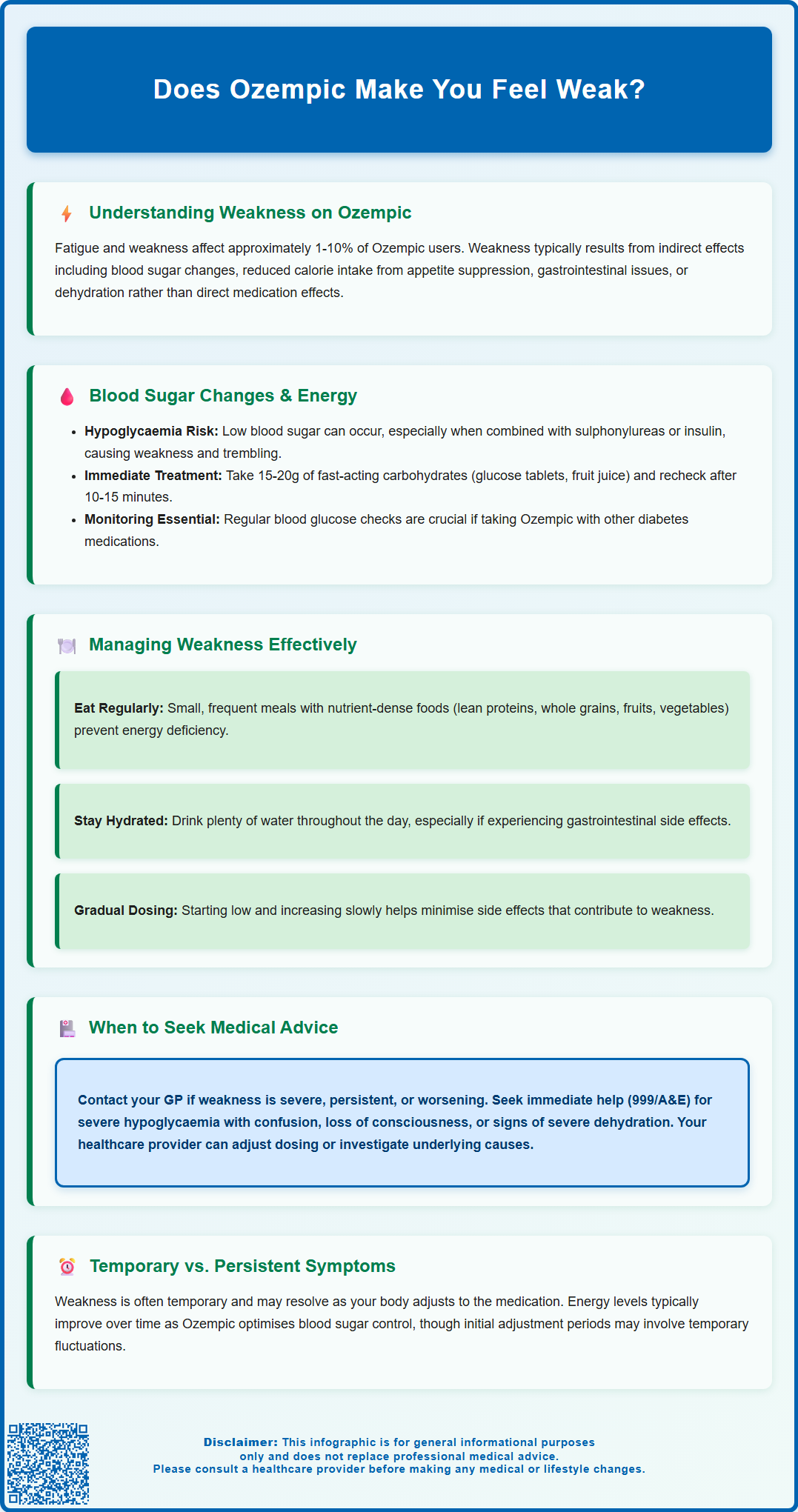
Does Ozempic make you feel weak? Fatigue and weakness affect approximately 1–10% of patients taking Ozempic (semaglutide), a GLP-1 receptor agonist licensed in the UK for type 2 diabetes. Whilst weakness is not a direct pharmacological effect, it may arise indirectly through changes in blood glucose levels, reduced caloric intake from appetite suppression, gastrointestinal side effects such as nausea or vomiting, and dehydration. Most patients find these symptoms transient, resolving as the body adapts to treatment. If you experience persistent or severe weakness whilst taking Ozempic, consult your GP or diabetes specialist nurse for assessment and guidance.
Summary: Ozempic can cause weakness in approximately 1–10% of patients, typically through indirect mechanisms such as blood glucose changes, reduced caloric intake, gastrointestinal side effects, and dehydration rather than direct pharmacological action.
- Semaglutide is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus treatment.
- Weakness may result from hypoglycaemia (especially with sulphonylureas or insulin), appetite suppression leading to insufficient energy intake, or gastrointestinal side effects causing dehydration.
- Gradual dose titration as per the Summary of Product Characteristics helps minimise side effects during the adjustment period.
- Persistent or severe weakness requires medical assessment to exclude hypoglycaemia, dehydration, electrolyte imbalance, or other underlying conditions.
- Report suspected adverse effects through the MHRA Yellow Card Scheme and attend regular follow-up appointments for monitoring.
Table of Contents
Does Ozempic Make You Feel Weak?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Semaglutide is also available at a higher dose as Wegovy, which is licensed specifically for weight management. Fatigue and asthenia (weakness) are listed as adverse reactions in the Ozempic Summary of Product Characteristics (SmPC), with fatigue occurring in approximately 1-10% of patients.
While weakness is not a primary pharmacodynamic effect of semaglutide, several indirect mechanisms may contribute to feelings of weakness in individuals taking Ozempic. These include changes in blood glucose levels, reduced caloric intake due to appetite suppression, gastrointestinal side effects (such as nausea, vomiting, or diarrhoea), and dehydration. The medication works by enhancing insulin secretion in a glucose-dependent manner, slowing gastric emptying, and reducing appetite—all of which can influence energy balance and subjective feelings of vitality.
Patients starting Ozempic may experience an adjustment period as their body adapts to the medication. Starting with a low dose and gradually increasing it (as recommended in the SmPC) can help reduce gastrointestinal side effects that may contribute to weakness. Many patients find that weakness may be transient and resolve as treatment continues, particularly if related to initial gastrointestinal symptoms.
If you are experiencing persistent or severe weakness whilst taking Ozempic, it is advisable to discuss this with your GP or diabetes specialist nurse. They can assess whether the symptom is related to the medication, an underlying condition, or another factor requiring investigation or adjustment to your treatment plan.
Blood Sugar Changes and Energy Levels on Ozempic
One of the primary mechanisms by which Ozempic may contribute to feelings of weakness is through alterations in blood glucose levels. Semaglutide enhances glucose-dependent insulin secretion from pancreatic beta cells and suppresses inappropriate glucagon release. Whilst this action improves glycaemic control in people with type 2 diabetes, it can occasionally lead to hypoglycaemia (low blood sugar), particularly when Ozempic is used in combination with other glucose-lowering agents such as sulphonylureas or insulin. When initiating Ozempic, your doctor may reduce doses of these medications to lower the risk of hypoglycaemia.
Symptoms of hypoglycaemia include:
-
Trembling or shakiness
-
Sweating
-
Palpitations
-
Confusion or difficulty concentrating
-
Weakness or fatigue
-
Hunger
If hypoglycaemia occurs (blood glucose below 4 mmol/L), treat it promptly with 15-20g of fast-acting carbohydrates (such as glucose tablets, fruit juice, or sugary sweets). Recheck your blood glucose after 10-15 minutes and repeat treatment if needed. If your next meal is more than an hour away, follow with a longer-acting carbohydrate snack.
Blood glucose monitoring is particularly important for those taking Ozempic alongside insulin or sulphonylureas, or for those with a history of hypoglycaemia. For other patients, your healthcare team will advise on whether regular self-monitoring is necessary, in line with NICE guidance (NG28).
Conversely, some individuals may experience relative hyperglycaemia if their diabetes is not yet optimally controlled, which can also manifest as fatigue and weakness.
As Ozempic improves overall glycaemic control, some patients report enhanced energy levels over time. The initial adjustment period may involve fluctuations in energy, but improvements in HbA1c and metabolic health often correlate with better overall well-being. Maintaining a balanced diet with adequate carbohydrate intake, tailored to individual needs, supports stable blood glucose and energy levels throughout the day.
Managing Weakness While Taking Ozempic
If you are experiencing weakness whilst taking Ozempic, several practical strategies can help manage this symptom and improve your overall sense of well-being. Firstly, ensure you are maintaining adequate nutrition despite the appetite-suppressing effects of the medication. Ozempic slows gastric emptying and reduces hunger, which can lead to significantly reduced caloric intake. Whilst this contributes to weight loss, insufficient energy intake may result in fatigue and weakness.
Nutritional strategies include:
-
Eating small, frequent meals throughout the day to maintain energy levels
-
Prioritising nutrient-dense foods, including lean proteins, whole grains, fruits, and vegetables
-
Ensuring adequate hydration, as dehydration can exacerbate feelings of weakness
-
Avoiding excessive restriction of carbohydrates, which are the body's primary energy source
Gastrointestinal side effects such as nausea, vomiting, and diarrhoea are common with Ozempic, particularly during dose escalation. These symptoms can lead to reduced food intake and fluid loss, both of which contribute to weakness. If these side effects are problematic, discuss with your healthcare provider about slowing the dose titration or temporarily reducing the dose as per the SmPC guidance. Managing these side effects through dietary modifications (such as eating bland, easily digestible foods) and anti-emetic medication if prescribed can help maintain nutritional status.
If vomiting or diarrhoea persist for more than 24 hours or you are unable to maintain adequate hydration, seek medical advice promptly as there is a risk of dehydration and acute kidney injury.
Regular physical activity, tailored to your fitness level, can paradoxically improve energy levels and reduce feelings of fatigue. However, if weakness is significant, it may be necessary to temporarily reduce exercise intensity and gradually rebuild activity levels as symptoms improve.
If you are taking other diabetes medications alongside Ozempic, your healthcare team may need to adjust doses to reduce the risk of low blood sugar.
Finally, ensure you are getting adequate sleep and managing stress, as both can significantly impact energy levels and overall well-being. If weakness persists despite these measures, further medical evaluation is warranted to exclude other underlying causes.
When to Seek Medical Advice About Weakness
Whilst mild, transient weakness during the initial weeks of Ozempic treatment may be manageable with self-care strategies, certain symptoms warrant prompt medical attention. It is important to recognise when weakness may indicate a more serious underlying issue requiring clinical assessment.
You should contact your GP or diabetes specialist nurse if:
-
Weakness is severe, persistent, or progressively worsening
-
You experience recurrent episodes of hypoglycaemia (blood glucose below 4 mmol/L)
-
Weakness is accompanied by chest pain, shortness of breath, or palpitations
-
You have significant muscle weakness affecting mobility or daily activities
-
Gastrointestinal symptoms (nausea, vomiting, diarrhoea) are severe or prolonged, leading to dehydration
-
You notice unexplained weight loss beyond what is expected with treatment
-
You develop symptoms of pancreatitis (severe, persistent abdominal pain radiating to the back)
-
You experience right upper quadrant pain, fever or jaundice (possible gallbladder issues)
-
You notice new or sudden changes in your vision
-
You have reduced urine output or confusion (possible dehydration or kidney problems)
Contact NHS 111 for urgent but non-life-threatening concerns, or seek emergency care (call 999 or attend A&E) if:
-
You experience symptoms of severe hypoglycaemia with confusion, loss of consciousness, or seizures
-
You have signs of severe dehydration (extreme dizziness, reduced urine output, rapid heartbeat)
-
You develop symptoms suggestive of diabetic ketoacidosis (though rare with GLP-1 receptor agonists like Ozempic), such as abdominal pain, vomiting, rapid breathing, and ketones in blood or urine
Your healthcare provider can conduct a thorough assessment, including blood tests to evaluate glucose control, electrolyte balance, kidney function, and thyroid status. They may also review your medication regimen to determine whether dose adjustments or alternative treatments are appropriate. NICE guidance emphasises individualised diabetes management, and your treatment plan should be tailored to your specific needs and tolerability.
If you suspect you are experiencing side effects from Ozempic, you can report these through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk). Regular follow-up appointments allow for monitoring of both therapeutic efficacy and potential adverse effects, ensuring that your diabetes management remains safe and effective whilst optimising your quality of life.
Frequently Asked Questions
How common is weakness as a side effect of Ozempic?
Fatigue and weakness occur in approximately 1–10% of patients taking Ozempic, as listed in the Summary of Product Characteristics. These symptoms are typically transient and may resolve as the body adapts to treatment.
Can Ozempic cause low blood sugar leading to weakness?
Ozempic can cause hypoglycaemia (low blood sugar), particularly when used with sulphonylureas or insulin, which may manifest as weakness, trembling, sweating, and confusion. Your doctor may adjust doses of other diabetes medications to reduce this risk.
When should I contact my doctor about weakness on Ozempic?
Contact your GP or diabetes specialist nurse if weakness is severe, persistent, or worsening, if you experience recurrent hypoglycaemia, or if weakness is accompanied by chest pain, severe gastrointestinal symptoms, dehydration, or reduced mobility.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript