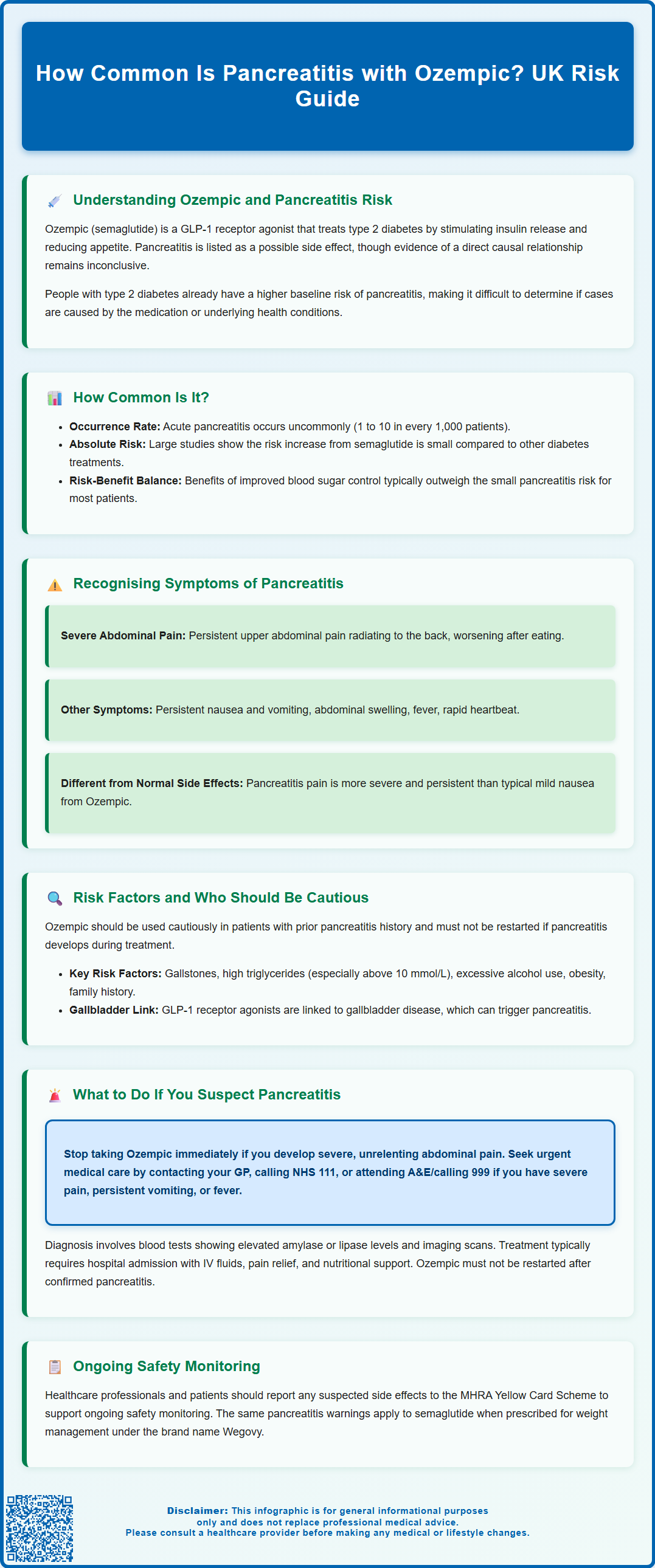
How common is pancreatitis with Ozempic? Pancreatitis is classified as an 'uncommon' adverse reaction with Ozempic (semaglutide), occurring in approximately 1 in 1,000 to 1 in 100 patients. Ozempic is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Whilst pancreatitis remains a recognised potential side effect, the absolute risk is small, and people with type 2 diabetes already have an elevated baseline risk of developing this condition. Understanding the symptoms, risk factors, and when to seek medical attention is essential for safe use of this medication.
Summary: Pancreatitis with Ozempic occurs uncommonly, affecting approximately 1 in 1,000 to 1 in 100 patients according to UK regulatory data.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus treatment.
- Acute pancreatitis is listed as an 'uncommon' adverse reaction in the Summary of Product Characteristics.
- Patients with type 2 diabetes have an elevated baseline risk of pancreatitis independent of medication use.
- Severe, persistent upper abdominal pain radiating to the back is the hallmark symptom requiring immediate medical attention.
- Ozempic should be discontinued immediately if pancreatitis is suspected and must not be restarted after a confirmed episode.
- The MHRA and EMA continue to monitor GLP-1 receptor agonists, with benefits typically outweighing risks for most patients.
Table of Contents
Understanding Ozempic and Pancreatitis Risk
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite. These mechanisms help improve glycaemic control and often lead to weight reduction, making Ozempic an effective option for many patients with type 2 diabetes.
Since its introduction, there has been ongoing discussion within the medical community regarding a potential association between GLP-1 receptor agonists and acute pancreatitis. Pancreatitis is inflammation of the pancreas that can range from mild, self-limiting episodes to severe, life-threatening conditions requiring intensive care. The concern arose from pre-clinical animal studies and post-marketing surveillance reports, prompting regulatory bodies including the Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) to monitor this potential adverse effect closely.
While evidence regarding a causal relationship remains inconclusive, pancreatitis is listed as a possible side effect in the Ozempic Summary of Product Characteristics (SmPC). The SmPC advises that semaglutide should be discontinued if pancreatitis is suspected. Patients with type 2 diabetes themselves have an elevated baseline risk of pancreatitis compared to the general population, which complicates the assessment of whether any observed cases are directly attributable to the medication or related to underlying metabolic factors and comorbidities.
It's worth noting that similar pancreatitis warnings apply to semaglutide when used for weight management (Wegovy).
How Common Is Pancreatitis with Ozempic?
In the Ozempic Summary of Product Characteristics (SmPC), acute pancreatitis is listed as an 'uncommon' adverse reaction (occurring in ≥1/1,000 to <1/100 patients). Cases were very infrequent in clinical trials, and real-world post-marketing data have been consistent with these findings.
People with type 2 diabetes have a higher baseline risk of developing pancreatitis compared to the general population. Large observational studies and meta-analyses examining GLP-1 receptor agonists, including semaglutide, suggest that the absolute risk increase attributable to the medication is small, with no clear increased risk versus comparator treatments.
It is crucial to interpret these statistics within the broader clinical context. The benefits of improved glycaemic control and weight management often outweigh the small potential risk of pancreatitis for most patients. The SUSTAIN-6 trial showed cardiovascular outcome benefits with semaglutide, though it's important to note that cardiovascular risk reduction is not currently part of Ozempic's UK licence. NICE guidance continues to support the use of semaglutide in appropriate patient populations, emphasising the importance of individualised risk assessment and informed decision-making between patients and their healthcare providers.
Healthcare professionals and patients are encouraged to report any suspected adverse reactions to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk), which helps maintain ongoing surveillance and ensures patient safety remains paramount.
Recognising Symptoms of Pancreatitis
Early recognition of pancreatitis symptoms is essential for prompt diagnosis and management. The hallmark symptom of acute pancreatitis is severe, persistent abdominal pain, typically located in the upper abdomen (epigastric region) and often radiating through to the back. This pain usually develops suddenly and may be described as a constant, boring, or knife-like sensation that worsens after eating, particularly following fatty meals.
Accompanying symptoms frequently include:
-
Nausea and vomiting that may be persistent and provide little relief
-
Abdominal tenderness and distension, with the abdomen feeling swollen or tight
-
Fever and tachycardia as systemic inflammatory responses develop
-
Loss of appetite and an inability to tolerate oral intake
-
In severe cases, signs of systemic illness such as jaundice, confusion, or shock
Patients taking Ozempic should be counselled to recognise these warning signs. The pain of pancreatitis is typically more severe and persistent than common gastrointestinal side effects associated with GLP-1 receptor agonists, such as mild nausea or dyspepsia, which tend to be transient and improve over time.
If you experience severe, unrelenting abdominal pain whilst taking Ozempic, you should stop the medication immediately and seek urgent medical attention. Do not wait to see if symptoms resolve on their own. Contact your GP urgently, call NHS 111 for advice, or attend your local Emergency Department if symptoms are severe. Timely assessment, including blood tests (serum amylase or lipase levels elevated to at least three times the upper limit of normal) and imaging studies, is necessary to confirm the diagnosis and determine the severity of inflammation, guiding appropriate treatment.
Risk Factors and Who Should Be Cautious
Certain patient characteristics and medical histories increase the baseline risk of developing pancreatitis, and these factors should be carefully considered before initiating Ozempic therapy. According to the SmPC, semaglutide should be used with caution in patients with a history of pancreatitis. If pancreatitis occurs while on semaglutide therapy, the medication should not be restarted.
Other important risk factors include:
-
Gallstones (cholelithiasis), which are the leading cause of acute pancreatitis in the UK
-
Hypertriglyceridaemia, particularly when triglyceride levels exceed 10 mmol/L
-
Excessive alcohol consumption, a well-established independent risk factor
-
Obesity, which is associated with both gallstone formation and metabolic dysfunction
-
Family history of pancreatitis or genetic predisposition
It's also worth noting that GLP-1 receptor agonists, including semaglutide, have been associated with gallbladder disease, which can itself precipitate pancreatitis. Patients should be advised to seek medical attention if they develop symptoms suggestive of gallbladder problems, such as right upper quadrant pain, nausea, or jaundice.
Before prescribing Ozempic, healthcare professionals should conduct a thorough clinical assessment, including a detailed medical history and baseline investigations. NICE guidance (NG28) recommends that lipid profiles, including triglyceride levels, should be monitored in patients with diabetes. If significant hypertriglyceridaemia is present, this should be addressed before considering GLP-1 receptor agonist therapy.
Patients should be counselled about modifiable risk factors, particularly alcohol intake and weight management. Shared decision-making is essential—discussing both the benefits of improved diabetes control and the small but recognised risk of pancreatitis allows patients to make informed choices about their treatment. For those at higher risk, alternative glucose-lowering therapies may be more appropriate.
What to Do If You Suspect Pancreatitis
If you develop symptoms suggestive of pancreatitis whilst taking Ozempic, immediate action is required. The first step is to discontinue Ozempic and refrain from taking any further doses until you have been assessed by a healthcare professional. Do not attempt to self-manage severe abdominal pain, as pancreatitis can rapidly progress and lead to serious complications including pancreatic necrosis, infection, or multi-organ failure.
Seek urgent medical attention through one of the following routes:
-
Contact your GP practice immediately for same-day assessment if symptoms develop during working hours
-
Call NHS 111 for guidance if you are unsure about the severity or need advice outside normal surgery hours
-
Attend your local Emergency Department or call 999 if you experience severe pain, persistent vomiting, signs of dehydration, fever, or feel generally unwell
When you present for medical assessment, inform healthcare staff that you are taking Ozempic and describe your symptoms clearly. Diagnosis typically involves blood tests measuring serum amylase or lipase levels (elevated to at least three times the upper limit of normal), alongside imaging studies such as abdominal ultrasound or CT scanning to visualise pancreatic inflammation and identify potential complications.
Management of acute pancreatitis is primarily supportive and usually requires hospital admission. Treatment includes intravenous fluid resuscitation, pain relief, anti-emetics, and nutritional support. Most cases resolve with conservative management, though severe pancreatitis may necessitate intensive care.
It's important to monitor your blood glucose levels after stopping Ozempic and contact your diabetes team for advice on adjusting your diabetes treatment regimen.
Following a confirmed episode of pancreatitis, Ozempic should not be restarted, as stated in the SmPC. Your diabetes care team will need to review your treatment plan and consider alternative glucose-lowering therapies. It is essential to attend follow-up appointments to ensure your diabetes remains well controlled and to address any underlying risk factors that may have contributed to the pancreatitis episode.
Frequently Asked Questions
What are the warning signs of pancreatitis whilst taking Ozempic?
The hallmark symptom is severe, persistent upper abdominal pain that often radiates through to the back, accompanied by nausea, vomiting, abdominal tenderness, and fever. If you experience these symptoms, stop Ozempic immediately and seek urgent medical attention.
Should I stop taking Ozempic if I've had pancreatitis before?
Ozempic should be used with caution in patients with a history of pancreatitis, and following a confirmed episode of pancreatitis whilst on semaglutide, the medication must not be restarted. Discuss alternative diabetes treatments with your healthcare team.
How is pancreatitis diagnosed if I'm taking Ozempic?
Diagnosis involves blood tests measuring serum amylase or lipase levels (elevated to at least three times the upper limit of normal) alongside imaging studies such as abdominal ultrasound or CT scanning to visualise pancreatic inflammation.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript