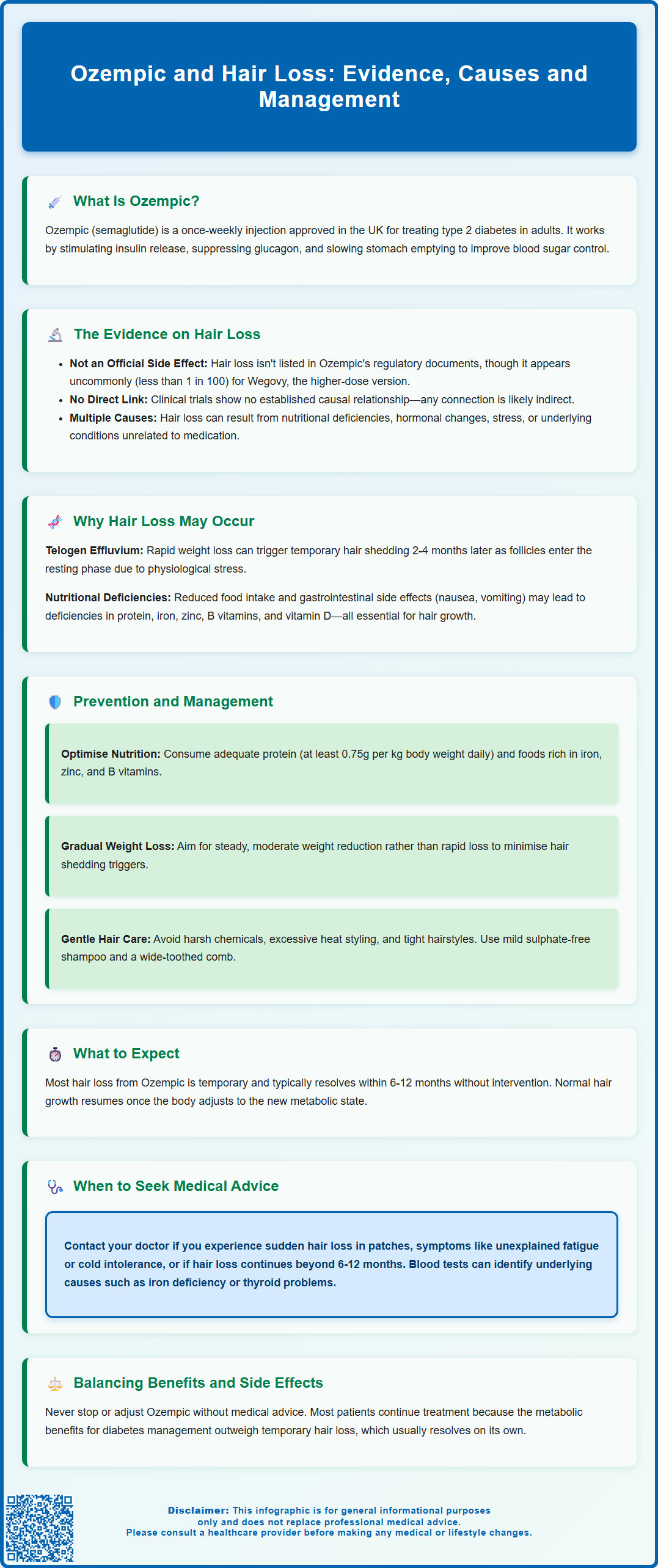
Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, administered as a once-weekly injection. Whilst the medication effectively lowers blood glucose and HbA1c levels, some patients have reported hair thinning or shedding during treatment. Hair loss is not listed as a recognised adverse effect in Ozempic's UK prescribing information, though it appears as an uncommon reaction with the higher-dose formulation Wegovy. Understanding the potential mechanisms—including rapid weight loss and nutritional changes—can help patients and clinicians manage this concern whilst maintaining effective diabetes control.
Summary: Hair loss is not a recognised adverse effect of Ozempic in UK prescribing information, though some patients report hair thinning likely related to rapid weight loss rather than direct drug effects.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed for type 2 diabetes, administered as a once-weekly subcutaneous injection.
- Alopecia is not listed in Ozempic's Summary of Product Characteristics but appears as uncommon (less than 1 in 100) with higher-dose Wegovy.
- Rapid weight loss can trigger telogen effluvium, causing temporary hair shedding 2-4 months after the metabolic stress.
- Nutritional deficiencies in protein, iron, zinc, and B vitamins may contribute to hair loss during treatment.
- Patients experiencing severe, patchy, or persistent hair loss beyond 6-12 months should seek GP assessment and blood tests.
- Most telogen effluvium cases resolve spontaneously within 6-12 months with nutritional optimisation and supportive care.
Table of Contents
Understanding Ozempic and Its Primary Uses
Ozempic (semaglutide) is a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that regulates blood sugar levels and appetite.
The medication is administered as a once-weekly subcutaneous injection and functions through several mechanisms. Primarily, Ozempic stimulates insulin secretion from the pancreas when blood glucose levels are elevated, whilst simultaneously suppressing the release of glucagon, a hormone that raises blood sugar. Additionally, it slows gastric emptying, which helps to reduce post-meal glucose spikes and promotes a feeling of fullness that can lead to reduced calorie intake.
Ozempic has been shown in clinical trials to effectively lower HbA1c levels (a measure of long-term blood glucose control) and is often prescribed when other diabetes medications have not achieved adequate glycaemic control. A notable secondary effect observed in clinical studies is weight loss. It is important to note that Ozempic is not licensed for weight management in the UK. A higher-dose formulation of semaglutide (marketed as Wegovy) has been specifically licensed for chronic weight management in certain patient groups.
The Medicines and Healthcare products Regulatory Agency (MHRA) has approved Ozempic for use in the UK, and NICE guidelines (NG28) recommend GLP-1 receptor agonists as a treatment option for adults with type 2 diabetes when specific criteria are met, typically in combination with other diabetes medications. Patients prescribed Ozempic should receive proper training on injection technique and be monitored regularly for efficacy and potential adverse effects.
The Link Between Ozempic and Hair Loss: What the Evidence Shows
Hair loss, medically termed alopecia, has been reported anecdotally by some individuals taking Ozempic, though it is important to understand the current evidence base. Hair loss is not listed as an adverse effect in the official Summary of Product Characteristics (SmPC) for Ozempic approved by the MHRA or the European Medicines Agency (EMA). The most frequently reported side effects in clinical trials include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation.
Interestingly, alopecia is listed as an uncommon adverse reaction (affecting less than 1 in 100 people) in the SmPC for Wegovy, the higher-dose semaglutide product licensed for weight management. This difference may reflect the higher dosage used or the effects of more substantial weight loss.
Post-marketing surveillance and patient reports have drawn attention to potential hair thinning or shedding in some users. It is crucial to note that there is no established causal relationship between Ozempic and hair loss based on current clinical trial data. The medication's prescribing information does not identify alopecia as a recognised adverse drug reaction, which suggests that if a link exists, it may be related to secondary effects rather than a direct pharmacological effect of semaglutide itself.
Several factors complicate the assessment of this potential association. Firstly, hair loss can occur for numerous reasons unrelated to medication, including nutritional deficiencies, hormonal changes, stress, and underlying medical conditions. Secondly, many patients taking Ozempic experience significant weight loss, which is itself a recognised trigger for a specific type of hair shedding called telogen effluvium. This condition typically occurs several months after a physiological stressor, such as rapid weight reduction, major surgery, or severe illness.
Healthcare professionals should be aware that whilst patient experiences are valid and warrant investigation, the current evidence does not support a direct mechanism by which semaglutide would cause hair loss. Any patient experiencing a suspected adverse drug reaction should report it through the MHRA Yellow Card Scheme.
Why Hair Loss May Occur During Ozempic Treatment
Understanding the potential mechanisms behind hair loss in patients taking Ozempic requires consideration of several interconnected factors, most of which relate to the metabolic and nutritional changes associated with the medication's effects rather than direct drug toxicity to hair follicles.
Rapid weight loss is perhaps the most significant contributing factor. When individuals lose weight quickly, the body may interpret this as a form of physiological stress. This can trigger telogen effluvium, a condition where hair follicles prematurely enter the resting (telogen) phase of the hair growth cycle. Typically, this results in noticeable hair shedding approximately 2-4 months after the triggering event. The hair loss is usually temporary, and normal growth resumes once the body adjusts to the new metabolic state.
Nutritional deficiencies represent another important consideration. Ozempic's appetite-suppressing effects and the associated reduction in food intake may lead to inadequate consumption of essential nutrients vital for healthy hair growth. Key nutrients include protein (hair is primarily composed of keratin, a protein), iron, zinc, B vitamins (including B12), and vitamin D. Patients following very low-calorie diets or those with pre-existing nutritional deficiencies may be particularly vulnerable.
Additionally, the gastrointestinal side effects commonly experienced with Ozempic—such as nausea, vomiting, and diarrhoea—can further compromise nutritional status by reducing appetite and potentially affecting nutrient absorption. Chronic nausea may lead patients to avoid nutrient-dense foods, whilst severe or prolonged diarrhoea could potentially impact absorption of certain nutrients.
It is also worth noting that type 2 diabetes itself can be associated with hair changes, as can other conditions that frequently coexist with diabetes, such as thyroid disorders, polycystic ovary syndrome (PCOS), and autoimmune conditions. Therefore, a comprehensive assessment is essential to identify the true cause of hair loss in any individual patient.
Managing and Preventing Hair Loss While Taking Ozempic
For patients experiencing hair thinning or shedding whilst taking Ozempic, several practical strategies may help to minimise this effect and support healthy hair regrowth. It is important to emphasise that most cases of telogen effluvium are self-limiting, with hair typically returning to normal within 6-12 months once the triggering factor is addressed.
Optimising nutritional intake is paramount. Patients should aim to consume a balanced, nutrient-rich diet that provides adequate protein (at least 0.75g per kilogram of body weight daily; higher amounts may be appropriate for some individuals, though patients with kidney disease should discuss protein intake with their healthcare team). Foods rich in iron (lean red meat, dark leafy greens, pulses), zinc (shellfish, nuts, seeds, whole grains), and B vitamins (eggs, dairy, fortified cereals) should be emphasised. Some patients may benefit from a targeted supplement if blood tests confirm specific deficiencies, though this should be discussed with a healthcare professional.
Moderating the rate of weight loss can also be beneficial. Whilst weight reduction is often a desired outcome of Ozempic therapy, aiming for a gradual, steady loss as recommended in NHS healthy weight guidance is generally safer and less likely to trigger telogen effluvium than very rapid weight reduction. This may involve working with a dietitian to ensure adequate calorie and nutrient intake whilst still achieving glycaemic and weight management goals.
Gentle hair care practices are advisable during periods of increased shedding. Patients should avoid harsh chemical treatments, excessive heat styling, and tight hairstyles that place tension on hair follicles. Using a mild, sulphate-free shampoo and a wide-toothed comb can help minimise mechanical damage to fragile hair.
Some individuals may wish to consider topical treatments such as minoxidil, though evidence for its efficacy in telogen effluvium is limited. Any such treatment should be discussed with a GP or dermatologist. Importantly, patients should not stop or adjust their Ozempic dose without medical advice, as the benefits for diabetes management typically outweigh temporary hair-related side effects. If nutritional intake is significantly affected by side effects, a healthcare professional may consider adjusting the titration schedule or reviewing the treatment plan.
When to Seek Medical Advice About Hair Loss
Whilst mild hair shedding during Ozempic treatment may not require immediate medical intervention, certain circumstances warrant prompt assessment by a healthcare professional. Patients should contact their GP or diabetes specialist nurse if they experience any of the following:
-
Sudden or severe hair loss, particularly if it occurs in patches (which may suggest alopecia areata, an autoimmune condition) rather than diffuse thinning
-
Hair loss accompanied by other symptoms such as unexplained fatigue, cold intolerance, weight changes beyond those expected, skin changes, or mood disturbances, which could indicate thyroid dysfunction or other endocrine disorders
-
Scalp symptoms including redness, scaling, itching, or pain, which may suggest a dermatological condition requiring specific treatment
-
Hair loss that persists beyond 6-12 months or continues to worsen despite nutritional optimisation and other supportive measures
-
Concerns about nutritional deficiencies, particularly if dietary intake has been significantly reduced or if gastrointestinal symptoms have been severe
A thorough medical assessment typically includes a detailed history (including medication review, dietary assessment, and family history of hair loss), physical examination of the scalp and hair, and blood tests to evaluate potential underlying causes. Initial investigations in UK primary care usually include full blood count, ferritin (iron stores), and thyroid function tests. Additional tests such as vitamin B12, folate, and vitamin D may be considered based on clinical assessment. If taking biotin supplements, patients should inform their healthcare provider, as high-dose biotin can interfere with certain laboratory tests, including thyroid function tests.
If hair loss is confirmed to be related to Ozempic therapy—either directly or through associated weight loss and nutritional factors—the healthcare team will discuss the risks and benefits of continuing treatment. In most cases, the metabolic benefits of Ozempic for diabetes management outweigh the temporary inconvenience of hair thinning, particularly given that telogen effluvium typically resolves spontaneously. However, each patient's situation is unique, and treatment decisions should be individualised based on clinical need, patient preferences, and the severity of adverse effects. If the diagnosis remains uncertain or hair loss persists despite initial management, referral to a dermatologist may be appropriate.
Frequently Asked Questions
Does Ozempic directly cause hair loss?
Hair loss is not listed as a recognised adverse effect in Ozempic's UK prescribing information. Any hair thinning is more likely related to rapid weight loss triggering telogen effluvium or nutritional deficiencies rather than a direct pharmacological effect of semaglutide.
How long does hair loss last with Ozempic treatment?
If hair loss occurs due to telogen effluvium from rapid weight loss, it typically begins 2-4 months after starting treatment and resolves within 6-12 months once the body adjusts. Normal hair growth usually resumes with nutritional optimisation and supportive care.
Should I stop taking Ozempic if I experience hair loss?
Do not stop or adjust Ozempic without medical advice, as the benefits for diabetes management typically outweigh temporary hair-related effects. Discuss concerns with your GP or diabetes specialist, who can assess underlying causes and optimise nutritional support whilst continuing treatment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










