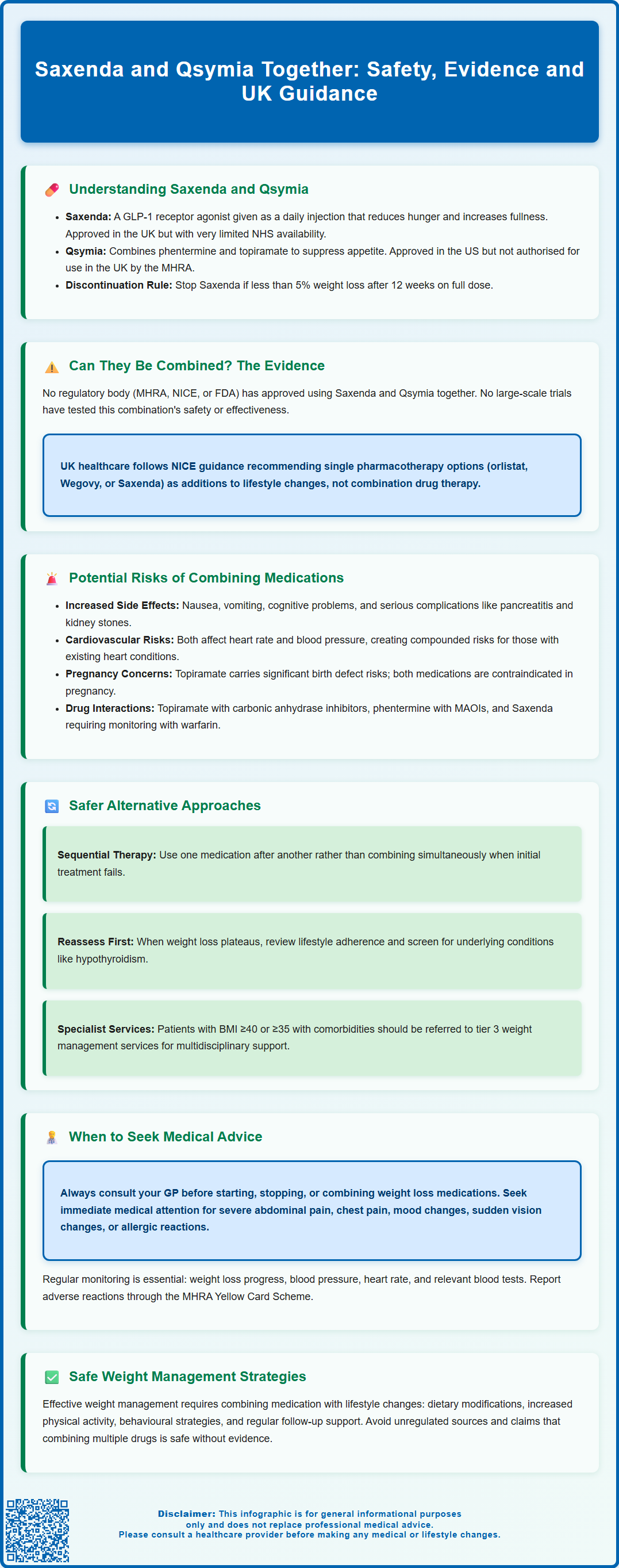
Saxenda (liraglutide 3.0 mg) and Qsymia (phentermine/topiramate extended-release) are prescription weight management medications with distinct regulatory statuses in the UK. Whilst Saxenda is MHRA-approved and available through specialist NHS services, Qsymia has not received UK or European authorisation. Patients sometimes enquire about using Saxenda and Qsymia together to enhance weight loss outcomes. However, no clinical trials have evaluated this combination, and neither the MHRA, NICE, nor international regulators endorse concurrent use. This article examines the evidence, safety considerations, and appropriate clinical pathways for weight management in the UK context.
Summary: There is no regulatory approval or clinical evidence supporting the combined use of Saxenda and Qsymia for weight management.
- Saxenda (liraglutide) is a GLP-1 receptor agonist approved by the MHRA; Qsymia (phentermine/topiramate) is not authorised in the UK or EU.
- No clinical trials have assessed the safety or efficacy of using these medications together.
- Combining weight loss drugs may increase adverse effects including cardiovascular risks, gastrointestinal symptoms, and metabolic complications.
- NICE guidance recommends pharmacotherapy as an adjunct to lifestyle interventions, with regular monitoring by healthcare professionals.
- Patients should consult their GP before starting any weight loss medication and seek specialist referral for complex obesity management.
Table of Contents
- Understanding Saxenda and Qsymia: Mechanisms and Approved Uses
- Can Saxenda and Qsymia Be Taken Together? Current Evidence and Regulatory Position
- Potential Risks and Drug Interactions of Combining Weight Loss Medications
- Alternative Approaches: Sequential Use and Combination Therapy Under Medical Supervision
- When to Seek Medical Advice: Safe Weight Management Strategies
- Frequently Asked Questions
Understanding Saxenda and Qsymia: Mechanisms and Approved Uses
Saxenda (liraglutide 3.0 mg) and Qsymia (phentermine/topiramate extended-release) are prescription medications licensed for weight management, though their availability and regulatory status differ between the UK and other jurisdictions. Saxenda is approved by the MHRA in the UK, but has restricted NHS availability through specialist (tier 3) weight management services for specific patient groups. Qsymia is licensed in the United States but was refused authorisation by the European Medicines Agency and is not approved for use in the United Kingdom.
Saxenda belongs to a class of medications called GLP-1 receptor agonists. It works by mimicking the action of glucagon-like peptide-1, a naturally occurring hormone that regulates appetite and food intake. Liraglutide acts on areas of the brain involved in appetite regulation, promoting feelings of fullness (satiety) and reducing hunger. It also slows gastric emptying, which contributes to prolonged satiety after meals. Saxenda is administered as a once-daily subcutaneous injection and is indicated for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater in the presence of at least one weight-related comorbidity such as type 2 diabetes, hypertension, or dyslipidaemia. Treatment should be discontinued if patients have not lost at least 5% of their initial body weight after 12 weeks on the full 3.0 mg daily dose.
Qsymia combines two active pharmaceutical ingredients with distinct mechanisms. Phentermine is a sympathomimetic amine that suppresses appetite through effects on the central nervous system, whilst topiramate—originally developed as an antiepileptic—contributes to weight loss through multiple pathways including appetite suppression and increased satiety. The extended-release formulation is designed to provide sustained drug levels throughout the day. In the United States, Qsymia is approved for chronic weight management in adults with similar BMI criteria to Saxenda. However, UK patients do not have access to Qsymia through standard NHS or private prescription channels, as it has not received MHRA authorisation.
Can Saxenda and Qsymia Be Taken Together? Current Evidence and Regulatory Position
There is no official approval or clinical guidance supporting the concurrent use of Saxenda and Qsymia for weight management. Neither the MHRA, NICE, nor the US Food and Drug Administration (FDA) has evaluated or endorsed combining these medications. The prescribing information for both drugs does not include data on their combined use, and no large-scale clinical trials have systematically assessed the safety, efficacy, or pharmacological interactions of this combination.
The absence of regulatory approval reflects several important considerations. Firstly, clinical trials for weight loss medications typically evaluate single agents against placebo or lifestyle interventions, not combinations of prescription drugs. Secondly, combining medications with overlapping mechanisms or side effect profiles may increase the risk of adverse events without proportional therapeutic benefit. Thirdly, the regulatory framework requires robust evidence of safety and efficacy before approving any medication regimen, and such evidence does not currently exist for Saxenda and Qsymia used together.
From a UK perspective, the question of combining these medications is largely theoretical, as Qsymia is not authorised by the MHRA and cannot be routinely prescribed in the UK. Patients who obtain Qsymia through international online pharmacies or medical tourism face additional risks, including lack of quality assurance, absence of appropriate medical supervision, and potential legal implications. The MHRA actively warns against purchasing prescription medications from unregulated sources due to significant safety concerns.
Healthcare professionals in the UK follow NICE guidance on obesity management, which recommends pharmacotherapy as an adjunct to lifestyle interventions in appropriate patients. Current NICE-recommended options include orlistat (as per CG189), semaglutide 2.4 mg (Wegovy) for patients meeting specific criteria, and liraglutide 3.0 mg (Saxenda) for a restricted subgroup within specialist services. While naltrexone/bupropion (Mysimba) is licensed in the UK, it is not currently recommended by NICE. Any off-label or combination use would require careful consideration of the risk-benefit profile, informed consent, and close monitoring—circumstances that are difficult to achieve when one agent lacks UK regulatory approval.
Potential Risks and Drug Interactions of Combining Weight Loss Medications
Combining Saxenda and Qsymia would theoretically expose patients to the cumulative adverse effect profiles of both medications, potentially increasing the frequency and severity of side effects. Common adverse effects of Saxenda include nausea, vomiting, diarrhoea, constipation, and abdominal pain, particularly during dose titration. More serious but less common risks include pancreatitis, gallbladder disease, and increased heart rate. The Saxenda SmPC notes that thyroid C-cell tumours have been observed in rodent studies, though the relevance to humans remains uncertain.
Qsymia's side effect profile reflects its dual-component formulation. Phentermine, as a sympathomimetic agent, can cause increased heart rate, elevated blood pressure, insomnia, dry mouth, and nervousness. It has potential for dependence and is classified as a controlled substance in the United States. Topiramate is associated with cognitive effects (difficulty concentrating, memory problems), paraesthesia (tingling sensations), taste alterations, and metabolic acidosis. Topiramate also carries significant teratogenic risk and is contraindicated in pregnancy, requiring reliable contraception in women of childbearing potential. Other important topiramate risks include acute myopia with secondary angle-closure glaucoma (presenting as sudden vision changes or eye pain) and nephrolithiasis (kidney stones).
Cardiovascular considerations are particularly important when contemplating combination therapy. Both medications can affect heart rate and cardiovascular parameters. Saxenda may increase resting heart rate by 2–3 beats per minute on average, whilst phentermine's sympathomimetic effects can elevate both heart rate and blood pressure. Patients with pre-existing cardiovascular disease, uncontrolled hypertension, or arrhythmias would face compounded risks.
Drug interactions must also be considered. Topiramate can interact with carbonic anhydrase inhibitors and other medications affecting acid-base balance. While topiramate at higher doses (≥200 mg/day) can reduce oral contraceptive efficacy, at the doses used in Qsymia this effect is less pronounced, though irregular bleeding can occur. Phentermine should not be combined with monoamine oxidase inhibitors (MAOIs) or used within 14 days of MAOI discontinuation. Saxenda generally has no clinically relevant effect on the exposure of oral medications, though it may delay absorption. Monitoring is advised when initiating liraglutide with warfarin or other narrow therapeutic index drugs. Both medications are contraindicated in pregnancy; effective contraception is essential, and treatment should be stopped immediately if pregnancy occurs.
Alternative Approaches: Sequential Use and Combination Therapy Under Medical Supervision
Rather than combining weight loss medications simultaneously, sequential therapy—using one medication after another—represents a more evidence-based approach when initial treatment proves insufficient. NICE guidance on obesity management emphasises a stepwise approach, beginning with lifestyle interventions (dietary modification, increased physical activity, behavioural strategies) and adding pharmacotherapy when appropriate. If one medication is discontinued due to inadequate response or tolerability issues, switching to an alternative agent with a different mechanism of action may be considered.
For patients who achieve initial weight loss with one medication but subsequently plateau, reassessment of the overall treatment plan is more appropriate than adding a second weight loss drug. This reassessment should include evaluation of adherence to lifestyle modifications, identification of potential barriers to continued weight loss, screening for medical conditions that may impede weight management (such as hypothyroidism or medication-induced weight gain), and consideration of whether the current pharmacotherapy remains optimal.
Combination approaches in obesity medicine do exist within evidence-based frameworks, but these involve specifically studied and approved combinations. For example, naltrexone/bupropion (Mysimba in the UK) is a fixed-dose combination product that has undergone clinical trials evaluating its safety and efficacy as a combined formulation. This differs fundamentally from combining two separately approved medications without supporting clinical trial data.
In specialist obesity services, multidisciplinary management may incorporate various therapeutic modalities under close supervision. This might include pharmacotherapy alongside psychological support, dietetic input, exercise prescription, and in appropriate cases, consideration of bariatric surgery. Such comprehensive programmes are delivered by healthcare professionals with expertise in obesity medicine and include regular monitoring of efficacy, safety parameters, and overall health status.
Patients considering any form of combination or intensive pharmacotherapy should be managed within appropriate clinical frameworks. In the UK, this typically means referral to specialist weight management services (tier 3) for individuals with BMI ≥40 kg/m² or ≥35 kg/m² with significant comorbidities, particularly for those who have not responded adequately to standard interventions. Specialist services can provide the intensive monitoring and individualised treatment planning necessary for more complex cases, and can assess eligibility for treatments with specific NICE criteria, such as semaglutide 2.4 mg (Wegovy) or liraglutide 3.0 mg (Saxenda).
When to Seek Medical Advice: Safe Weight Management Strategies
Patients should consult their GP or healthcare provider before starting, stopping, or combining any weight loss medications. This is particularly important given that Qsymia is not approved in the UK, and obtaining it through unregulated channels poses significant safety risks. Healthcare professionals can provide evidence-based guidance on appropriate weight management strategies, assess suitability for pharmacotherapy, and ensure proper monitoring of treatment.
Immediate medical attention should be sought if any of the following occur whilst taking weight loss medications:
-
Severe abdominal pain, particularly if persistent and radiating to the back, which may indicate pancreatitis
-
Chest pain, palpitations, or shortness of breath, suggesting potential cardiovascular effects
-
Mood changes, depression, or suicidal thoughts, as some weight loss medications can affect mental health
-
Sudden vision changes or eye pain, which may indicate acute myopia with secondary angle-closure glaucoma (a serious effect of topiramate)
-
Signs of allergic reaction, including rash, swelling, or difficulty breathing
-
Symptoms of gallbladder disease, such as right upper quadrant pain, particularly after eating
-
Flank pain with or without blood in urine, which could indicate kidney stones (associated with topiramate)
Regular monitoring is essential for anyone taking prescription weight loss medications. This typically includes periodic assessment of weight loss progress, blood pressure, heart rate, and relevant blood tests. For patients with diabetes taking Saxenda alongside insulin or sulfonylureas, monitoring for hypoglycaemia is important, and dose adjustments of diabetes medications may be needed. The frequency of monitoring should be determined by the prescribing clinician based on individual patient factors.
Evidence-based weight management in the UK follows NICE guidelines, which emphasise that pharmacotherapy should always be used as an adjunct to, not a replacement for, lifestyle modifications. Sustainable weight loss requires a comprehensive approach incorporating:
-
Dietary changes focusing on energy deficit, balanced nutrition, and sustainable eating patterns
-
Increased physical activity tailored to individual capabilities and preferences
-
Behavioural strategies to address eating behaviours, emotional eating, and lifestyle factors
-
Regular follow-up to monitor progress, adjust treatment plans, and provide ongoing support
Patients should be wary of claims suggesting that combining multiple weight loss medications will produce superior results without increased risks. Safe, effective weight management requires individualised treatment plans developed in partnership with qualified healthcare professionals, realistic goal-setting, and commitment to long-term lifestyle changes. Any suspected adverse reactions to medications should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app). For those struggling with obesity despite lifestyle interventions, discussing evidence-based pharmacotherapy options with a GP or referral to specialist weight management services represents the most appropriate pathway to safe and effective treatment.
Frequently Asked Questions
Is Qsymia available in the UK?
No, Qsymia is not approved by the MHRA or EMA and cannot be legally prescribed in the UK. It was refused European authorisation and is only licensed in the United States.
What are the risks of combining weight loss medications?
Combining medications may increase adverse effects including cardiovascular complications, gastrointestinal symptoms, metabolic disturbances, and drug interactions. Without clinical trial data, the safety profile of such combinations remains unknown.
What should I do if one weight loss medication stops working?
Consult your GP or specialist to reassess your treatment plan, review lifestyle modifications, and consider switching to an alternative medication with a different mechanism of action rather than combining drugs.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript