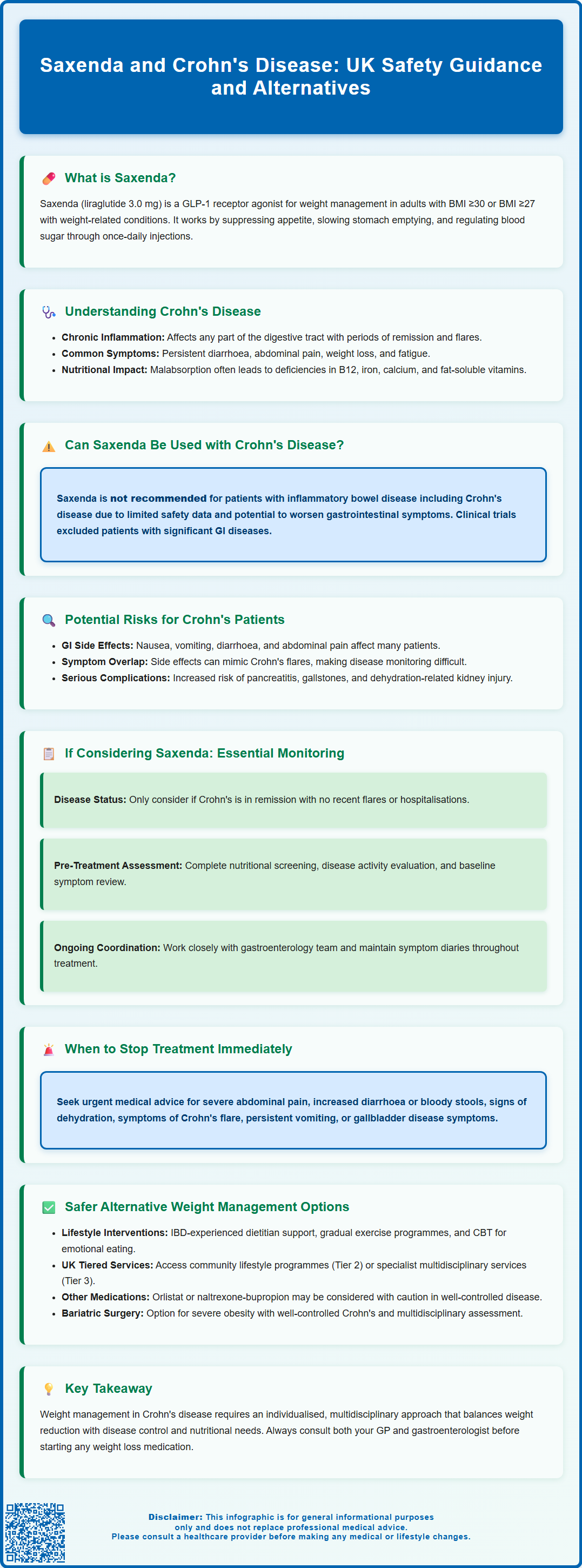
Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults and adolescents with obesity or overweight with comorbidities. However, its use in patients with Crohn's disease requires careful consideration. The UK Summary of Product Characteristics states that liraglutide is not recommended in patients with inflammatory bowel disease due to limited study data and potential gastrointestinal adverse effects. This article examines the safety considerations, potential risks, and alternative weight management options for individuals with Crohn's disease considering Saxenda treatment.
Summary: Saxenda is not recommended for patients with Crohn's disease according to UK prescribing guidance due to limited safety data and potential gastrointestinal adverse effects that may exacerbate inflammatory bowel disease symptoms.
- Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist that delays gastric emptying and commonly causes nausea, vomiting, diarrhoea, and abdominal pain.
- The UK Summary of Product Characteristics advises against liraglutide use in inflammatory bowel disease including Crohn's disease due to insufficient clinical trial data in this population.
- Gastrointestinal side effects may mask or worsen Crohn's disease symptoms, complicate nutritional management, and increase dehydration risk in affected patients.
- If Saxenda is considered despite recommendations, treatment requires comprehensive pre-assessment, disease remission confirmation, gastroenterology team collaboration, and close monitoring for adverse effects.
- Alternative weight management approaches include specialist dietetic support, lifestyle interventions, alternative pharmacotherapy (with caution), or bariatric surgery with multidisciplinary assessment for suitable candidates.
Table of Contents
- Understanding Saxenda and Its Mechanism of Action
- Crohn's Disease: Overview and Gastrointestinal Considerations
- Can Saxenda Be Used Safely in Patients with Crohn's Disease?
- Potential Risks and Gastrointestinal Side Effects of Saxenda
- Clinical Guidance and Monitoring for Crohn's Disease Patients Considering Saxenda
- Alternative Weight Management Options for Patients with Crohn's Disease
- Frequently Asked Questions
Understanding Saxenda and Its Mechanism of Action
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, such as type 2 diabetes, hypertension, or dyslipidaemia. It is also licensed for weight management in adolescents aged 12-17 years with obesity (BMI corresponding to ≥30 kg/m² in adults) and body weight above 60 kg.
Saxenda belongs to a class of medications known as glucagon-like peptide-1 (GLP-1) receptor agonists. Liraglutide is a synthetic analogue of human GLP-1, a naturally occurring incretin hormone released from the intestinal L-cells in response to food intake. GLP-1 plays a crucial role in glucose homeostasis and appetite regulation.
The mechanism of action of Saxenda involves several physiological pathways:
-
Appetite suppression: Liraglutide acts on GLP-1 receptors in the hypothalamus and other brain regions involved in appetite control, leading to increased satiety and reduced hunger.
-
Delayed gastric emptying: The medication slows the rate at which food leaves the stomach, prolonging feelings of fullness after meals.
-
Glucose regulation: Although primarily used for weight management at the 3.0 mg dose, liraglutide also enhances glucose-dependent insulin secretion and suppresses inappropriate glucagon release.
Saxenda is administered once daily via subcutaneous injection, typically in the abdomen, thigh, or upper arm. The dose is gradually increased over five weeks to minimise gastrointestinal side effects, starting at 0.6 mg daily and reaching the maintenance dose of 3.0 mg daily. Treatment should be used alongside a reduced-calorie diet and increased physical activity for optimal weight loss outcomes.
Importantly, treatment should be discontinued after 12 weeks on the 3.0 mg/day dose if patients have not lost at least 5% of their initial body weight. Regular evaluation of the benefit and risk of continued therapy is essential.
Saxenda is contraindicated in pregnancy and during breast-feeding. Key warnings include risks of pancreatitis, gallbladder disease, increased heart rate, dehydration leading to renal impairment, and suicidal ideation.
Crohn's Disease: Overview and Gastrointestinal Considerations
Crohn's disease is a chronic, relapsing inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract from mouth to anus, though it most commonly involves the terminal ileum and colon. The condition is characterised by transmural inflammation (affecting all layers of the bowel wall), which can lead to complications including strictures, fistulae, and abscesses.
The aetiology of Crohn's disease is multifactorial, involving genetic susceptibility, environmental triggers, intestinal microbiome alterations, and immune dysregulation. In the UK, the prevalence is estimated at approximately 145 per 100,000 people, with regional variations and increasing incidence rates. The condition typically presents in young adulthood, though it can occur at any age.
Common symptoms of Crohn's disease include:
-
Persistent diarrhoea (which may be bloody)
-
Abdominal pain and cramping
-
Weight loss and malnutrition
-
Fatigue and general malaise
-
Fever during active flares
Patients with Crohn's disease often experience periods of remission alternating with active disease flares. The gastrointestinal tract in these patients is particularly sensitive, and many individuals report food intolerances, altered bowel motility, and heightened visceral sensitivity.
Nutritional considerations are paramount in Crohn's disease management. Malabsorption, increased metabolic demands during inflammation, and dietary restrictions can lead to deficiencies in vitamins (particularly B12, folate, and fat-soluble vitamins), minerals (iron, calcium, magnesium), and protein. Conversely, some patients may experience weight gain during remission, particularly if treated with corticosteroids, which can increase appetite and promote central adiposity. According to NICE guidance (NG129), management should include regular nutritional assessment and dietetic input to optimise nutritional status whilst managing symptoms.
Red flags requiring urgent medical review include suspected intestinal obstruction, high fever suggesting sepsis, severe continuous abdominal pain, persistent vomiting leading to dehydration, and significant rectal bleeding with haemodynamic compromise.
Can Saxenda Be Used Safely in Patients with Crohn's Disease?
The use of Saxenda in patients with Crohn's disease requires careful consideration. According to the UK Summary of Product Characteristics (SmPC), liraglutide is not recommended in patients with inflammatory bowel disease and other severe gastrointestinal disease due to limited study data and the potential for gastrointestinal adverse effects.
While there is no absolute contraindication specifically listing Crohn's disease in the SmPC, the presence of inflammatory bowel disease introduces several important clinical considerations that warrant thorough evaluation before initiating treatment.
The primary concern relates to Saxenda's gastrointestinal effects. The medication's mechanism of delaying gastric emptying and its common gastrointestinal adverse effects (nausea, vomiting, diarrhoea, constipation, and abdominal pain) may potentially exacerbate symptoms in patients with active or even quiescent Crohn's disease. For individuals already experiencing compromised gastrointestinal function, these additional effects could significantly impact quality of life and disease management.
Clinical evidence specifically examining Saxenda use in Crohn's disease patients is limited. The pivotal clinical trials for liraglutide 3.0 mg (the SCALE programme) generally excluded patients with significant gastrointestinal diseases, including inflammatory bowel disease. This means there is insufficient data to definitively establish safety profiles in this specific population.
Key considerations for prescribers include:
-
Disease activity status: Patients with active Crohn's disease experiencing frequent diarrhoea, abdominal pain, or malabsorption are unlikely to be suitable candidates for Saxenda.
-
Nutritional status: Given that Crohn's disease can cause malnutrition and that Saxenda promotes weight loss, careful assessment of nutritional adequacy is essential.
-
Medication interactions: Patients with Crohn's disease often take immunosuppressants, biologics, or corticosteroids; whilst there are no known direct drug interactions with liraglutide, the overall treatment burden should be considered.
Decisions regarding Saxenda use in Crohn's disease patients should be made collaboratively between the prescribing clinician, the patient's gastroenterologist, and the patient themselves, with individualised risk-benefit assessment. If treatment is initiated, the 12-week stopping rule (discontinuation if <5% weight loss is achieved) should be strictly applied.
Potential Risks and Gastrointestinal Side Effects of Saxenda
Saxenda is associated with a range of gastrointestinal adverse effects, which are the most commonly reported side effects and the primary reason for treatment discontinuation. Understanding these effects is particularly important when considering use in patients with pre-existing gastrointestinal conditions such as Crohn's disease.
Very common gastrointestinal side effects (occurring in more than 1 in 10 patients) include:
-
Nausea: The most frequent adverse effect, typically most pronounced during dose escalation and often diminishing over time.
-
Vomiting: Often accompanies nausea, particularly in the initial treatment phase.
Common gastrointestinal side effects (occurring in between 1 in 100 and 1 in 10 patients) include:
-
Diarrhoea: Can range from mild to severe and may lead to dehydration if not managed appropriately.
-
Constipation: Affects a significant proportion of patients and may alternate with diarrhoea.
-
Abdominal pain and discomfort: May be difficult to distinguish from Crohn's-related pain in affected patients.
-
Dyspepsia: Indigestion and upper abdominal discomfort are frequently reported.
For patients with Crohn's disease, these effects could potentially:
-
Mimic or mask disease flare symptoms, making it difficult to distinguish medication side effects from disease activity
-
Exacerbate existing gastrointestinal symptoms, reducing quality of life
-
Complicate nutritional management and absorption of other medications
-
Increase the risk of dehydration, particularly if diarrhoea is already present
Serious risks associated with GLP-1 receptor agonists include:
-
Acute pancreatitis: Patients should be advised to seek immediate medical attention if they experience severe, persistent abdominal pain radiating to the back, as this may indicate pancreatitis. Treatment should be discontinued if pancreatitis is confirmed.
-
Gallbladder disease: Liraglutide has been associated with an increased risk of cholelithiasis (gallstones) and cholecystitis. Patients should seek medical attention for right upper quadrant pain, fever, or jaundice.
-
Dehydration and acute kidney injury: Gastrointestinal side effects may lead to dehydration, which can impair renal function. Adequate hydration is essential, and renal function should be monitored in at-risk patients.
Patients should be advised to report any suspected side effects to their healthcare professional or directly to the MHRA Yellow Card Scheme.
Clinical Guidance and Monitoring for Crohn's Disease Patients Considering Saxenda
If Saxenda is being considered for a patient with Crohn's disease, despite the SmPC recommendation against use in inflammatory bowel disease, a comprehensive pre-treatment assessment is essential. This should include collaboration with the patient's gastroenterology team to ensure coordinated care and appropriate monitoring.
Pre-treatment evaluation should include:
-
Disease activity assessment: Confirm that Crohn's disease is in remission or well-controlled. Patients with active inflammation, frequent flares, or recent hospitalisations are generally not suitable candidates.
-
Nutritional status: Conduct thorough nutritional assessment including BMI, body composition, and screening for deficiencies (full blood count, vitamin B12, folate, vitamin D, iron studies, albumin). Weight loss therapy should only be considered if the patient is genuinely overweight or obese and nutritionally replete.
-
Gastrointestinal symptom baseline: Document current bowel frequency, consistency (using Bristol Stool Chart), and any abdominal pain to enable comparison during treatment.
-
Structural complications: Review recent imaging or endoscopy results to identify strictures, fistulae, or other complications that might increase risk.
-
Current medications: Review all medications, particularly those affecting gastrointestinal motility or absorption.
-
Cardiovascular assessment: Check baseline heart rate and blood pressure, as liraglutide can increase heart rate.
Monitoring during treatment should be individualised according to local specialist weight management service protocols and the patient's IBD team recommendations:
-
Initial phase: Regular contact during dose escalation (first 5 weeks) to assess tolerability and gastrointestinal symptoms.
-
Ongoing monitoring: Regular reviews in line with local Tier 3/4 weight management service protocols.
-
Symptom tracking: Patients should maintain a symptom diary recording bowel movements, abdominal pain, and any new symptoms.
-
Weight and nutritional parameters: Regular monitoring to ensure weight loss is appropriate and not excessive; repeat nutritional blood tests as clinically indicated.
-
12-week assessment: Evaluate weight loss at 12 weeks on the 3.0 mg dose; discontinue treatment if less than 5% of initial body weight has been lost.
When to stop treatment or seek urgent advice:
-
Severe or persistent abdominal pain
-
Significant increase in diarrhoea frequency or blood in stools
-
Signs of dehydration (reduced urine output, dizziness, dry mouth)
-
Symptoms suggesting Crohn's flare (fever, weight loss beyond expected, severe fatigue)
-
Inability to tolerate oral intake due to nausea or vomiting
-
Right upper quadrant pain, jaundice or fever (possible gallbladder disease)
Patients should have direct access to their gastroenterology team and clear instructions on when to seek urgent medical review.
Alternative Weight Management Options for Patients with Crohn's Disease
For patients with Crohn's disease who require weight management but for whom Saxenda may not be appropriate, several alternative approaches should be considered. NICE guidance on obesity management (CG189) emphasises a multimodal approach tailored to individual circumstances.
Lifestyle interventions remain the foundation of weight management:
-
Dietary modification: Working with a specialist dietitian experienced in IBD is crucial. Approaches should balance calorie reduction with nutritional adequacy and symptom management. Low-FODMAP diets, whilst helpful for IBS-type symptoms, should be used cautiously and with professional guidance to avoid nutritional deficiencies.
-
Physical activity: Regular exercise is beneficial for both weight management and Crohn's disease outcomes. A gradual, individualised exercise programme should be developed, considering the patient's current fitness level and disease activity. Activities such as walking, swimming, or cycling may be better tolerated than high-impact exercises.
-
Behavioural support: Psychological interventions including cognitive behavioural therapy (CBT) can address emotional eating, body image concerns, and the psychological impact of living with chronic disease.
Pharmacological alternatives to consider:
-
Orlistat: This lipase inhibitor reduces dietary fat absorption and may be better tolerated than GLP-1 agonists in some patients. However, it can cause gastrointestinal side effects (particularly steatorrhoea and faecal urgency) which may be problematic in Crohn's disease. It should be used with caution and only in patients with well-controlled disease.
-
Naltrexone-bupropion (Mysimba): This is licensed in the UK for weight management, although availability through NHS services may vary as NICE has not completed an appraisal. It has different side effects from GLP-1 agonists but should still be used with caution in IBD.
-
Semaglutide (Wegovy): Recently approved in the UK (NICE TA875) for weight management. As another GLP-1 receptor agonist, it has a similar gastrointestinal side effect profile to liraglutide and the same cautions would apply regarding use in inflammatory bowel disease.
Bariatric surgery may be considered for patients with severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities) who have not responded to other interventions. However, Crohn's disease presents specific considerations:
-
Disease activity should be well-controlled before considering surgery
-
Careful surgical planning is required, particularly if there is previous bowel resection or known strictures
-
Procedure selection should be individualised based on the patient's specific IBD history and anatomy
-
Multidisciplinary team assessment including gastroenterology input is essential
UK tiered weight management services provide structured support:
-
Tier 2: Community-based lifestyle interventions
-
Tier 3: Specialist multidisciplinary weight management services
-
Tier 4: Bariatric surgery and associated care
Referral pathways typically start with the GP or can be initiated by specialist teams. Patients with complex needs such as Crohn's disease often benefit from Tier 3 services before considering pharmacotherapy or surgery.
Ultimately, weight management in Crohn's disease requires an individualised, multidisciplinary approach that prioritises disease control, nutritional adequacy, and overall wellbeing alongside weight reduction goals. Patients should be supported to make informed decisions based on comprehensive discussion of risks and benefits for their specific circumstances.
Frequently Asked Questions
Is Saxenda safe for people with Crohn's disease?
Saxenda is not recommended for patients with Crohn's disease according to UK prescribing guidance. The medication's gastrointestinal side effects, including nausea, vomiting, and diarrhoea, may worsen symptoms in patients with inflammatory bowel disease, and there is limited clinical trial data in this population.
What are the main risks of using Saxenda with Crohn's disease?
The main risks include exacerbation of gastrointestinal symptoms, difficulty distinguishing medication side effects from disease flares, increased dehydration risk, complications in nutritional management, and potential for acute pancreatitis or gallbladder disease which may be harder to diagnose in patients with existing bowel inflammation.
What weight management alternatives exist for Crohn's disease patients?
Alternatives include specialist dietetic support tailored to inflammatory bowel disease, structured lifestyle interventions through NHS tiered weight management services, cautious use of alternative medications such as orlistat (with gastroenterology input), and bariatric surgery for suitable candidates with well-controlled disease following multidisciplinary assessment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript