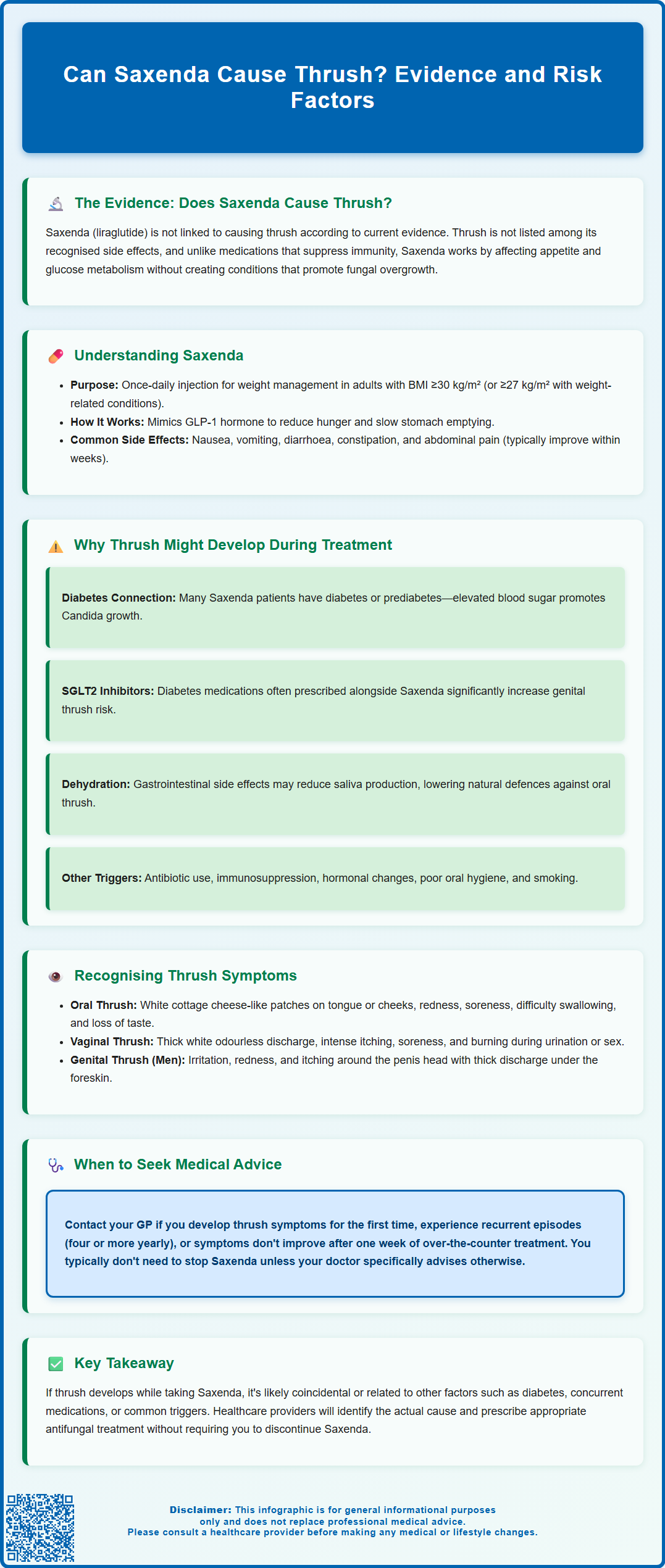
Can Saxenda cause thrush? This is a common concern among patients prescribed liraglutide for weight management. Thrush, a fungal infection caused by Candida species, is not listed as a recognised side effect of Saxenda in UK prescribing information. However, patients using Saxenda may develop thrush due to other factors, particularly if they have type 2 diabetes or take certain co-prescribed medications such as SGLT2 inhibitors. Understanding the relationship between Saxenda, underlying health conditions, and thrush risk helps patients distinguish between medication effects and coincidental infections, ensuring appropriate management and continuation of weight loss treatment.
Summary: Saxenda (liraglutide) does not directly cause thrush and is not associated with increased fungal infection risk according to UK prescribing information.
- Saxenda is a GLP-1 receptor agonist used for weight management, not linked to immunosuppression or Candida overgrowth.
- Patients with type 2 diabetes have inherently higher thrush risk due to elevated blood glucose, regardless of Saxenda use.
- SGLT2 inhibitors (often co-prescribed with Saxenda) significantly increase genital thrush risk through their mechanism of action.
- Thrush developing during Saxenda treatment typically relates to underlying conditions, co-medications, or coincidental factors rather than liraglutide itself.
- Patients experiencing thrush symptoms should consult their GP for diagnosis and antifungal treatment without necessarily discontinuing Saxenda.
Table of Contents
Can Saxenda Cause Thrush?
Saxenda (liraglutide) is not directly associated with causing thrush according to current evidence and the official UK Summary of Product Characteristics (SmPC). Thrush, a fungal infection caused by Candida species, is not listed among the recognised adverse effects in Saxenda's prescribing information. However, patients using Saxenda may still develop thrush for reasons unrelated to the medication itself.
There is no evidence that liraglutide increases susceptibility to fungal infections. Saxenda works as a glucagon-like peptide-1 (GLP-1) receptor agonist, primarily affecting appetite regulation and glucose metabolism. Unlike some medications that directly suppress immune function or alter the oral environment (such as inhaled corticosteroids), Saxenda does not create conditions that typically promote Candida overgrowth.
That said, patients undergoing weight management treatment may experience various health changes that could indirectly influence thrush risk. Factors such as dietary modifications, stress related to lifestyle changes, or concurrent health conditions might contribute to fungal infections. Importantly, individuals with type 2 diabetes—a population that often uses GLP-1 receptor agonists—have an inherently higher risk of thrush due to elevated blood glucose levels, which can encourage Candida growth. Additionally, SGLT2 inhibitors (such as dapagliflozin or empagliflozin), which are commonly prescribed alongside GLP-1 medications for diabetes, significantly increase the risk of genital thrush.
If you develop symptoms of thrush whilst taking Saxenda, it is advisable to consult your GP or healthcare provider. They can assess whether the infection is coincidental or related to other factors in your medical history, and provide appropriate antifungal treatment. Understanding the distinction between medication side effects and coincidental health issues is essential for effective management.
Understanding Saxenda and Its Common Side Effects
Saxenda (liraglutide 3 mg) is a prescription medication licensed in the UK for weight management in adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with weight-related comorbidities such as type 2 diabetes, hypertension, or dyslipidaemia. It's worth noting that NHS access criteria, as defined by NICE guidance, are narrower than the licensed indication. Saxenda belongs to the GLP-1 receptor agonist class and is administered as a once-daily subcutaneous injection.
The mechanism of action involves mimicking the naturally occurring hormone GLP-1, which regulates appetite and food intake. Saxenda works by:
-
Slowing gastric emptying, which prolongs feelings of fullness
-
Acting on appetite centres in the brain to reduce hunger
-
Supporting sustainable weight loss when combined with diet and exercise
-
Improving glycaemic control as a physiological effect (though Saxenda is not indicated for diabetes treatment)
The most commonly reported adverse effects of Saxenda according to the UK SmPC include:
-
Nausea and vomiting (very common, affecting more than 1 in 10 people)
-
Diarrhoea or constipation (very common)
-
Abdominal pain and dyspepsia (common, affecting between 1 in 10 and 1 in 100 people)
-
Injection site reactions such as bruising or irritation (common)
-
Headache and dizziness (common)
-
Increased heart rate (common)
Serious adverse effects include pancreatitis (uncommon), gallbladder disease (common), and hypoglycaemia (common, particularly in patients taking concomitant diabetes medications such as insulin or sulfonylureas). Dehydration and renal impairment secondary to vomiting or diarrhoea may also occur. Patients should be counselled about recognising symptoms of these conditions. The prescribing information does not list immunosuppression or increased infection risk as recognised effects. Most gastrointestinal side effects improve as the body adjusts to treatment, typically within the first few weeks.
Why Thrush Might Develop During Saxenda Treatment
Whilst Saxenda itself does not cause thrush, several factors associated with weight management treatment or the patient's underlying health status may contribute to fungal infections. Understanding these potential contributors helps distinguish between medication effects and coincidental health issues.
Diabetes and blood glucose control represent the most significant risk factor for thrush among Saxenda users. Many patients prescribed Saxenda have type 2 diabetes or prediabetes. Elevated blood glucose levels create an environment conducive to Candida overgrowth, as the fungus thrives on sugar. Saxenda actually improves glycaemic control, which should theoretically reduce thrush risk in diabetic patients over time.
Medications commonly co-prescribed with Saxenda may increase thrush risk. SGLT2 inhibitors (such as dapagliflozin, empagliflozin, or canagliflozin) significantly increase the risk of genital thrush due to their mechanism of action causing glucose excretion in urine. If you develop thrush while taking Saxenda, your healthcare provider should review all your medications.
Dietary changes during weight management may potentially play a role. Patients following calorie-restricted diets might experience nutritional changes that could affect immune function. Dehydration, sometimes occurring with gastrointestinal side effects like vomiting or diarrhoea, may reduce saliva production, which is a natural defence against oral thrush.
Other contributing factors unrelated to Saxenda include:
-
Antibiotic use, which disrupts normal bacterial flora and allows Candida overgrowth
-
Immunosuppression from other medications or underlying conditions
-
Hormonal changes, particularly in women, affecting vaginal thrush risk
-
Poor oral hygiene or ill-fitting dentures
-
Smoking, which damages oral mucosa
Stress and lifestyle changes associated with weight management programmes may temporarily affect immune function. If you develop thrush whilst taking Saxenda, your healthcare provider will assess these various factors to identify the underlying cause and ensure appropriate treatment. There is no evidence suggesting that discontinuing Saxenda is necessary for thrush management.
Recognising Symptoms of Oral and Vaginal Thrush
Early recognition of thrush symptoms enables prompt treatment and prevents complications. Thrush can affect different body sites, with oral and vaginal thrush being most common. Understanding the characteristic features helps patients identify when medical attention is needed.
Oral thrush (oropharyngeal candidiasis) typically presents with:
-
White patches or plaques on the tongue, inner cheeks, gums, tonsils, or roof of the mouth
-
Redness or soreness in the mouth and throat
-
Difficulty swallowing or a sensation of food sticking
-
Loss of taste or an unpleasant taste in the mouth
-
Cracking at the corners of the mouth (angular cheilitis)
-
Cotton-like sensation in the mouth
The white patches may resemble cottage cheese and can be wiped off with some effort, often leaving red, inflamed areas that might bleed slightly. Some patients experience no symptoms, with thrush discovered incidentally during dental or medical examinations.
Vaginal thrush (vulvovaginal candidiasis) is characterised by:
-
Thick, white vaginal discharge resembling cottage cheese, usually odourless
-
Intense itching around the vagina and vulva
-
Soreness, redness, and swelling of the vaginal tissues
-
Stinging or burning during urination or sexual intercourse
-
Vaginal discomfort or irritation
In men, genital thrush may cause irritation, redness, and itching around the head of the penis, along with a thick discharge under the foreskin.
It is important to note that these symptoms can overlap with other conditions. Oral lesions might indicate other infections or inflammatory conditions, whilst vaginal symptoms could represent bacterial vaginosis or sexually transmitted infections. Self-diagnosis is not recommended. If you experience these symptoms whilst taking Saxenda, contact your GP or pharmacist for proper assessment. They can confirm the diagnosis through clinical examination or laboratory testing and prescribe appropriate antifungal treatment. Uncomplicated vaginal thrush often responds to treatment within 1-3 days, while oral thrush typically resolves within 7–14 days of appropriate therapy.
When to Seek Medical Advice About Thrush on Saxenda
Knowing when to contact your healthcare provider ensures appropriate management of thrush and continuation of your weight management treatment. Most cases of thrush are straightforward to treat, but certain situations require prompt medical attention.
You should contact your GP or pharmacist if you:
-
Develop symptoms suggestive of thrush for the first time, to confirm the diagnosis
-
Experience recurrent thrush (four or more episodes within 12 months)
-
Have symptoms that do not improve after one week of over-the-counter antifungal treatment
-
Are pregnant or breastfeeding and develop thrush symptoms (note that oral fluconazole should be avoided in pregnancy; topical azoles such as clotrimazole are preferred)
-
Have a weakened immune system due to conditions like HIV or medications such as chemotherapy
-
Experience severe symptoms including difficulty swallowing, high fever, or spreading infection
Seek urgent medical attention if you develop:
-
Severe difficulty swallowing or breathing
-
Signs of systemic infection such as high fever, chills, or feeling generally unwell
-
Spreading redness or swelling beyond the initial affected area
-
Symptoms in infants or young children, who require specialist assessment
Regarding your Saxenda treatment, there is typically no need to discontinue the medication due to thrush unless your clinician advises otherwise. Your healthcare provider will:
-
Confirm the diagnosis through clinical examination or swab testing
-
Prescribe appropriate antifungal treatment, such as oral fluconazole (except in pregnancy), nystatin suspension, or topical clotrimazole
-
Investigate underlying causes, particularly assessing diabetes control if relevant
-
Review your medication list for other potential contributing factors, especially SGLT2 inhibitors
-
Provide advice on prevention, including oral hygiene and managing risk factors
According to NICE guidance, uncomplicated thrush can often be managed with short courses of antifungal therapy. Your healthcare provider will ensure that any prescribed antifungal medication is compatible with Saxenda and your other medications. Continue your Saxenda injections as prescribed unless specifically advised otherwise. If you experience any suspected side effects from Saxenda, you or your healthcare professional can report them via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Frequently Asked Questions
Is thrush a recognised side effect of Saxenda?
No, thrush is not listed as a recognised adverse effect in Saxenda's UK Summary of Product Characteristics. There is no evidence that liraglutide increases susceptibility to fungal infections.
Why might I develop thrush whilst taking Saxenda?
Thrush during Saxenda treatment typically relates to other factors such as type 2 diabetes (which increases Candida risk), co-prescribed SGLT2 inhibitors, antibiotic use, or hormonal changes rather than the liraglutide itself.
Should I stop taking Saxenda if I develop thrush?
No, there is typically no need to discontinue Saxenda due to thrush unless your clinician advises otherwise. Consult your GP for appropriate antifungal treatment whilst continuing your prescribed Saxenda regimen.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript