Mounjaro (tirzepatide) is not recommended for use during breastfeeding. As a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus, Mounjaro has demonstrated significant efficacy in glycaemic control. However, it remains unknown whether tirzepatide is excreted in human breast milk, and a risk to newborns and infants cannot be excluded according to the MHRA Summary of Product Characteristics. Clinical trials have not included breastfeeding women, meaning potential risks to nursing infants are undetermined. This article examines the evidence surrounding Mounjaro and breastfeeding, explores alternative diabetes treatments compatible with nursing, and provides guidance on when to discuss treatment options with your healthcare provider.
Summary: Mounjaro (tirzepatide) should not be used during breastfeeding as it is unknown whether the medication passes into human milk and potential risks to nursing infants cannot be excluded.
- Tirzepatide is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus treatment.
- Clinical trials have not included breastfeeding women, leaving the safety profile in nursing mothers undetermined.
- Metformin and insulin are preferred diabetes treatment options during breastfeeding with established safety profiles.
- Women of childbearing potential using Mounjaro should use effective contraception, with additional barrier methods needed for 4 weeks after initiation and dose escalations.
- Tirzepatide should be discontinued at least 1 month before a planned pregnancy according to MHRA guidance.
- Healthcare providers can recommend breastfeeding-compatible alternatives that maintain glycaemic control whilst protecting infant safety.
Table of Contents
Can You Take Mounjaro While Breastfeeding?
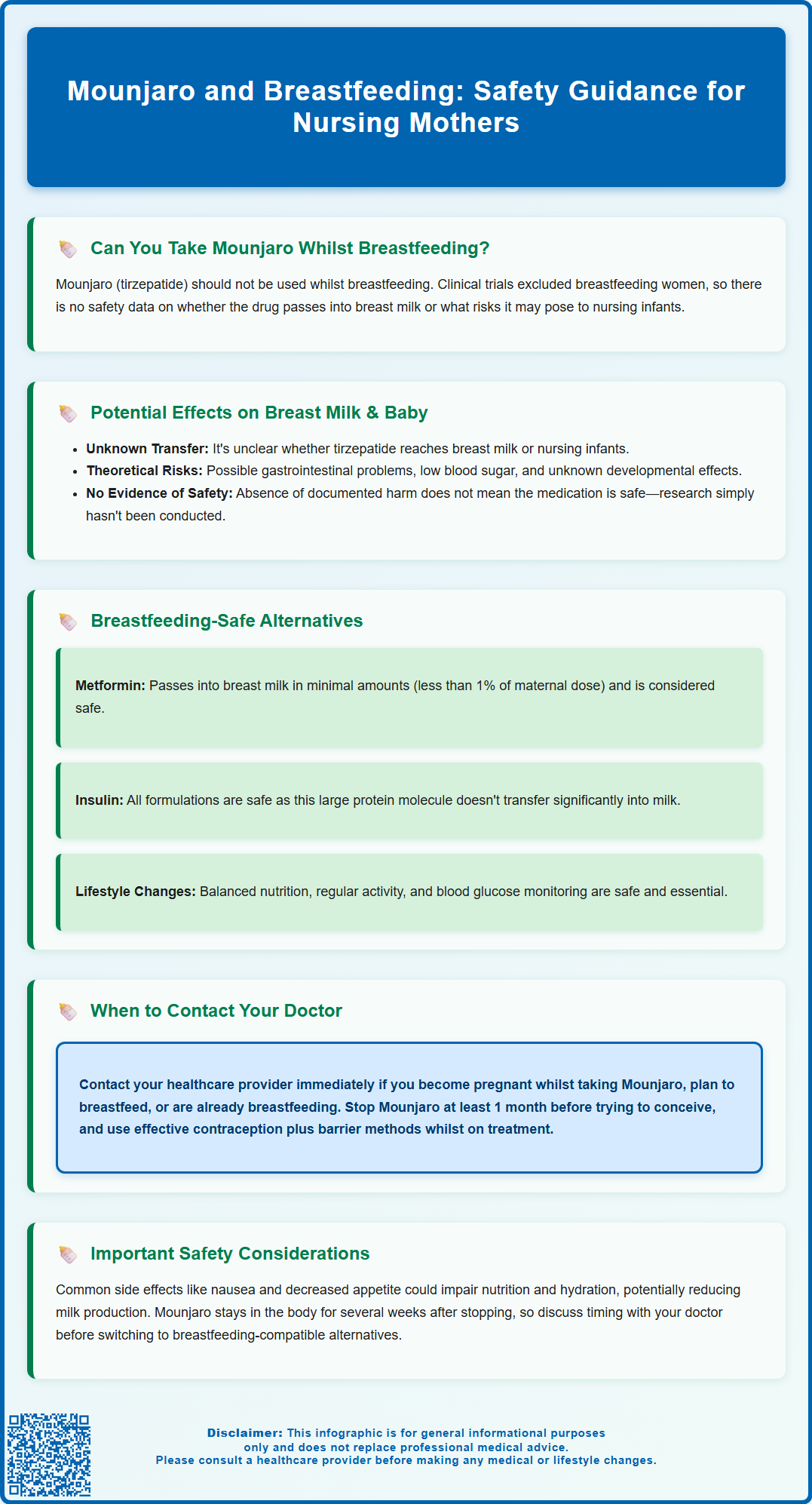
Mounjaro (tirzepatide) should not be used during breastfeeding. According to the MHRA Summary of Product Characteristics (SmPC), it is unknown whether tirzepatide is excreted in human milk, and a risk to newborns/infants cannot be excluded.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, licensed in the UK for the treatment of type 2 diabetes mellitus. Whilst the medication has demonstrated significant efficacy in glycaemic control and weight management, clinical trials have not included breastfeeding women, meaning the potential risks to nursing infants remain unknown.
The primary concern centres on whether tirzepatide passes into breast milk and, if so, in what concentrations. As a large peptide molecule (molecular weight approximately 4,813 Da), tirzepatide's transfer into breast milk is theoretically limited; however, without robust human data, healthcare professionals cannot confirm this assumption. Animal studies provide limited reassurance, as they do not always predict human outcomes accurately.
If you are currently breastfeeding or planning to breastfeed, you should not use Mounjaro. The decision to use any medication during lactation requires careful consideration of the benefits to the mother against potential risks to the infant. In most cases, alternative diabetes management strategies that are better studied in breastfeeding populations will be recommended. Your healthcare team can help you navigate these options whilst ensuring both your health and your baby's wellbeing remain protected.
How Mounjaro May Affect Breast Milk and Your Baby
The transfer of tirzepatide into human breast milk has not been adequately studied, making it impossible to definitively state whether the medication reaches nursing infants or what effects it might have. As stated in the MHRA SmPC: "It is unknown whether tirzepatide is excreted in human milk. A risk to newborns/infants cannot be excluded."
Tirzepatide's pharmacological properties offer some theoretical insights. As a large peptide molecule administered subcutaneously once weekly, it has a half-life of approximately five days and works systemically to enhance insulin secretion and suppress glucagon release. Tirzepatide also delays gastric emptying, which may affect the absorption of oral medicines. If tirzepatide were to enter breast milk, the acidic environment of an infant's stomach would likely break down the peptide structure, potentially reducing systemic absorption in the baby. However, this remains theoretical, and even minimal exposure during critical developmental periods warrants caution.
Potential theoretical concerns for nursing infants might include:
-
Gastrointestinal effects: Tirzepatide very commonly causes nausea, vomiting, and diarrhoea in adults. If transferred via breast milk, similar effects could theoretically occur in infants, though this has not been documented.
-
Hypoglycaemia: Whilst tirzepatide's glucose-lowering effects are glucose-dependent (reducing the risk of hypoglycaemia), any medication affecting glucose metabolism raises theoretical concerns for infant blood sugar regulation.
-
Growth and development: The long-term effects of GIP/GLP-1 receptor agonist exposure during infancy are completely unknown.
There are no documented adverse infant outcomes from Mounjaro use during breastfeeding, simply because the necessary research has not been conducted. This absence of evidence is not evidence of safety. Consequently, Mounjaro should not be used during breastfeeding.
Alternative Diabetes Treatments During Breastfeeding
Several diabetes management options have established safety profiles during breastfeeding, allowing mothers with type 2 diabetes to maintain glycaemic control whilst nursing. NICE guidance emphasises individualised treatment plans that consider both maternal health needs and infant safety.
Metformin and insulin are preferred options during breastfeeding, with selection individualised based on clinical circumstances. Metformin is generally considered safe during breastfeeding and is often the first-line oral medication for type 2 diabetes in nursing mothers. Studies have shown that metformin passes into breast milk in small quantities (less than 1% of the maternal dose), with no adverse effects reported in breastfed infants. The British National Formulary (BNF) notes that metformin may be used during breastfeeding, though monitoring of the infant is advisable.
Insulin therapy is also compatible with breastfeeding. All insulin formulations (rapid-acting, short-acting, intermediate-acting, and long-acting analogues) are considered safe during breastfeeding, as insulin does not pass into breast milk in clinically significant amounts. Insulin is a large protein molecule that, even if present in milk, would be digested in the infant's gastrointestinal tract.
Glibenclamide (known as glyburide in the US) has limited data suggesting low milk transfer, whilst other sulphonylureas and newer agents generally lack sufficient evidence.
SGLT2 inhibitors should be avoided during breastfeeding due to potential risks to infant renal development.
Lifestyle modifications form the cornerstone of diabetes management and are entirely compatible with breastfeeding. These include:
-
Balanced nutrition with regular meal timing
-
Regular physical activity appropriate for the postpartum period
-
Weight management through sustainable dietary changes
-
Blood glucose monitoring to guide treatment adjustments
Your diabetes specialist can review your specific circumstances and recommend the most appropriate regimen that balances effective glycaemic control with infant safety.
When to Discuss Mounjaro with Your Healthcare Provider
You should contact your GP or diabetes specialist before starting, stopping, or continuing Mounjaro in several specific circumstances related to breastfeeding and family planning. Open communication with your healthcare team ensures safe, evidence-based decision-making.
Contact your healthcare provider immediately if:
-
You discover you are pregnant whilst taking Mounjaro, as the medication is not recommended during pregnancy and alternative treatments should be arranged promptly
-
You are currently taking Mounjaro and wish to start breastfeeding
-
You are breastfeeding and have been prescribed Mounjaro
-
You are planning pregnancy in the near future and are currently using Mounjaro
Schedule a routine appointment to discuss Mounjaro if:
-
You are considering starting diabetes treatment and are currently breastfeeding or planning to breastfeed within the next year
-
Your current diabetes medications are not achieving adequate glycaemic control and you are nursing
-
You are approaching the end of breastfeeding and wish to explore whether Mounjaro might be appropriate for your diabetes management
-
You have questions about how long to wait after stopping breastfeeding before starting Mounjaro
The MHRA recommends that women of childbearing potential should use effective contraception during Mounjaro treatment. Importantly, tirzepatide reduces the exposure of oral hormonal contraceptives; additional barrier contraception is needed for 4 weeks after initiation and after each dose escalation. The SmPC also advises to discontinue tirzepatide at least 1 month before a planned pregnancy.
Your diabetes review should include discussion of:
-
Your current glycaemic control and HbA1c levels
-
Alternative medications compatible with breastfeeding
-
Your breastfeeding plans and timeline
-
The risks and benefits of different treatment options
-
Monitoring requirements for both you and your baby
Your healthcare team can provide personalised advice based on your individual circumstances, diabetes history, and family planning intentions. Never discontinue prescribed diabetes medications without medical guidance, as uncontrolled blood glucose poses significant health risks.
Safety Considerations for Nursing Mothers Taking Mounjaro
The current medical consensus is that Mounjaro should not be used during breastfeeding due to the absence of safety data. However, understanding the broader safety considerations helps nursing mothers make informed decisions about their diabetes management.
If Mounjaro use during breastfeeding were to be considered in exceptional circumstances, several safety factors would require careful evaluation:
Maternal considerations:
-
Gastrointestinal adverse effects: Nausea, vomiting, diarrhoea, and decreased appetite are very common with tirzepatide. These effects could impact a nursing mother's nutritional status and ability to maintain adequate hydration, potentially affecting milk production.
-
Hypoglycaemia risk: Whilst tirzepatide alone carries low hypoglycaemia risk, combination with other diabetes medications (particularly insulin or sulphonylureas) increases this risk. Hypoglycaemic episodes could impair a mother's ability to safely care for her infant.
-
Nutritional requirements: Breastfeeding increases energy needs. The NHS recommends a balanced, nutritious diet and adequate hydration to support milk production. Tirzepatide's appetite-suppressing effects might make meeting these increased nutritional needs challenging.
Infant monitoring considerations:
Should a mother take Mounjaro whilst breastfeeding (against current guidance), the infant would require close monitoring for:
-
Feeding patterns and weight gain
-
Gastrointestinal symptoms (unusual fussiness, vomiting, diarrhoea)
-
General wellbeing and developmental milestones
Timing and drug washout:
Given tirzepatide's five-day half-life and weekly dosing schedule, the medication remains in the system for several weeks after the last dose. Substantial elimination typically occurs within 4-5 half-lives. If transitioning from Mounjaro to breastfeeding-compatible alternatives, discuss appropriate timing with your healthcare provider. The SmPC specifies discontinuing tirzepatide at least 1 month before a planned pregnancy, though no specific breastfeeding washout period is defined.
The principle of informed decision-making requires that nursing mothers receive complete information about both the known risks of uncontrolled diabetes and the unknown risks of medication exposure through breast milk. Your healthcare team should support you in achieving optimal diabetes control through evidence-based, breastfeeding-compatible treatments, ensuring both your health and your baby's safety remain the priority.
If you experience any suspected side effects from diabetes medications, report them to the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk.
Frequently Asked Questions
Can I take Mounjaro whilst breastfeeding?
No, Mounjaro (tirzepatide) should not be used during breastfeeding. It is unknown whether tirzepatide passes into human breast milk, and potential risks to nursing infants cannot be excluded according to MHRA guidance.
What diabetes medications are safe during breastfeeding?
Metformin and insulin are preferred options during breastfeeding with established safety profiles. Both medications have been studied in nursing mothers and are considered compatible with breastfeeding when used under medical supervision.
How long after stopping Mounjaro can I start breastfeeding?
Tirzepatide has a half-life of approximately five days and remains in the system for several weeks after the last dose. Discuss appropriate timing with your healthcare provider, who can advise on transitioning to breastfeeding-compatible diabetes treatments.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript