Experiencing a weight loss plateau whilst taking Saxenda (liraglutide 3.0 mg) is a common challenge that many patients face during their weight management journey. Saxenda, a GLP-1 receptor agonist licensed by the MHRA, works by regulating appetite and food intake, but weight loss typically slows after the initial months of treatment. Understanding how to jump-start Saxenda after a plateau requires a systematic approach that addresses metabolic adaptation, dietary adherence, and lifestyle factors. This article explores evidence-based strategies to overcome plateaus, when to seek medical review, and how to optimise treatment effectiveness in line with NHS and NICE guidance.
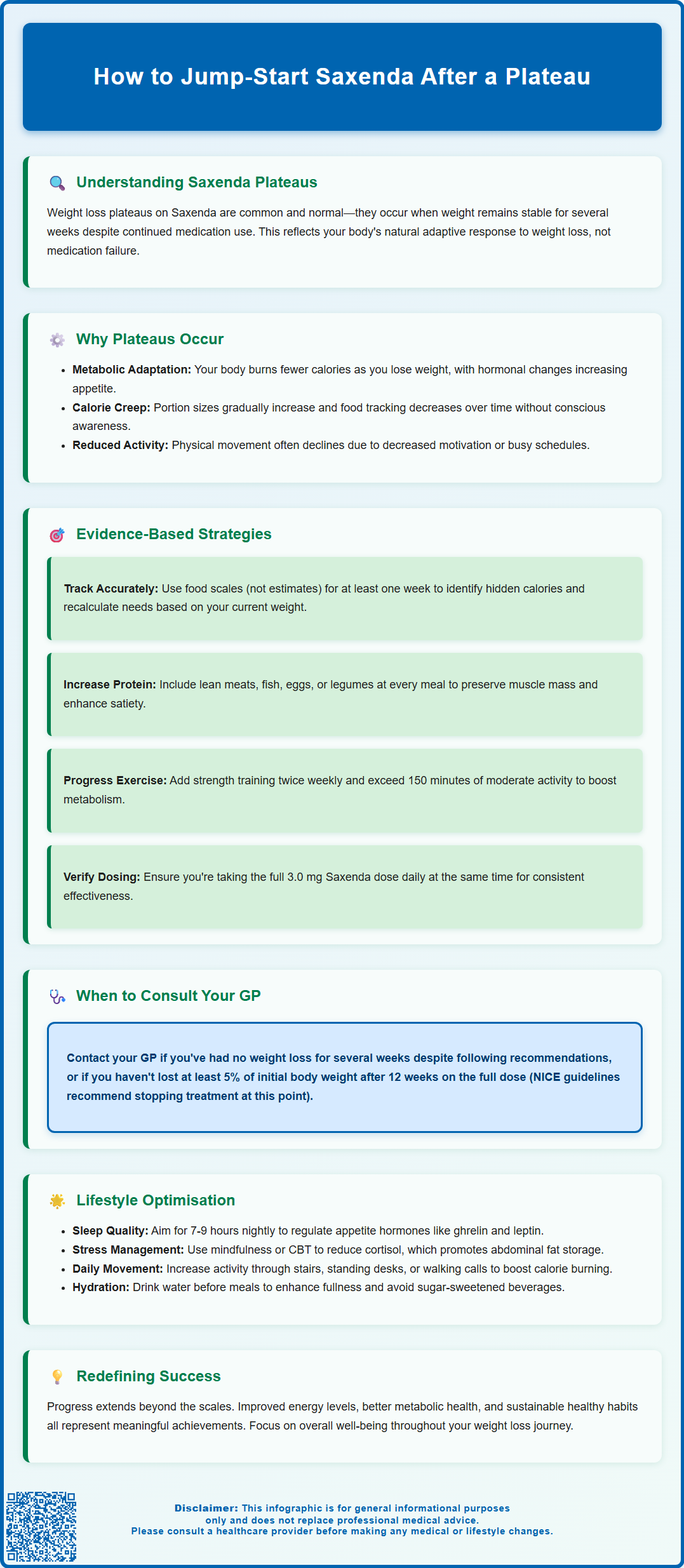
Summary: To jump-start Saxenda after a plateau, reassess caloric intake with accurate food tracking, increase physical activity beyond current levels, ensure consistent medication administration at the full 3.0 mg dose, and address lifestyle factors including sleep quality and stress management.
- Saxenda is a GLP-1 receptor agonist licensed for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with comorbidities
- Plateaus occur due to metabolic adaptation, reduced energy expenditure, dietary adherence decline, and hormonal changes during weight loss
- Treatment should be discontinued after 12 weeks on 3.0 mg if less than 5% initial body weight has been lost, per NICE guidance
- Accurate calorie tracking, increased protein intake, and progressive physical activity are evidence-based strategies to overcome plateaus
- Seek urgent medical attention for severe abdominal pain, gallbladder symptoms, or persistent vomiting which may indicate serious complications
Table of Contents
Understanding Weight Loss Plateaus on Saxenda
A weight loss plateau whilst taking Saxenda (liraglutide 3.0 mg) is a common and often frustrating experience. Saxenda is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with weight-related comorbidities. The medication works by mimicking the natural hormone GLP-1, which regulates appetite and food intake by acting on areas of the brain that control hunger.
A plateau is commonly considered to be a period of several weeks during which weight remains stable despite continued adherence to treatment and lifestyle modifications. Clinical data from the SCALE trials suggest that early response to Saxenda often predicts longer-term outcomes, with the rate of weight loss typically slowing after the initial months of treatment. This slowing is not necessarily a sign that the medication has stopped working entirely, but rather reflects the body's natural adaptive responses to weight loss.
Characteristics that may indicate a plateau include:
-
No significant weight change for several consecutive weeks
-
Continued adherence to prescribed Saxenda dosing
-
Maintenance of dietary and physical activity recommendations
-
Absence of new medications or medical conditions affecting weight
It is important to distinguish between a true plateau and normal weight fluctuations, which can occur due to fluid retention, hormonal changes, or variations in dietary sodium intake. Understanding that plateaus are a normal part of the weight loss journey can help maintain realistic expectations.
In the NHS, Saxenda is typically initiated and monitored within specialist weight management services in accordance with NICE Technology Appraisal 664. The Saxenda SmPC specifies that treatment should be discontinued after 12 weeks on the full 3.0 mg dose if at least 5% of initial body weight has not been lost (a lower threshold applies for people with type 2 diabetes).
Why Saxenda May Stop Working After Initial Success
Several physiological and behavioural factors contribute to reduced weight loss efficacy over time with Saxenda. Understanding these mechanisms can help identify appropriate strategies to overcome plateaus.
Metabolic adaptation is perhaps the most significant factor. As body weight decreases, total energy expenditure naturally declines because a smaller body requires fewer calories for basic metabolic functions and physical activity. Research shows that resting metabolic rate can decrease during significant weight loss, though the magnitude varies between individuals. Additionally, hormonal changes occur during weight loss, including reductions in leptin (which signals satiety) and increases in ghrelin (which stimulates appetite), creating a biological drive to regain lost weight.
Dietary adherence often diminishes over time, even unconsciously. Portion sizes may gradually increase, or higher-calorie foods may be reintroduced more frequently. Self-monitoring of food intake typically decreases after the initial months of treatment, leading to "calorie creep" where energy intake slowly rises without conscious awareness.
Pharmacological tolerance is sometimes discussed, though there is no official link established between long-term Saxenda use and true receptor desensitisation. The medication continues to exert its pharmacological effects on GLP-1 receptors, but the relative impact on appetite suppression may feel less pronounced as initial side effects (such as nausea) diminish and eating patterns normalise.
Physical activity levels may also decline over time due to increased confidence, busy schedules, or reduced motivation once initial weight loss goals are partially achieved. This reduction in energy expenditure can significantly impact the overall calorie deficit needed for continued weight loss.
It's worth noting that if you miss more than 3 consecutive days of Saxenda injections, the SmPC recommends restarting at 0.6 mg and following the dose escalation schedule again to minimise gastrointestinal side effects.
Evidence-Based Strategies to Restart Weight Loss on Saxenda
Breaking through a Saxenda plateau requires a systematic, evidence-based approach that addresses both physiological and behavioural factors.
Reassess caloric intake accurately. The most effective first step is to conduct a thorough dietary review. Utilise a food diary or smartphone application to track all food and beverages for at least one week, measuring portions with kitchen scales rather than estimating. Research indicates that many people unintentionally underestimate their calorie intake when attempting to lose weight. Calculate your current energy needs based on your new, lower body weight, and aim for about a 600 kcal per day deficit in line with NICE guidance, or consider an evidence-based low-energy diet with appropriate support.
Consider protein intake. Adequate protein intake can help preserve lean muscle mass during weight loss and increase satiety. Focus on including protein-rich foods at each meal, such as lean meats, fish, eggs, legumes, and low-fat dairy products. If considering higher protein intakes, discuss with a healthcare professional, particularly if you have kidney disease or other conditions that may require dietary protein modification.
Review physical activity. If you have maintained the same exercise routine throughout your Saxenda treatment, your body has likely adapted to this level of activity. UK Chief Medical Officers' guidelines recommend at least 150 minutes of moderate-intensity aerobic activity weekly plus strength exercises on at least 2 days per week. Increasing activity beyond these minimums may provide additional benefits for weight management. Consider incorporating resistance training to build or maintain muscle mass, which supports metabolic rate.
Review medication administration. Ensure you are administering Saxenda at the same time each day and have reached the full maintenance dose of 3.0 mg daily (unless limited by tolerability). The SmPC does not indicate that the timing of injection relative to meals affects the medication's efficacy, but consistency in administration is important for optimal results.
When to Speak with Your GP About Your Saxenda Plateau
Whilst plateaus are common, certain circumstances warrant medical review to ensure safe and effective ongoing treatment.
Schedule a GP appointment if:
-
You have experienced no weight loss for several weeks despite documented adherence to dietary, activity, and medication recommendations
-
You have developed new or worsening side effects
-
You have concerns about continuing treatment
-
You have developed new symptoms or medical conditions that may affect weight
Seek urgent medical attention if you experience:
-
Severe, persistent abdominal pain (with or without vomiting) which could indicate pancreatitis
-
Symptoms of gallbladder disease such as pain in the upper right abdomen, fever, or yellowing of the skin/eyes
-
Significant dehydration from persistent vomiting or diarrhoea
Your GP can conduct a comprehensive medication review to identify any newly prescribed drugs that may contribute to weight gain or plateau, such as certain antidepressants, antipsychotics, corticosteroids, or diabetes medications. They can also assess for medical conditions that affect metabolism, including hypothyroidism, polycystic ovary syndrome (PCOS), or Cushing's syndrome, though these are relatively uncommon causes of treatment-resistant weight plateaus.
According to the Saxenda SmPC and NICE Technology Appraisal 664, treatment should be discontinued if at least 5% of initial body weight has not been lost after 12 weeks on the full 3.0 mg daily dose (a lower threshold applies for people with type 2 diabetes). In the NHS, Saxenda is typically initiated and monitored within specialist weight management services rather than primary care.
Your healthcare provider may refer you to specialist weight management services, which can provide multidisciplinary support including dietetic input, psychological interventions for eating behaviours, and structured physical activity programmes. Some individuals may be candidates for alternative pharmacological treatments or, in specific circumstances, bariatric surgery referral if BMI and comorbidity criteria are met.
If you experience any suspected side effects from Saxenda, report them via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Lifestyle Adjustments That Support Saxenda Effectiveness
Sustainable lifestyle modifications are essential for maximising Saxenda's effectiveness and maintaining long-term weight management success.
Implement structured eating patterns. Rather than grazing throughout the day, establish regular meal times with defined eating windows. Some individuals find that time-restricted eating (consuming all calories within a limited daily window) helps with adherence, though evidence for its superiority over standard calorie restriction is mixed. This approach may not be suitable for everyone, particularly those with diabetes on hypoglycaemia-inducing medications, history of eating disorders, or during pregnancy or breastfeeding. Focus on whole, minimally processed foods with high nutrient density and satiety value, including vegetables, fruits, whole grains, lean proteins, and healthy fats.
Address sleep quality and duration. Poor sleep is strongly associated with weight gain and difficulty losing weight. Aim for 7–9 hours of quality sleep nightly. Sleep deprivation disrupts hormones that regulate appetite (increasing ghrelin and decreasing leptin) and impairs glucose metabolism. Establish a consistent sleep schedule, create a dark and cool sleeping environment, and limit screen time before bed.
Manage stress effectively. Chronic psychological stress elevates cortisol levels, which can promote abdominal fat storage and increase cravings for high-calorie comfort foods. Incorporate stress-reduction techniques such as mindfulness meditation, yoga, deep breathing exercises, or regular physical activity. Consider cognitive behavioural therapy (CBT) if emotional eating or stress-related eating patterns are significant barriers.
Increase non-exercise activity thermogenesis (NEAT). Small increases in daily movement—such as taking stairs, parking further away, standing whilst working, or walking during phone calls—can cumulatively increase energy expenditure throughout the day without requiring structured exercise sessions.
Stay adequately hydrated. Drinking water before meals can enhance satiety and reduce calorie intake. The NHS recommends 6-8 cups or glasses of fluid daily, with water being the healthiest choice. Avoid sugar-sweetened beverages and limit alcohol consumption, as alcoholic drinks provide calories without nutritional value and can impair judgement regarding food choices.
Frequently Asked Questions
How long does a Saxenda plateau typically last?
A plateau is commonly defined as several consecutive weeks without significant weight change despite continued adherence to treatment and lifestyle modifications. The duration varies between individuals, but if no weight loss occurs after 12 weeks on the full 3.0 mg dose and less than 5% initial body weight has been lost, NICE guidance recommends discontinuing treatment.
Can I increase my Saxenda dose beyond 3.0 mg to break a plateau?
No, the maximum licensed dose of Saxenda is 3.0 mg daily. Increasing beyond this dose is not recommended and is not supported by clinical evidence or regulatory approval from the MHRA.
Should I stop and restart Saxenda to overcome a plateau?
Stopping and restarting Saxenda is not an evidence-based strategy for overcoming plateaus. If you miss more than 3 consecutive days, you must restart at 0.6 mg and follow the dose escalation schedule again. Discuss any concerns about treatment effectiveness with your GP or specialist weight management service.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










