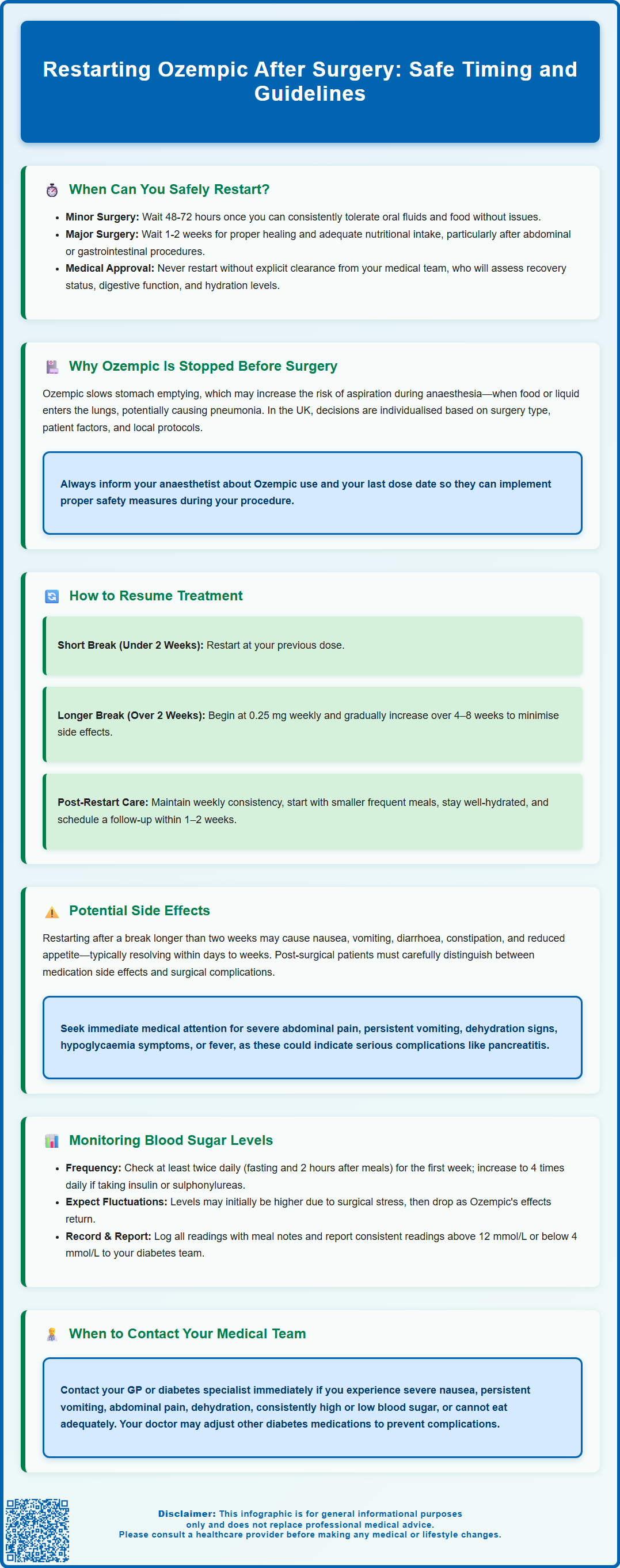
Restarting Ozempic after surgery requires careful timing and medical supervision to ensure safe recovery. This GLP-1 receptor agonist, used for type 2 diabetes management in the UK, is often paused before procedures due to delayed gastric emptying concerns. The restart timeline varies from 48–72 hours after minor surgery to one to two weeks following major operations, depending on your recovery, gastrointestinal function, and ability to tolerate food. Your surgeon and diabetes team will determine the optimal approach based on individual factors, including blood glucose control and post-operative complications. Never resume Ozempic without explicit medical approval, as premature reintroduction may compromise healing or cause gastrointestinal distress during this vulnerable period.
Summary: Ozempic can typically be restarted 48–72 hours after minor surgery or one to two weeks after major procedures, once you can tolerate oral intake and your medical team approves resumption.
- Ozempic is a GLP-1 receptor agonist that slows gastric emptying, which may increase aspiration risk during anaesthesia.
- Restart timing depends on surgery type, recovery progress, gastrointestinal function, and ability to maintain adequate nutrition.
- If stopped for over two weeks, re-titration from a lower dose (0.25 mg weekly) is often recommended to minimise side effects.
- Common restart side effects include nausea, vomiting, diarrhoea, and abdominal discomfort, typically resolving within days to weeks.
- Blood glucose monitoring should increase to at least twice daily during the restart period, with adjustments to concurrent diabetes medications as needed.
- Always obtain explicit approval from your surgeon or diabetes specialist before administering the first post-operative dose.
Table of Contents
When Can You Safely Restart Ozempic After Surgery?
The timing for restarting Ozempic (semaglutide) after surgery depends on several factors, including the type of procedure performed, your recovery progress, and your ability to resume normal eating and drinking. Clinical practice suggests waiting until you can tolerate oral fluids and food consistently before reintroducing this medication, typically within 48 to 72 hours after minor procedures. However, for major abdominal or gastrointestinal surgery, your healthcare team may recommend a longer interval of one to two weeks to ensure adequate healing and nutritional intake.
Your surgeon and diabetes specialist should work together to determine the optimal restart time based on your individual circumstances. Key considerations include:
-
Your post-operative recovery status and any complications
-
Return of normal gastrointestinal function (absence of nausea, vomiting, or ileus)
-
Ability to maintain adequate hydration and nutrition
-
Current blood glucose control and insulin requirements
-
Type and extent of surgical intervention
For patients who underwent emergency surgery or experienced post-operative complications, the restart timeline may be extended further. It is essential never to restart Ozempic without explicit approval from your medical team, as premature reintroduction could interfere with wound healing, nutritional recovery, or cause gastrointestinal distress during a vulnerable period.
If you were using Ozempic for type 2 diabetes management (its licensed indication in the UK), your healthcare provider will likely monitor your blood glucose levels closely during the interruption period and may prescribe alternative medications or adjust insulin doses temporarily. For those using semaglutide for weight management (where Wegovy is the licensed product in the UK), the brief interruption is unlikely to significantly impact long-term outcomes, and safe resumption takes priority over continuity of treatment.
The UK Centre for Perioperative Care (CPOC) and Joint British Diabetes Societies (JBDS) provide guidance for healthcare professionals on managing diabetes medications during the perioperative period, which your clinical team will follow.
Why Ozempic Is Stopped Before Surgical Procedures
Ozempic belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by slowing gastric emptying, enhancing insulin secretion, and reducing appetite. Whilst these mechanisms are beneficial for diabetes and weight management, they create specific considerations in the perioperative setting that may necessitate temporary discontinuation.
The primary concern relates to delayed gastric emptying, which could potentially increase the risk of pulmonary aspiration during anaesthesia. When stomach contents empty more slowly, food and liquid may remain in the stomach longer than expected, even after appropriate fasting periods. During induction of anaesthesia or in the recovery period, this retained gastric content could be regurgitated and aspirated into the lungs, potentially causing aspiration pneumonitis or pneumonia.
In the UK, perioperative management of GLP-1 receptor agonists like Ozempic is increasingly risk-stratified rather than universally discontinued. The UK Clinical Pharmacy Association (UKCPA) Handbook of Perioperative Medicines notes that decisions should be based on individual patient factors and local protocols. Your anaesthetist will assess your specific risks and may recommend stopping the medication before planned surgery based on this assessment.
Factors that may influence the decision to stop Ozempic include:
-
Type and urgency of surgery (particularly upper gastrointestinal procedures)
-
Risk of post-operative nausea and vomiting
-
Potential interference with post-surgical nutrition and hydration
-
Difficulty assessing surgical complications if gastrointestinal symptoms occur
-
Blood glucose management during the stress of surgery
For emergency surgery where stopping Ozempic in advance is impossible, anaesthetists will take appropriate precautions based on your clinical situation. Your anaesthetist should always be informed of recent Ozempic use, including the date of your last dose, to ensure appropriate safety measures are implemented. Always follow the specific advice of your healthcare team regarding medication management before surgery.
How to Resume Ozempic Treatment Post-Surgery
Restarting Ozempic after surgery requires a systematic, cautious approach to minimise side effects and ensure safe reintroduction. Your healthcare provider will guide you through this process, which may differ from your initial titration schedule depending on how long the medication was interrupted.
If you stopped Ozempic for less than two weeks, you can typically restart at your previous maintenance dose once cleared by your medical team. However, if the interruption exceeded two weeks, many clinicians recommend restarting at a lower dose (usually 0.25 mg weekly) and gradually re-titrating upwards according to the licensed schedule (0.25 mg → 0.5 mg → 1 mg, and potentially to 2 mg for type 2 diabetes) over 4–8 weeks to reduce gastrointestinal side effects. This approach mirrors the initial dose escalation protocol in the Ozempic Summary of Product Characteristics (SmPC) and helps your body readjust to the medication's effects on gastric emptying and appetite.
Practical steps for safe resumption include:
-
Obtain explicit approval from your surgeon or diabetes specialist before administering the first post-operative dose
-
Ensure you can tolerate normal meals and fluids without nausea, vomiting, or significant discomfort
-
Administer the injection at the same day each week as before surgery to maintain consistency
-
Start with smaller, frequent meals for the first few days after restarting to assess tolerance
-
Stay well-hydrated, as dehydration can worsen potential side effects
Your healthcare provider may schedule a follow-up appointment within 1–2 weeks of restarting to assess your tolerance, review blood glucose readings, and adjust the dose if necessary. Keep a record of any side effects, blood sugar levels, and dietary intake to discuss at this appointment. If you experience severe nausea, vomiting, abdominal pain, or signs of dehydration after restarting, contact your GP or diabetes team promptly rather than continuing with subsequent doses.
Patients who have undergone bariatric or major gastrointestinal surgery may need a more individualised approach to restarting Ozempic, with potential modifications to the standard re-titration schedule. In these cases, close collaboration between your bariatric team and diabetes specialists is essential.
Potential Side Effects When Restarting Ozempic
When reintroducing Ozempic after a surgical interruption, you may experience similar side effects to those encountered when first starting the medication, particularly if the break exceeded two weeks. The most common adverse effects are gastrointestinal in nature and typically diminish as your body readjusts to the medication over several weeks.
Common side effects when restarting include:
-
Nausea and vomiting (affecting approximately 15-20% of patients according to the SmPC)
-
Diarrhoea or constipation
-
Abdominal discomfort or bloating
-
Reduced appetite (which may be more pronounced if you're still recovering nutritionally)
-
Fatigue or general malaise
-
Injection site reactions (redness, itching, or mild swelling)
These effects are generally mild to moderate and self-limiting, resolving within days to a few weeks. However, in the post-surgical context, distinguishing between medication side effects and surgical complications can be challenging. Contact your healthcare provider immediately if you experience:
-
Severe, persistent abdominal pain (could indicate pancreatitis, gallbladder disease, or surgical complications)
-
Persistent vomiting preventing fluid intake (risk of dehydration and acute kidney injury)
-
Signs of dehydration (dark urine, dizziness, reduced urination)
-
Symptoms of hypoglycaemia if taking other diabetes medications
-
Unusual fatigue, fever, or wound-related concerns
The Ozempic SmPC specifically mentions pancreatitis and gallbladder disease as potential risks that require prompt medical attention. While there is limited specific evidence regarding restarting Ozempic after surgery, the post-operative period represents a time of physiological stress and altered metabolism, making careful monitoring essential. If side effects are intolerable, your healthcare provider may recommend a slower re-titration schedule, temporary dose reduction, or consideration of alternative diabetes management strategies until you have fully recovered from surgery.
Monitoring Blood Sugar Levels During the Restart Period
Careful glucose monitoring is essential when restarting Ozempic after surgery, as the perioperative period and medication interruption can significantly affect blood sugar control. The stress response to surgery, changes in diet and activity, pain medications, and the reintroduction of Ozempic all influence glucose levels in complex ways.
NICE guidance (NG28) for type 2 diabetes recommends more frequent blood glucose monitoring during periods of illness, medication changes, or physiological stress—all of which apply to the post-surgical period. If you don't routinely monitor at home, your healthcare team may provide a glucose meter and testing supplies specifically for this transition period.
Recommended monitoring approach:
-
Test blood glucose at least twice daily (fasting and 2 hours post-meal) for the first week after restarting Ozempic
-
Increase testing frequency to 4 times daily if you take insulin or sulfonylureas alongside Ozempic, due to hypoglycaemia risk
-
Record all readings along with notes about meals, activity, and any symptoms
-
Report consistent readings above 12 mmol/L or below 4 mmol/L to your diabetes team
Be aware that blood glucose levels may initially be higher than pre-surgery values due to the medication interruption and surgical stress response. Conversely, as Ozempic's effects re-establish and your appetite decreases, glucose levels may drop, particularly if you're taking other glucose-lowering medications. Your healthcare provider may need to adjust doses of concurrent diabetes medications such as insulin, sulfonylureas, or SGLT2 inhibitors to prevent hypoglycaemia.
If you are also taking an SGLT2 inhibitor (medications like empagliflozin, dapagliflozin, or canagliflozin), be particularly vigilant as these are often temporarily stopped around surgery and require careful monitoring when restarted due to the risk of euglycaemic diabetic ketoacidosis.
Contact your GP or diabetes specialist if:
-
Blood glucose remains consistently above 12 mmol/L despite restarting Ozempic
-
You experience symptoms of hypoglycaemia (shaking, sweating, confusion, rapid heartbeat)
-
You're unable to eat adequately due to nausea or other side effects
-
You have concerns about your diabetes management during recovery
For urgent concerns outside normal hours, contact NHS 111 or attend A&E if you have severe symptoms. Your healthcare team will typically schedule a review appointment 2–4 weeks after restarting to assess glucose control, review your monitoring records, evaluate medication tolerance, and make any necessary adjustments to your diabetes management plan. This collaborative approach ensures safe, effective resumption of Ozempic whilst optimising your overall post-surgical recovery and long-term metabolic health.
Frequently Asked Questions
How long after surgery can I restart Ozempic?
You can typically restart Ozempic 48–72 hours after minor procedures or one to two weeks after major abdominal or gastrointestinal surgery, once you can tolerate oral intake and your medical team approves. The exact timing depends on your individual recovery and surgical type.
Do I need to restart Ozempic at a lower dose after surgery?
If you stopped Ozempic for less than two weeks, you can usually resume at your previous dose. If the interruption exceeded two weeks, many clinicians recommend restarting at 0.25 mg weekly and gradually re-titrating upwards to reduce gastrointestinal side effects.
What side effects should I watch for when restarting Ozempic after surgery?
Common side effects include nausea, vomiting, diarrhoea, and abdominal discomfort. Contact your healthcare provider immediately if you experience severe abdominal pain, persistent vomiting, signs of dehydration, or symptoms that could indicate surgical complications rather than medication effects.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












