Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, not as an energy booster. Many patients wonder whether Ozempic gives you energy or causes fatigue. The medication works by improving blood glucose control and slowing gastric emptying, which can indirectly affect how you feel. Some people report increased energy as their diabetes stabilises and weight decreases, whilst others experience tiredness, particularly during initial treatment. Understanding these effects helps set realistic expectations and guides appropriate management strategies.
Summary: Ozempic does not directly increase energy levels; any changes in energy are indirect consequences of improved blood glucose control, weight loss, or side effects such as nausea and reduced appetite.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK by the MHRA for type 2 diabetes treatment, not as an energy supplement.
- Energy improvements may occur indirectly through better glycaemic control and weight reduction, whilst fatigue often results from gastrointestinal side effects or reduced caloric intake.
- Common side effects including nausea, vomiting, diarrhoea, and reduced appetite can significantly impact energy levels, particularly during dose escalation.
- Hypoglycaemia risk increases when Ozempic is combined with sulphonylureas or insulin, requiring careful monitoring and dose adjustment of concomitant medications.
- Seek urgent medical advice for severe persistent fatigue, recurrent hypoglycaemia, dehydration signs, or severe abdominal pain whilst taking Ozempic.
Table of Contents
Does Ozempic Give You Energy or Make You Tired?
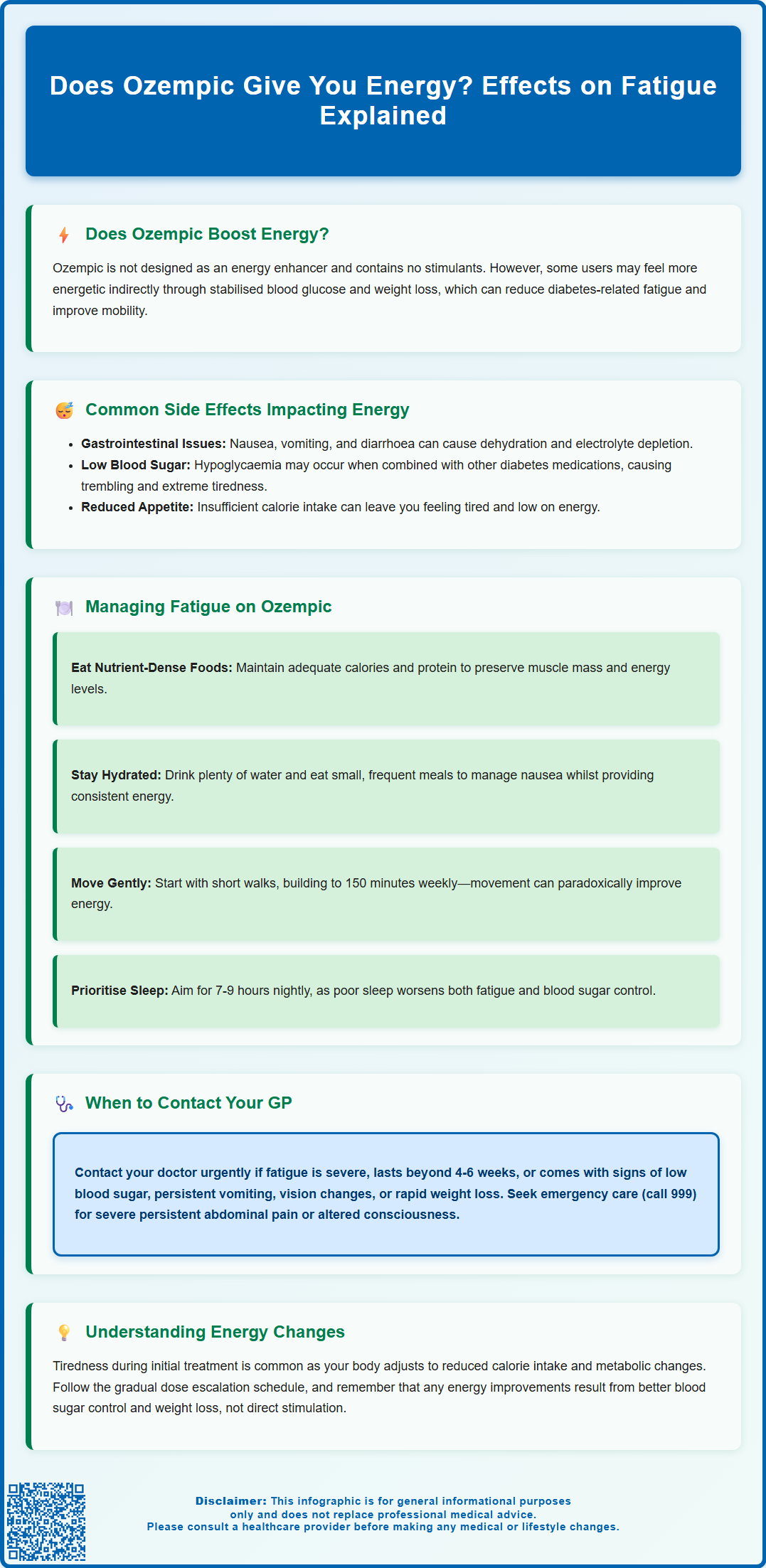
Ozempic (semaglutide) is not designed to increase energy levels, and there is no official evidence that it acts as an energy booster. This glucagon-like peptide-1 (GLP-1) receptor agonist is licensed in the UK by the MHRA for the treatment of type 2 diabetes mellitus (not for weight management, for which Wegovy is the licensed semaglutide product). Ozempic works primarily by enhancing insulin secretion, suppressing glucagon release, and slowing gastric emptying. Its primary therapeutic goal is improved glycaemic control, with weight reduction occurring as a beneficial effect.
Individual experiences with energy levels whilst taking Ozempic vary considerably. Some people may feel more energetic as their blood glucose stabilises and excess weight decreases, both of which can indirectly improve overall wellbeing and physical capacity. Better diabetes control can reduce the fatigue associated with hyperglycaemia, whilst weight loss may enhance mobility and reduce strain on joints and the cardiovascular system.
Conversely, many patients may experience tiredness, particularly during the initial weeks of treatment. This is not listed as a common direct adverse effect in the UK SmPC but may result from several factors: the medication's effect on appetite and reduced caloric intake, gastrointestinal side effects such as nausea, or the body's adjustment to improved metabolic control. Additionally, weight loss can temporarily affect energy levels as the body adapts to lower caloric intake.
It is important to note that patients with pre-existing diabetic retinopathy should be monitored closely, as rapid improvement in blood glucose control may temporarily worsen retinopathy. Patients with this condition should inform their eye care team when starting Ozempic.
Ozempic does not contain stimulants and does not directly influence energy metabolism in the way that, for example, thyroid hormones do. Any changes in energy levels are typically indirect consequences of the medication's effects on glucose regulation, appetite, body weight, and gastrointestinal function.
Common Side Effects That May Impact Your Energy
Several common adverse effects of Ozempic can significantly influence how energetic or fatigued you feel during treatment. Understanding these side effects helps distinguish between expected medication responses and symptoms requiring medical attention.
Gastrointestinal disturbances are the most frequently reported side effects and can substantially impact energy levels:
-
Nausea and vomiting – Very common side effects (may affect more than 1 in 10 people), particularly during dose escalation, these symptoms can reduce nutritional intake and lead to dehydration, both contributing to fatigue
-
Diarrhoea – A common side effect that can cause fluid and electrolyte losses, resulting in weakness and tiredness
-
Reduced appetite – Whilst therapeutically beneficial for weight management, significantly decreased food intake may result in insufficient caloric energy
-
Abdominal discomfort and constipation – Persistent digestive upset can disrupt sleep quality and daily functioning
Hypoglycaemia (low blood sugar) represents another important consideration, especially when Ozempic is used alongside other glucose-lowering medications such as sulphonylureas or insulin. Symptoms of hypoglycaemia include trembling, sweating, confusion, and profound tiredness. NICE guidance (NG28) recommends careful dose adjustment of concomitant medications to minimise this risk.
Dehydration may occur secondary to gastrointestinal side effects and is a frequently overlooked cause of fatigue. Severe dehydration can lead to acute kidney injury, so monitoring urine output and seeking early medical advice is important if vomiting or diarrhoea is persistent.
Gallbladder problems including gallstones and inflammation of the gallbladder have been reported with GLP-1 receptor agonists and may cause fatigue alongside right upper quadrant pain, fever or jaundice.
Additionally, some patients experience headaches (a common side effect) and dizziness (less common), both of which can contribute to a general sense of unwellness and reduced energy. These effects often improve as the body adjusts to the medication, typically after dose escalation stabilises.
Managing Fatigue While Taking Ozempic
If you experience fatigue whilst taking Ozempic, several evidence-based strategies can help manage this symptom whilst maintaining the therapeutic benefits of treatment.
Nutritional optimisation is paramount:
-
Maintain adequate caloric intake – Despite reduced appetite, ensure you consume sufficient calories to meet your body's energy requirements. Focus on nutrient-dense foods rather than empty calories
-
Consider protein intake – Adequate protein intake helps preserve muscle mass during weight loss and supports energy levels. Discuss appropriate targets with your healthcare provider, especially if you have kidney disease
-
Eat small, frequent meals – This approach can help manage nausea whilst ensuring consistent energy supply throughout the day
-
Stay well hydrated – Aim for adequate fluid intake daily, with the amount individualised based on your health status (particularly important if you have heart failure or kidney disease)
Gradual dose escalation, as recommended in the Summary of Product Characteristics, allows your body to adapt to the medication. The standard titration schedule begins with 0.25mg weekly for four weeks (a starter dose not intended for glycaemic control), increasing to 0.5mg, then potentially to 1mg after at least four weeks. If additional glycaemic control is needed, the dose may be increased to 2mg once weekly after at least 4 weeks on the 1mg dose. Never increase your dose more rapidly than prescribed.
Physical activity, though challenging when fatigued, can paradoxically improve energy levels. Start with gentle exercise such as short walks, gradually increasing duration and intensity as tolerated. The UK Chief Medical Officers' Physical Activity Guidelines recommend that adults aim for at least 150 minutes of moderate-intensity activity weekly, but this should be built up gradually, especially for those with type 2 diabetes.
Sleep hygiene is essential—maintain regular sleep patterns, aiming for 7-9 hours nightly. Poor sleep exacerbates fatigue and can worsen glycaemic control.
Timing of administration is flexible; Ozempic can be administered at any time of day, with or without meals. Some patients find a routine that works best for their individual circumstances, but there is no clinical evidence supporting specific timing to reduce fatigue.
When to Speak to Your GP About Energy Changes
Whilst mild fatigue during the initial weeks of Ozempic treatment is relatively common, certain symptoms warrant prompt medical review. Understanding when to seek professional advice ensures both safety and optimal treatment outcomes.
Contact your GP or diabetes specialist nurse urgently if you experience:
-
Severe or persistent fatigue that significantly impairs daily functioning or does not improve after 4-6 weeks of stable dosing
-
Signs of hypoglycaemia – particularly if recurrent, including trembling, confusion, sweating, or extreme tiredness (blood glucose consistently below 4mmol/L)
-
Symptoms of dehydration – reduced urination, dark urine, dizziness upon standing, dry mouth, or persistent thirst
-
Rapid or unintentional weight loss persisting over weeks, which may indicate excessive caloric restriction
-
Persistent nausea or vomiting preventing adequate food or fluid intake for more than 24-48 hours
-
New or worsening visual symptoms – including sudden vision changes, floaters, or blurred vision, especially if you have pre-existing diabetic retinopathy
-
Right upper abdominal pain, fever or yellowing of the skin/eyes – which may indicate gallbladder problems
If you're unsure whether your symptoms require urgent attention, NHS 111 can provide guidance.
Seek immediate medical attention (call 999 or attend A&E) if you develop:
-
Severe, persistent abdominal pain (potential pancreatitis—a rare but serious side effect)
-
Signs of severe dehydration with altered consciousness
-
Symptoms of diabetic ketoacidosis (though rare in type 2 diabetes and more likely if insulin is reduced abruptly or when taking SGLT2 inhibitors)
Your healthcare team can assess whether fatigue relates to Ozempic, underlying diabetes control, other medications, or separate medical conditions such as anaemia, thyroid dysfunction, or vitamin deficiencies—all of which are more common in people with diabetes. They may recommend blood tests including full blood count, thyroid function, renal function (U&Es/eGFR), HbA1c, vitamin B12, and vitamin D levels.
Dose adjustment, additional anti-emetic medication, or switching to an alternative GLP-1 receptor agonist may be appropriate if side effects prove intolerable. Never stop Ozempic abruptly without medical advice, as this may result in deterioration of glycaemic control. Your GP can work with you to develop an individualised management plan that balances diabetes control with quality of life.
Scientific References
Frequently Asked Questions
Can Ozempic make you feel more energetic?
Ozempic does not directly boost energy, but some patients feel more energetic as their blood glucose stabilises and weight decreases. Any energy improvements are indirect consequences of better diabetes control and reduced body weight, not a direct pharmacological effect of the medication.
Why do I feel tired after starting Ozempic?
Fatigue during initial Ozempic treatment commonly results from gastrointestinal side effects such as nausea, reduced appetite leading to lower caloric intake, or the body adjusting to improved metabolic control. These symptoms typically improve after dose escalation stabilises, usually within 4-6 weeks.
When should I contact my GP about fatigue whilst taking Ozempic?
Contact your GP if you experience severe or persistent fatigue impairing daily functioning, recurrent hypoglycaemia, signs of dehydration, persistent vomiting preventing adequate intake, or symptoms lasting beyond 4-6 weeks of stable dosing. Seek immediate medical attention for severe abdominal pain or signs of severe dehydration with altered consciousness.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript