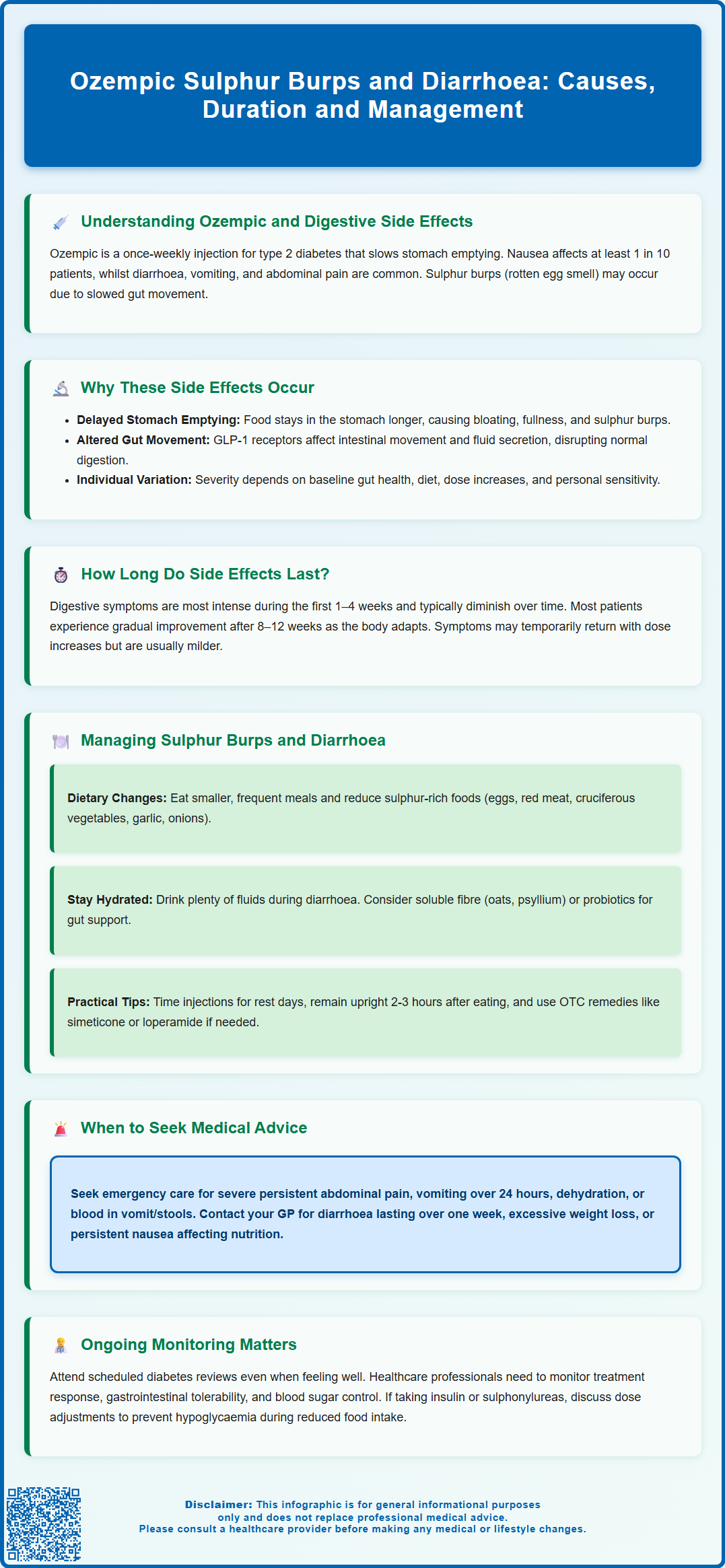
Ozempic (semaglutide), a GLP-1 receptor agonist for type 2 diabetes, commonly causes gastrointestinal side effects including diarrhoea and sulphur burps. These symptoms result from the medication's mechanism of slowing gastric emptying and affecting gut motility. Whilst not always listed in official prescribing information, sulphurous eructation is frequently reported alongside nausea, diarrhoea, and abdominal discomfort. Most digestive symptoms are dose-dependent, occurring during treatment initiation or dose escalation, and typically improve over time. Understanding why these effects occur and how to manage them effectively can help patients maintain treatment adherence whilst minimising discomfort and ensuring safe diabetes management.
Summary: Ozempic commonly causes sulphur burps and diarrhoea by slowing gastric emptying and altering gut motility through GLP-1 receptor activation.
- Semaglutide is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes treatment, administered as a once-weekly subcutaneous injection.
- Gastrointestinal side effects including nausea, diarrhoea, and sulphurous eructation result from delayed gastric emptying and altered intestinal function.
- Symptoms typically peak during treatment initiation and dose escalation, gradually diminishing over 8–12 weeks in most patients.
- Dietary modifications including smaller meals, reduced sulphur-rich foods, and adequate hydration form the cornerstone of symptom management.
- Seek urgent medical attention for severe persistent abdominal pain, persistent vomiting, blood in stools, or signs of dehydration.
- Dose escalation can be delayed by 4 weeks if adverse effects persist, and treatment is not recommended for patients with severe gastrointestinal disease.
Table of Contents
- Understanding Ozempic and Common Gastrointestinal Side Effects
- Why Ozempic Causes Sulphur Burps and Diarrhoea
- How Long Do Digestive Side Effects Last on Ozempic?
- Managing Sulphur Burps and Diarrhoea While Taking Ozempic
- When to Seek Medical Advice About Ozempic Side Effects
- Scientific References
- Frequently Asked Questions
Understanding Ozempic and Common Gastrointestinal Side Effects
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, it works by enhancing insulin secretion, suppressing glucagon release, and slowing gastric emptying. Whilst Ozempic has demonstrated significant efficacy in glycaemic control and, in adults with type 2 diabetes and established cardiovascular disease, cardiovascular risk reduction, gastrointestinal side effects are amongst the most commonly reported adverse reactions.
According to the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA), gastrointestinal disturbances affect a substantial proportion of patients initiating Ozempic therapy. The most frequently documented effects include:
-
Nausea (very common, affecting ≥1/10 patients)
-
Diarrhoea (common, affecting ≥1/100 to <1/10 patients)
-
Vomiting (common, affecting ≥1/100 to <1/10 patients)
-
Abdominal pain and distension (common)
-
Constipation (common)
-
Dyspepsia and gastro-oesophageal reflux (common)
Whilst not explicitly listed in the SmPC as a distinct adverse effect, many patients anecdotally report experiencing sulphur burps (eructation with a characteristic hydrogen sulphide odour) alongside other digestive symptoms. These burps, medically termed sulphurous eructation, may potentially relate to the medication's effect on gastrointestinal motility, though the exact mechanism remains unconfirmed.
Most gastrointestinal side effects are dose-dependent and tend to be most pronounced during treatment initiation or dose escalation. The standard titration schedule—starting at 0.25 mg weekly and gradually increasing to maintenance doses of 0.5 mg, 1 mg or 2 mg—is specifically designed to minimise these effects. Understanding the potential digestive symptoms can help patients and healthcare professionals implement appropriate management strategies and set realistic expectations for treatment tolerance.
Why Ozempic Causes Sulphur Burps and Diarrhoea
The gastrointestinal side effects associated with Ozempic stem directly from its pharmacological mechanism of action. As a GLP-1 receptor agonist, semaglutide binds to GLP-1 receptors distributed throughout the gastrointestinal tract, pancreas, and central nervous system. This binding triggers several physiological responses that, whilst therapeutically beneficial for diabetes management, can produce unwanted digestive symptoms.
Delayed gastric emptying represents the primary mechanism underlying many gastrointestinal effects. Ozempic significantly slows the rate at which food moves from the stomach into the small intestine—a process that contributes to improved postprandial glucose control and enhanced satiety. However, this prolonged gastric retention means food remains in the stomach for extended periods, potentially leading to:
-
Feelings of fullness, bloating, and nausea
-
Possible increased gastric fermentation
-
Changes in digestive processes that may contribute to sulphur-containing eructations
Diarrhoea associated with Ozempic likely results from multiple factors. The medication affects intestinal motility and fluid secretion through GLP-1 receptor activation in the gut. Additionally, the altered gastric emptying pattern may affect the normal digestive process. Changes in gut function may contribute to loose stools, though the precise mechanisms continue to be studied.
The intensity of these effects varies considerably between individuals, influenced by factors including baseline gastrointestinal function, dietary habits, dose escalation speed, and individual sensitivity to GLP-1 receptor activation. It's important to note that according to the MHRA SmPC, Ozempic is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis.
Patients should also be aware that GLP-1 receptor agonists like Ozempic have been associated with an increased risk of gallbladder events, including cholelithiasis (gallstones) and cholecystitis (gallbladder inflammation), which may present as right upper abdominal pain, particularly after fatty meals.
How Long Do Digestive Side Effects Last on Ozempic?
For most patients, gastrointestinal side effects associated with Ozempic follow a predictable temporal pattern, with symptoms typically being most pronounced during the initial weeks of treatment and following dose increases. Understanding this timeline helps patients maintain realistic expectations and persist with therapy when clinically appropriate.
Initial treatment phase (weeks 1–4): During the starting dose of 0.25 mg weekly, patients commonly experience mild to moderate nausea, occasional sulphur burps, and changes in bowel habits. Based on clinical trials summarised in the European Medicines Agency's European Public Assessment Report (EPAR), gastrointestinal symptoms are among the most common adverse events during this period. These effects may begin within days of the first injection and can vary throughout the week.
Dose escalation periods: When increasing from 0.25 mg to 0.5 mg (typically after 4 weeks), and subsequently to 1 mg or 2 mg if required, patients may experience a temporary resurgence of digestive symptoms. This recurrence is normal and generally less severe than initial symptoms. Importantly, the SmPC notes that dose escalation can be delayed by an additional 4 weeks if adverse effects persist, allowing for better tolerability.
Long-term treatment (beyond 8–12 weeks): For the majority of patients who continue Ozempic, gastrointestinal side effects gradually diminish over time as physiological adaptation occurs. However, some patients may continue to experience persistent symptoms that necessitate dose adjustment or treatment discontinuation.
Individual variation is considerable—some patients report complete resolution of symptoms within weeks, whilst others may experience intermittent digestive disturbances throughout treatment. Factors affecting symptom duration include dietary modifications, hydration status, concurrent medications, and individual gastrointestinal sensitivity. If symptoms persist beyond 12 weeks or significantly impact quality of life, medical review is warranted to assess whether continued therapy remains appropriate.
Managing Sulphur Burps and Diarrhoea While Taking Ozempic
Effective management of gastrointestinal side effects can significantly improve treatment tolerance and adherence to Ozempic therapy. Dietary modifications represent the cornerstone of symptom management and should be implemented from treatment initiation:
Dietary strategies to reduce sulphur burps:
-
Reduce sulphur-rich foods including eggs, red meat, cruciferous vegetables (broccoli, cauliflower, Brussels sprouts), garlic, and onions
-
Eat smaller, more frequent meals rather than large portions that overwhelm delayed gastric emptying
-
Avoid carbonated beverages which can exacerbate bloating and eructation
-
Limit high-fat foods that further slow gastric emptying
-
Chew food thoroughly and eat slowly to reduce air swallowing (aerophagia)
-
Stay upright for 2–3 hours after eating to facilitate digestion
Managing diarrhoea:
-
Maintain adequate hydration with water and oral rehydration solutions if needed (available from pharmacies)
-
Consider temporarily reducing foods that may trigger symptoms such as spicy foods, caffeine, alcohol, and artificial sweeteners
-
Include soluble fibre such as oats and psyllium, which can help regulate bowel movements
-
Consider probiotic supplementation after discussion with a healthcare professional
-
A short-term trial of a low-FODMAP diet may be considered with guidance from a healthcare professional or dietitian if symptoms are severe
Pharmacological interventions may be appropriate for persistent symptoms. Over-the-counter remedies such as simeticone (for gas and bloating) or loperamide (for diarrhoea) can provide symptomatic relief, though patients should consult their GP or pharmacist before regular use. Loperamide should not be used if there is blood in the stool, high fever, or for more than 48 hours without medical advice.
For severe nausea, prescription antiemetics may be considered under healthcare professional guidance. Patients should be aware that medications like domperidone have MHRA restrictions due to cardiac risks, and metoclopramide should not be used for more than 5 days due to neurological side effect risks.
Injection timing can also influence symptom severity. Some patients find that administering Ozempic on a day when they can rest helps them manage initial post-injection symptoms more comfortably.
Patients taking insulin or sulfonylureas alongside Ozempic should monitor blood glucose levels carefully during periods of reduced food intake, as the risk of hypoglycaemia may increase. Dose adjustments of these medications may be necessary under healthcare professional guidance.
If symptoms remain troublesome despite these measures, dose adjustment may be necessary. This might involve maintaining a lower dose for a longer period before escalation, or accepting a sub-maximal maintenance dose that balances efficacy with tolerability.
When to Seek Medical Advice About Ozempic Side Effects
Whilst mild to moderate gastrointestinal symptoms are expected with Ozempic therapy, certain presentations warrant prompt medical assessment to exclude serious complications or conditions requiring intervention. Patients should be counselled on red flag symptoms before initiating treatment.
Seek urgent medical attention (A&E or call 999) if experiencing:
-
Severe, persistent abdominal pain that is constant or worsening, particularly if localised to the upper abdomen or radiating to the back (potential pancreatitis)
-
Persistent vomiting preventing oral fluid intake for more than 24 hours (risk of dehydration and acute kidney injury)
-
Signs of dehydration including reduced urine output, dizziness, confusion, or rapid heartbeat
-
Blood in vomit or stools (haematemesis or melaena)
-
Severe allergic reactions such as facial swelling, difficulty breathing, or widespread rash
Contact your GP or diabetes specialist nurse within 24–48 hours for:
-
Diarrhoea persisting beyond one week or more than 6–8 loose stools daily
-
Unintentional weight loss exceeding 1–2 kg per week
-
Symptoms significantly impacting daily activities or quality of life
-
New or worsening abdominal pain that is moderate in severity
-
Persistent nausea preventing adequate nutritional intake
-
Symptoms of gallbladder disease including right upper quadrant pain, particularly after fatty meals
-
Worsening vision or eye symptoms, particularly in patients with pre-existing diabetic retinopathy
Routine review is appropriate for:
-
Mild, manageable symptoms that are improving with dietary modifications
-
Questions about symptom management strategies
-
Discussion of dose adjustment if symptoms are troublesome but not severe
If unsure about the urgency of symptoms, contact NHS 111 for advice.
NICE guidance recommends regular monitoring of patients on GLP-1 receptor agonists, including assessment of gastrointestinal tolerability, weight changes, and glycaemic control. Patients should attend scheduled diabetes reviews even if feeling well, as these appointments allow healthcare professionals to evaluate treatment response and identify any emerging concerns.
It is important to note that the Ozempic SmPC contains a precaution regarding thyroid C-cell tumours based on animal studies, though there is no established link in humans. Nevertheless, patients experiencing persistent neck lumps, hoarseness, or difficulty swallowing should seek medical evaluation.
Patients taking insulin or sulfonylureas alongside Ozempic should seek advice about dose adjustments if experiencing reduced food intake due to gastrointestinal symptoms, as the risk of hypoglycaemia may increase in these circumstances.
Scientific References
Frequently Asked Questions
How long do sulphur burps and diarrhoea last when taking Ozempic?
Most patients experience gastrointestinal symptoms during the initial 4 weeks and following dose increases, with gradual improvement over 8–12 weeks. Individual variation is considerable, and some patients may experience intermittent symptoms throughout treatment.
Can I take loperamide for Ozempic-related diarrhoea?
Loperamide may provide symptomatic relief for diarrhoea, but consult your GP or pharmacist before regular use. Do not use loperamide if there is blood in the stool, high fever, or for more than 48 hours without medical advice.
What foods should I avoid to reduce sulphur burps on Ozempic?
Reduce sulphur-rich foods including eggs, red meat, cruciferous vegetables (broccoli, cauliflower, Brussels sprouts), garlic, onions, and carbonated beverages. Eating smaller, more frequent meals and avoiding high-fat foods can also help minimise symptoms.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript