Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist used to manage type 2 diabetes in adults. Whilst effective for glycaemic control, Ozempic and breastfeeding are not compatible according to UK regulatory guidance. The Medicines and Healthcare products Regulatory Agency (MHRA) and manufacturer's Summary of Product Characteristics clearly state that semaglutide should not be used during lactation due to insufficient data on its excretion in human breast milk. For breastfeeding mothers with type 2 diabetes, established alternatives such as insulin and metformin offer safe, effective options with robust safety profiles. This article examines the evidence, risks, and alternative treatments available.
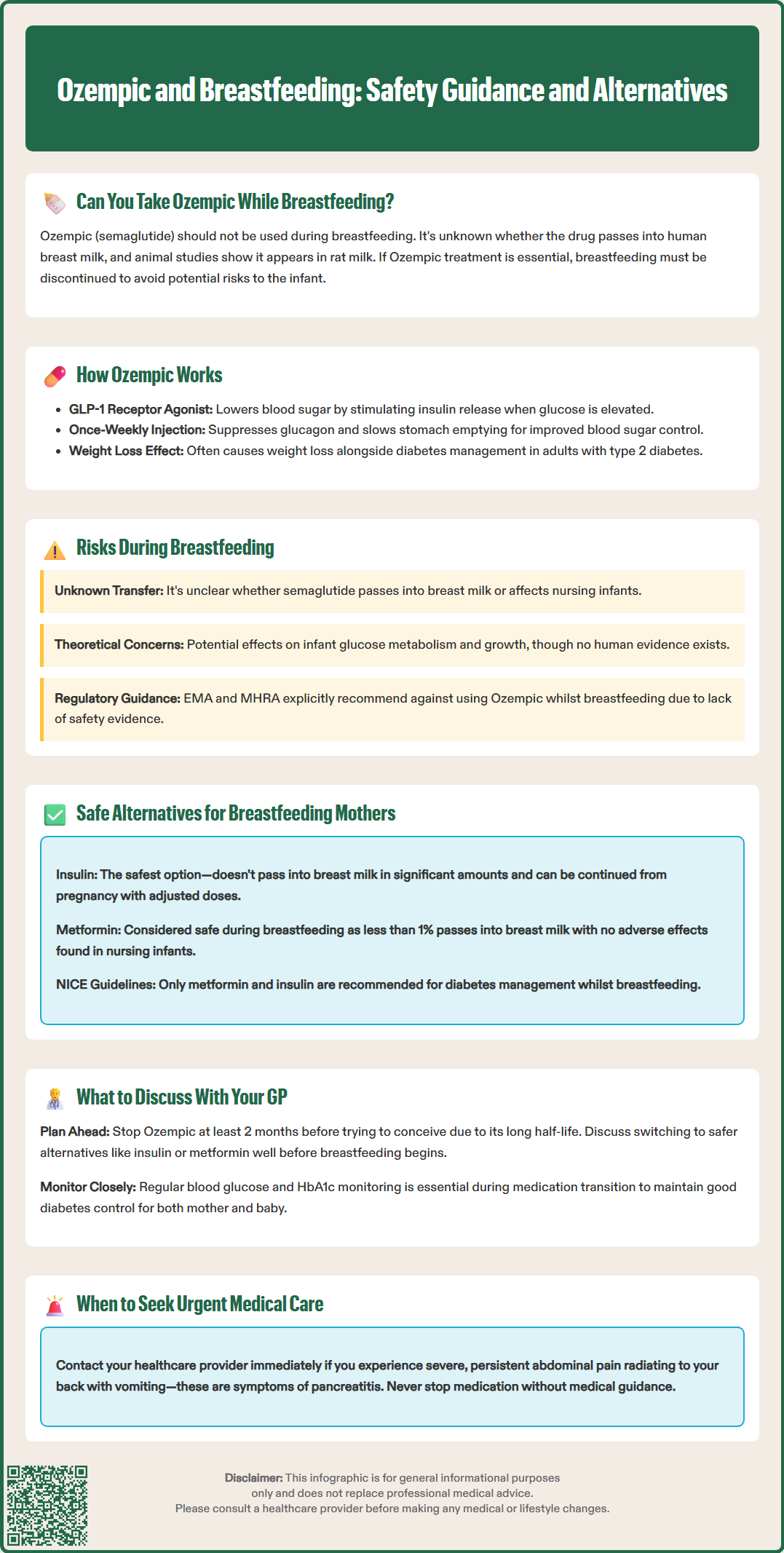
Summary: Ozempic (semaglutide) should not be used during breastfeeding due to unknown transfer into breast milk and absence of human safety data.
- Semaglutide is a GLP-1 receptor agonist that stimulates insulin secretion, suppresses glucagon, and slows gastric emptying to control blood glucose in type 2 diabetes.
- UK regulatory guidance (MHRA, SmPC) explicitly states Ozempic should be avoided during lactation as it is unknown whether semaglutide is excreted in human breast milk.
- Safe alternatives for breastfeeding mothers include insulin (does not pass into milk in significant amounts) and metformin (less than 1% of maternal dose enters milk).
- NICE guideline NG3 recommends only metformin and insulin for diabetes management during breastfeeding, avoiding other oral agents and GLP-1 agonists.
- Discontinue semaglutide at least 2 months before planned pregnancy and consult your GP immediately if breastfeeding is intended to arrange safe alternative treatment.
- Uncontrolled diabetes poses risks to both mother and infant, making individualised medical guidance essential for balancing effective glycaemic control with breastfeeding safety.
Table of Contents

Mounjaro®
Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy®
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereCan You Take Ozempic While Breastfeeding?
Ozempic (semaglutide) should not be used during breastfeeding according to the Medicines and Healthcare products Regulatory Agency (MHRA) and the manufacturer's guidance. The Summary of Product Characteristics (SmPC) clearly states that it is unknown whether semaglutide is excreted in human breast milk, and due to this uncertainty, the medication should be avoided during lactation.
Currently, there are no adequate human studies examining semaglutide levels in breast milk or its impact on milk production. Animal studies have shown that semaglutide and similar GLP-1 receptor agonists can be detected in the milk of lactating rats, though the relevance of these findings to humans remains unclear. If treatment with semaglutide is deemed essential, breastfeeding should be discontinued.
The decision regarding diabetes medication during breastfeeding requires careful consideration of the benefits to the mother against potential risks to the infant. For women with type 2 diabetes who are breastfeeding, several well-established treatment options exist with more robust safety data. The NHS and NICE guidelines (NG3) emphasise individualised care, recommending metformin and/or insulin as the preferred options during breastfeeding.
If you are currently taking Ozempic and discover you are pregnant or wish to breastfeed, contact your healthcare provider immediately to discuss alternative management strategies. The SmPC advises discontinuing semaglutide at least 2 months before a planned pregnancy. Do not stop taking prescribed medication without medical guidance, as uncontrolled diabetes can also pose risks to both mother and child.
How Ozempic Works and Its Safety Profile
Ozempic contains semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist that mimics the action of the naturally occurring hormone GLP-1. This medication works through several complementary mechanisms to improve blood glucose control in adults with type 2 diabetes. Semaglutide stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it only triggers insulin release when blood sugar levels are elevated, thereby reducing the risk of hypoglycaemia when used alone.
Additionally, Ozempic suppresses glucagon secretion, a hormone that raises blood glucose levels, and slows gastric emptying, which helps moderate the post-meal rise in blood sugar. These actions collectively improve glycaemic control and often lead to weight loss, which can be beneficial for many people with type 2 diabetes. The medication is administered once weekly via subcutaneous injection.
The general safety profile of Ozempic in non-pregnant, non-breastfeeding adults has been established through extensive clinical trials. Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, which typically diminish over time. More serious but rare risks include pancreatitis, diabetic retinopathy complications (particularly in people with pre-existing retinopathy and rapid improvement in glycaemic control), gallbladder disease (cholelithiasis/cholecystitis), and potential thyroid C-cell tumours (observed in animal studies). When combined with insulin or sulfonylureas, there is an increased risk of hypoglycaemia.
Safety data specific to breastfeeding is lacking. While the molecular weight of semaglutide (approximately 4,113 Da) might theoretically limit passage into breast milk, this has not been confirmed in human studies. The EMA and MHRA product information explicitly states that Ozempic should not be used during breastfeeding due to this absence of data.
Risks of Using Ozempic During Breastfeeding
The primary concern with using Ozempic during breastfeeding centres on the unknown transfer of semaglutide into breast milk and potential effects on the nursing infant. The UK SmPC is clear that semaglutide should not be used during breastfeeding due to this uncertainty.
Potential theoretical risks to the breastfed infant could include effects on glucose metabolism and growth, though it must be emphasised that there is no clinical evidence in humans to date. GLP-1 receptors are present throughout the body, including in the developing pancreas and gastrointestinal system. Exposure to a GLP-1 agonist during infancy could theoretically interfere with normal metabolic development, though no causal link has been established between Ozempic and specific infant complications. The gastrointestinal side effects commonly experienced by adults taking Ozempic raise theoretical questions about similar effects in infants, but again, no human data exist to confirm or refute these concerns.
Regarding impact on maternal milk production, there is no established evidence that Ozempic directly affects milk supply. While the medication's effects on appetite and food intake could theoretically influence a mother's nutritional status, this remains speculative without supporting clinical data.
For mothers with type 2 diabetes, uncontrolled blood glucose also poses risks during the breastfeeding period, including increased susceptibility to infections and delayed healing. Therefore, the decision-making process must balance the need for effective diabetes management against the precautionary principle of avoiding medications with unknown safety profiles in lactation. Your healthcare team can help assess your individual circumstances and guide you towards the safest treatment approach, which typically involves medications with established safety profiles during breastfeeding.
Alternative Diabetes Treatments for Breastfeeding Mothers
Fortunately, several diabetes treatments have established safety profiles during breastfeeding, allowing mothers to maintain good glycaemic control whilst nursing. The choice of treatment depends on individual circumstances, including the severity of diabetes, previous treatment response, and personal preferences.
Insulin remains the gold standard for managing diabetes during breastfeeding. It does not pass into breast milk in clinically significant amounts due to its large molecular size and protein structure, which would be digested in the infant's gastrointestinal tract if any trace amounts were present. Both long-acting basal insulins and rapid-acting mealtime insulins are considered safe. Many women who required insulin during pregnancy can continue the same regimen whilst breastfeeding, with dose adjustments as needed. The NHS and NICE guidelines support insulin as a first-line option for breastfeeding mothers requiring injectable therapy.
Metformin is generally considered compatible with breastfeeding. This oral medication, which reduces hepatic glucose production and improves insulin sensitivity, passes into breast milk in very small quantities—typically less than 1% of the maternal dose. Extensive clinical experience and published studies have not identified adverse effects in breastfed infants whose mothers take metformin. It is often the preferred oral agent for women with type 2 diabetes who are breastfeeding.
NICE guideline NG3 recommends that during breastfeeding, only metformin and insulin should be used for diabetes management. Other oral hypoglycaemic agents, including sulfonylureas such as glibenclamide, should be avoided. SGLT2 inhibitors are not recommended during breastfeeding due to theoretical concerns about effects on the developing infant kidney, while DPP-4 inhibitors have insufficient safety data in lactation.
Lifestyle modifications remain fundamental to diabetes management and are entirely safe during breastfeeding. A balanced diet, regular physical activity (as appropriate postpartum), and maintaining a healthy weight all contribute to improved glycaemic control. Breastfeeding itself can help with postpartum weight loss and may improve insulin sensitivity. Your diabetes care team, including specialist nurses and dietitians, can provide tailored advice on managing your condition through this period.
What to Discuss With Your GP Before Taking Ozempic
If you are considering Ozempic or are currently taking it and planning to breastfeed, a thorough discussion with your GP or diabetes specialist is essential. This conversation should occur well before you begin breastfeeding, ideally during pregnancy or when planning conception, to ensure a safe transition in your diabetes management.
Key topics to address include:
-
Your current diabetes control: Discuss your HbA1c levels, blood glucose patterns, and any complications. This helps determine the urgency and intensity of treatment needed.
-
Previous treatment responses: Review which medications have worked well for you in the past, including any you used before starting Ozempic. This information guides the selection of suitable alternatives.
-
Your breastfeeding plans: Be clear about your intentions and duration of breastfeeding, as this affects treatment planning. Some mothers may choose to exclusively breastfeed, whilst others may use mixed feeding, which could influence medication decisions.
-
Alternative treatment options: Ask your GP to explain the safety profile of insulin, metformin, and other suitable medications during breastfeeding. Understand the benefits and potential side effects of each option.
-
Timing of medication changes: If you need to switch from Ozempic to an alternative, discuss the optimal timing. Semaglutide has a long half-life (approximately one week), so planning the transition in advance is important. If you are planning pregnancy, the SmPC advises discontinuing semaglutide at least 2 months before conception.
Your GP should also arrange appropriate monitoring, including regular blood glucose checks and HbA1c measurements, to ensure your diabetes remains well-controlled during the transition. If you have pre-existing diabetic retinopathy, additional monitoring may be needed, particularly if your glycaemic control improves rapidly. You should also be advised to seek urgent medical assessment if you develop symptoms suggestive of pancreatitis, such as severe, persistent abdominal pain radiating to the back, often accompanied by vomiting.
Remember that good diabetes control benefits both you and your baby. Whilst Ozempic should not be used during breastfeeding, effective alternatives exist that allow you to safely manage your condition whilst providing the benefits of breastfeeding to your infant. Open communication with your healthcare team ensures you receive personalised, evidence-based care throughout this important period.
If you experience any side effects from your diabetes medication, report them to your healthcare provider and consider using the MHRA Yellow Card scheme to help monitor medication safety.
Frequently Asked Questions
Is Ozempic safe to take whilst breastfeeding?
No, Ozempic (semaglutide) should not be used during breastfeeding according to MHRA guidance, as it is unknown whether the medication passes into breast milk or affects the nursing infant.
What diabetes medications are safe during breastfeeding?
Insulin and metformin are considered safe and are recommended by NICE guidelines for managing diabetes during breastfeeding. Both have established safety profiles with extensive clinical experience in nursing mothers.
When should I stop taking Ozempic if I plan to breastfeed?
Contact your GP immediately if you are taking Ozempic and plan to breastfeed. The manufacturer advises discontinuing semaglutide at least 2 months before planned pregnancy, and your healthcare provider will arrange a safe transition to alternative diabetes treatments.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












