants, dedicated studies focusing exclusively on elderly populations remain limited. Subgroup analyses generally indicate that GLP-1 agonists retain efficacy and acceptable safety profiles in older adults, with cardiovascular benefits observed across age groups. However, frail elderly patients and those over 80 years are often underrepresented in clinical trials, meaning real-world clinical judgement is paramount.
Patient Selection and Individualisation
GLP-1 therapy may be particularly appropriate for older adults who:
-
Have type 2 diabetes inadequately controlled on metformin or other oral agents
-
Require weight reduction to improve mobility and reduce cardiovascular risk
-
Have established cardiovascular disease and may benefit from cardioprotective effects
-
Are at high risk of hypoglycaemia with alternative therapies such as sulphonylureas
Conversely, caution or alternative treatments may be preferable in older adults with:
-
Severe frailty or limited life expectancy where intensive glycaemic control may not be beneficial
-
History of pancreatitis or significant gastrointestinal disorders, including gastroparesis
-
Cognitive impairment affecting ability to self-administer injections safely
-
Severe renal impairment (particularly for exenatide if eGFR <30 mL/min/1.73m²)
NICE Guidance and Clinical Recommendations
NICE guidance (NG28) on type 2 diabetes management supports GLP-1 use as part of a stepwise approach, with consideration of individual patient factors including age, comorbidities, and treatment goals. For older adults, glycaemic targets should be individualised based on frailty, comorbidities, and hypoglycaemia risk, rather than applying fixed targets.
For weight management, NICE has approved semaglutide (Wegovy) for adults with specific BMI criteria (≥35 kg/m² or ≥30 kg/m² with weight-related comorbidities) within specialist weight management services.
When to Seek Medical Advice
Patients and carers should contact their GP or diabetes specialist nurse if they experience:
-
Persistent nausea, vomiting, or diarrhoea lasting more than a few days
-
Severe abdominal pain, particularly if radiating to the back
-
Signs of dehydration (dizziness, reduced urine output, confusion)
-
Symptoms of hypoglycaemia (tremor, sweating, confusion)
-
Unexplained weight loss exceeding clinical targets
-
Changes in vision, particularly in those with pre-existing diabetic retinopathy
Suspected adverse reactions should be reported via the MHRA Yellow Card scheme.
Conclusion
GLP-1 receptor agonists can be safe and effective for many older adults when prescribed judiciously, with appropriate patient selection, careful dose titration, and regular monitoring. Shared decision-making between clinicians, patients, and families—considering individual health status, treatment goals, and quality of life—remains central to optimising outcomes in this population.
Frequently Asked Questions
Can older adults with kidney problems take GLP-1 medications?
Most GLP-1 receptor agonists (semaglutide, dulaglutide, liraglutide) do not require dose adjustment in renal impairment, though exenatide should be avoided if eGFR is below 30 mL/min/1.73m². Renal function should be assessed before starting treatment and monitored regularly, particularly during illness or dehydration.
What are the most common side effects of GLP-1 therapy in elderly patients?
The most common side effects are gastrointestinal, including nausea, vomiting, diarrhoea, and reduced appetite. These symptoms are typically most pronounced during initial weeks of therapy and can be minimised through gradual dose titration starting at the lowest available dose.
Should GLP-1 medications be stopped during illness in older adults?
During periods of significant illness or dehydration, patients should seek medical advice and may need to temporarily interrupt GLP-1 treatment to reduce the risk of acute kidney injury and electrolyte imbalances. Healthcare professionals can provide guidance on when to safely resume therapy.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










