Ozempic (semaglutide) is a once-weekly GLP-1 receptor agonist licensed in the UK for type 2 diabetes management. As its use becomes increasingly common, patients and clinicians often question whether Ozempic and local anaesthesia can be safely combined during minor procedures. Whilst local anaesthetics do not directly interact with semaglutide, the medication's effect on gastric emptying raises important considerations for procedural safety. Understanding when Ozempic can be continued and when it may need temporary adjustment is essential for safe perioperative care. This article examines the evidence and UK clinical guidance on managing Ozempic therapy around procedures involving local anaesthesia.
Summary: Local anaesthesia can generally be administered safely to patients taking Ozempic, as there is no direct drug interaction between semaglutide and local anaesthetic agents.
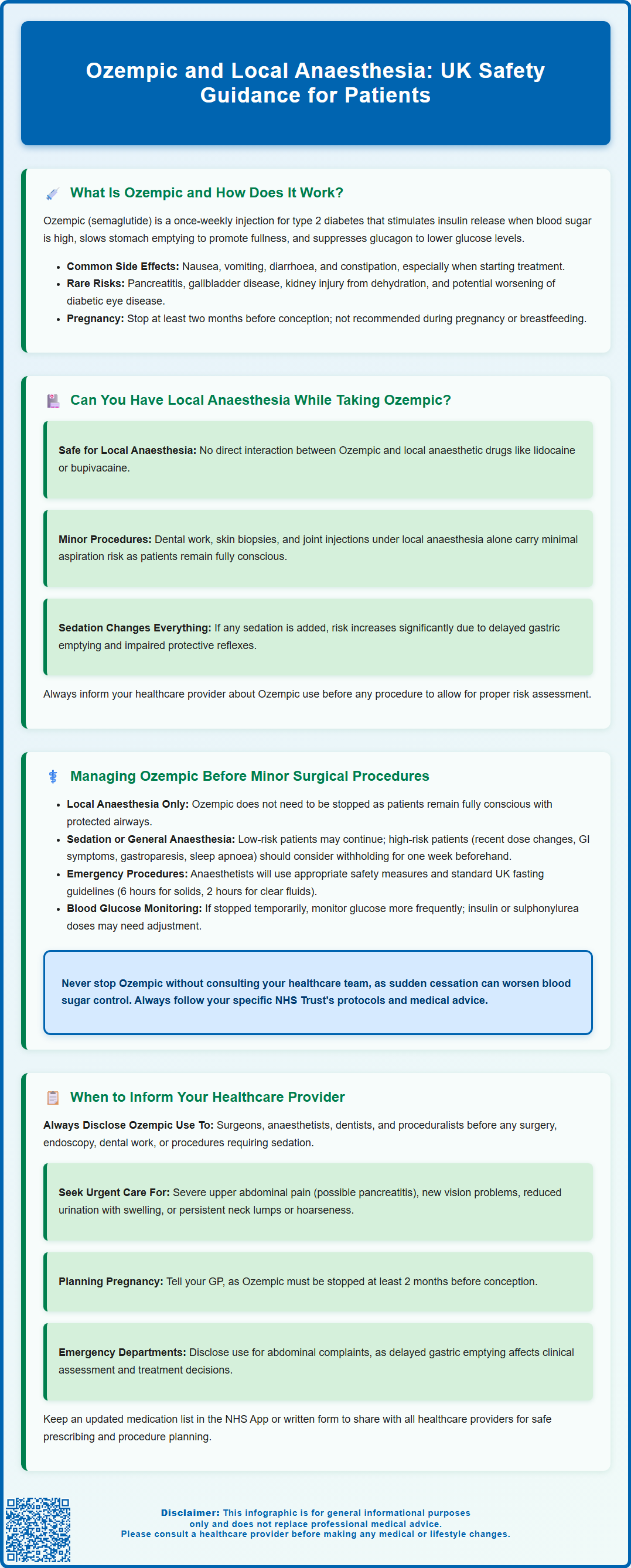
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes, administered as a once-weekly subcutaneous injection.
- The primary concern relates to delayed gastric emptying caused by semaglutide, which increases aspiration risk during procedures involving sedation or general anaesthesia.
- For minor procedures under local anaesthesia alone (without sedation), Ozempic can typically be continued as patients maintain full consciousness and protective airway reflexes.
- Patients should always inform procedural clinicians about Ozempic use to allow individualised risk assessment and adherence to local NHS Trust protocols.
- If sedation is required alongside local anaesthesia, a risk-stratified approach may be necessary, particularly for patients with ongoing gastrointestinal symptoms or recent dose escalation.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, it works by mimicking the action of the naturally occurring hormone GLP-1, which is released from the gut in response to food intake. While Wegovy (also semaglutide) is specifically licensed for weight management, Ozempic is not licensed for this purpose in the UK.
Semaglutide binds to GLP-1 receptors on pancreatic beta cells, stimulating insulin secretion in a glucose-dependent manner. This means insulin is released only when blood glucose levels are elevated, reducing the risk of hypoglycaemia compared with some diabetes medications. However, when used with insulin or sulphonylureas, the risk of hypoglycaemia increases.
Beyond glycaemic control, Ozempic exerts several other physiological effects. It slows gastric emptying, which prolongs the sensation of fullness and contributes to weight loss. It also suppresses glucagon secretion from pancreatic alpha cells, further helping to lower blood glucose levels. The SUSTAIN-6 trial showed that semaglutide may reduce the risk of major adverse cardiovascular events in people with type 2 diabetes and established cardiovascular disease, though this is not a licensed indication in the UK.
Common adverse effects include nausea, vomiting, diarrhoea, and constipation, particularly during dose escalation. Less common but serious side effects include pancreatitis, gallbladder disease, acute kidney injury (particularly from dehydration), and potential worsening of diabetic retinopathy in some patients. These gastrointestinal symptoms typically improve over time. Patients are advised to start on a low dose and titrate gradually to minimise these effects.
Semaglutide is not recommended during pregnancy or breastfeeding. Women of childbearing potential should discontinue Ozempic at least two months before a planned pregnancy.
Understanding how Ozempic works is essential when considering its interaction with anaesthesia and surgical procedures.
Can You Have Local Anaesthesia While Taking Ozempic?
Local anaesthesia can generally be administered safely to patients taking Ozempic, as there is no direct pharmacological interaction between semaglutide and local anaesthetic agents such as lidocaine, bupivacaine, or articaine. Local anaesthetics work by blocking sodium channels in nerve fibres, preventing the transmission of pain signals, and this mechanism does not interfere with GLP-1 receptor activity or glucose metabolism.
However, the primary concern when combining Ozempic with any form of anaesthesia—including local anaesthesia—relates to delayed gastric emptying. Semaglutide can slow the rate at which the stomach empties its contents into the small intestine, though this effect may attenuate somewhat with chronic treatment. This physiological effect persists even between doses due to the medication's long half-life of approximately one week. In the context of procedures requiring sedation or general anaesthesia, delayed gastric emptying increases the risk of aspiration (inhalation of stomach contents into the lungs), which can lead to serious complications such as aspiration pneumonitis.
For minor procedures performed under local anaesthesia alone—such as dental work, skin biopsies, joint injections, or minor dermatological surgery—the risk of aspiration is generally minimal because the patient remains fully conscious and maintains protective airway reflexes. Therefore, routine continuation of Ozempic is typically appropriate in these circumstances.
That said, if the procedure involves any element of sedation (such as conscious sedation for dental anxiety or endoscopy), the risk profile changes. Even light sedation can impair protective reflexes, and the combination with delayed gastric emptying warrants careful consideration. In such cases, healthcare providers may recommend a risk-stratified approach, particularly for patients in the dose-escalation phase, those with ongoing gastrointestinal symptoms, known gastroparesis, or autonomic neuropathy.
Patients should always inform their dentist, dermatologist, or procedural clinician about their Ozempic use to allow for individualised risk assessment and to follow local NHS Trust policies regarding GLP-1 receptor agonists and procedural sedation.
Managing Ozempic Before Minor Surgical Procedures
Current UK practice regarding GLP-1 receptor agonist therapy in the perioperative period varies, with many NHS Trusts developing local protocols for managing medications like Ozempic before procedures. While there is no single national guideline, the UK Clinical Pharmacy Association (UKCPA) and the Centre for Perioperative Care (CPOC) provide frameworks for perioperative diabetes management.
For procedures under local anaesthesia without sedation, there is generally no need to stop Ozempic. Patients maintain full consciousness and airway protection throughout these procedures.
For procedures involving sedation or general anaesthesia, a risk-stratified approach is recommended:
-
Low-risk patients (stable on therapy, no significant gastrointestinal symptoms): Many clinicians continue Ozempic with appropriate precautions
-
Higher-risk patients (recent dose escalation, significant gastrointestinal symptoms, known gastroparesis, obesity with obstructive sleep apnoea): Consider withholding the weekly dose before the procedure, typically for one week for once-weekly formulations like Ozempic
The decision to withhold Ozempic must balance the risk of aspiration against the potential for worsening glycaemic control and the clinical urgency of the procedure. This decision should be made collaboratively between the patient, their diabetes care team, and the procedural or surgical team.
For emergency or urgent procedures, it may not be feasible to wait for drug washout. In these situations, anaesthetists will employ appropriate safety measures based on individual risk assessment. Standard UK fasting guidelines should be followed (6 hours for solids, 2 hours for clear fluids), with the anaesthetist determining if additional precautions are needed.
If Ozempic is temporarily withheld, blood glucose monitoring becomes particularly important. Patients should check their capillary blood glucose more frequently, and those taking insulin or sulphonylureas may need dose adjustments to prevent hypoglycaemia.
Patients should never stop Ozempic without medical advice, as abrupt cessation can lead to deterioration in glycaemic control. Always follow the specific advice of your healthcare team and local NHS Trust protocols, which may vary based on local expertise and patient populations.
When to Inform Your Healthcare Provider About Ozempic Use
Patients taking Ozempic should proactively disclose their medication use in several key clinical scenarios to ensure safe and effective care. Transparency about GLP-1 agonist therapy allows healthcare providers to make informed decisions about procedural planning, anaesthetic management, and perioperative care.
Before any planned surgical or procedural intervention, patients must inform their surgeon, anaesthetist, dentist, or proceduralist about Ozempic use. This includes:
-
Elective surgery under general or regional anaesthesia
-
Endoscopic procedures (gastroscopy, colonoscopy) requiring sedation
-
Dental procedures involving sedation or general anaesthesia
-
Diagnostic imaging requiring sedation (e.g., MRI in claustrophobic patients)
-
Cosmetic procedures involving sedation or anaesthesia
Even for minor procedures under local anaesthesia, it is good practice to mention Ozempic use, as clinical circumstances may change (e.g., unexpected need for sedation, procedural complications requiring escalation of care).
Patients should seek urgent medical attention if they experience:
-
Severe or persistent upper abdominal pain (especially if radiating to the back and accompanied by vomiting), which may indicate pancreatitis – contact NHS 111, your GP urgently, or go to A&E if severe
-
Symptoms of gallbladder disease (pain in the upper right abdomen, particularly after eating)
-
New or worsening visual problems, which could indicate diabetic retinopathy complications
-
Signs of acute kidney injury (reduced urination, swelling, fatigue) particularly if experiencing severe vomiting or diarrhoea
Patients should also inform their GP or diabetes specialist about:
-
Persistent gastrointestinal symptoms (nausea, vomiting, abdominal pain)
-
Neck symptoms (lump, hoarseness, difficulty swallowing) that persist
-
Planned pregnancy or confirmed pregnancy, as semaglutide should be discontinued at least 2 months before a planned pregnancy and is not recommended during pregnancy or breastfeeding
Emergency department attendance also warrants disclosure of Ozempic use, particularly if presenting with abdominal symptoms, as delayed gastric emptying may complicate clinical assessment and management.
Maintaining an up-to-date medication list—including over-the-counter medicines and supplements—and sharing this with all healthcare providers is essential for safe prescribing and procedural planning. Patients can use the NHS App or carry a written list to facilitate accurate communication.
Suspected side effects can be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- Ozempic - European Public Assessment Report.
- GLP-1 and dual GIP/GLP-1 receptor agonists: potential risk of pulmonary aspiration during general anaesthesia or deep sedation.
- Perioperative Care of People with Diabetes Undergoing Surgery.
- Handbook of Perioperative Medicines.
Frequently Asked Questions
Do I need to stop Ozempic before dental treatment with local anaesthetic?
For routine dental procedures using local anaesthesia alone (without sedation), you can generally continue Ozempic as normal. However, always inform your dentist about your medication, as procedures involving sedation may require different management.
Why is delayed gastric emptying a concern with Ozempic and anaesthesia?
Ozempic slows gastric emptying, meaning food remains in the stomach longer. During procedures involving sedation or general anaesthesia, this increases the risk of aspiration (inhaling stomach contents into the lungs), which can cause serious complications.
Should I inform my surgeon about taking Ozempic before a minor procedure?
Yes, you should always inform any healthcare provider performing a procedure about your Ozempic use. This allows them to assess your individual risk and follow appropriate local NHS Trust protocols for safe perioperative management.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










