Mounjaro®
Dual-agonist support that helps curb appetite, hunger, and cravings to drive substantial, sustained weight loss.
- ~22.5% average body weight loss
- Significant weight reduction
- Improves blood sugar levels
- Clinically proven weight loss

Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist used to manage type 2 diabetes mellitus in adults. For breastfeeding mothers, understanding whether Ozempic is safe during lactation is crucial for both maternal diabetes control and infant wellbeing. Current UK guidance, including recommendations from the MHRA and NICE, advises against using Ozempic whilst breastfeeding due to insufficient data on its excretion into breast milk and potential effects on nursing infants. This article examines the evidence, explores safer alternatives such as metformin and insulin, and provides guidance on when to consult your GP about diabetes management during breastfeeding.
Summary: Ozempic (semaglutide) should not be used during breastfeeding according to UK regulatory guidance due to insufficient safety data.
Ozempic (semaglutide) is a prescription medication primarily used to manage type 2 diabetes mellitus in adults. It belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone in the body that regulates blood sugar levels.
The mechanism of action of Ozempic involves several key processes. Firstly, it stimulates insulin secretion from the pancreas in a glucose-dependent manner, meaning insulin is released only when blood sugar levels are elevated. This helps to lower blood glucose without causing excessive drops that could lead to hypoglycaemia. Secondly, Ozempic suppresses glucagon release, a hormone that raises blood sugar by prompting the liver to release stored glucose. By reducing glucagon, the medication helps prevent unnecessary glucose production.
Additionally, Ozempic slows gastric emptying, which means food moves more slowly from the stomach into the small intestine. This results in a more gradual rise in blood sugar after meals and can contribute to feelings of fullness. While this may assist with weight management in people with type 2 diabetes, it's important to note that Ozempic is not licensed for weight loss in the UK.
Ozempic is administered as a once-weekly subcutaneous injection, typically into the abdomen, thigh, or upper arm. Common adverse effects include nausea, vomiting, diarrhoea, and abdominal discomfort, particularly when starting treatment or increasing the dose. The risk of hypoglycaemia increases when Ozempic is used with insulin or sulfonylureas. More serious but rare risks include pancreatitis. Animal studies have shown thyroid C-cell tumours, though the relevance to humans is uncertain. Rapid improvement in blood glucose control may temporarily worsen diabetic retinopathy in some patients.
If you experience any side effects, report them via the MHRA Yellow Card scheme.
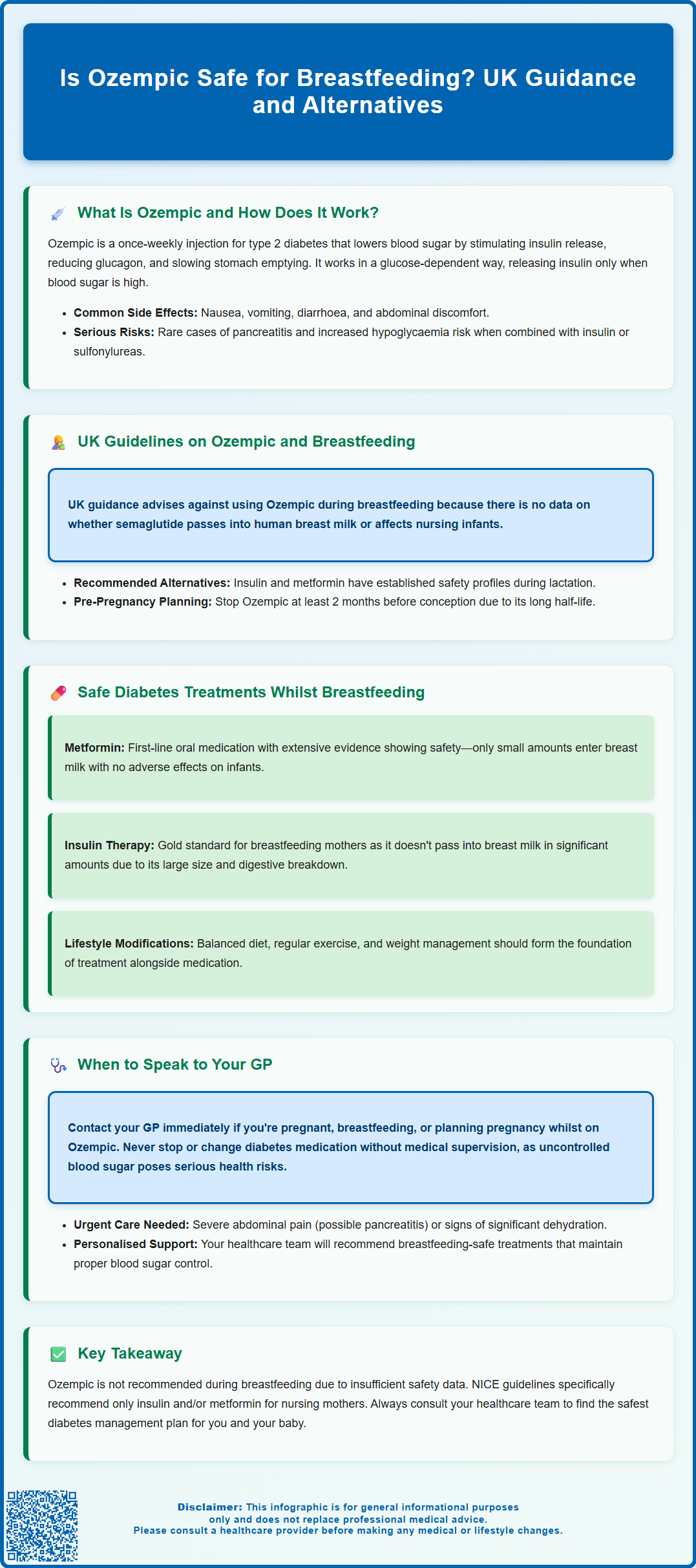
Current UK guidance on the use of Ozempic during breastfeeding is clear and cautious, reflecting the limited data available on the excretion of semaglutide into human breast milk and its potential effects on nursing infants.
The Medicines and Healthcare products Regulatory Agency (MHRA) and the Summary of Product Characteristics (SmPC) for Ozempic state that it is not known whether semaglutide is excreted in human milk. Due to this uncertainty, the manufacturer advises that Ozempic should not be used during breastfeeding. This precautionary stance is standard when robust safety data in lactating women are absent.
NICE guidance (NG3) on diabetes in pregnancy includes postnatal management recommendations, advising that insulin and/or metformin are the preferred options for breastfeeding mothers with diabetes, while other agents should generally be avoided. The British National Formulary (BNF) similarly advises avoiding Ozempic during breastfeeding due to insufficient evidence.
From a theoretical pharmacological perspective, semaglutide is a large peptide molecule with a molecular weight of approximately 4,100 Daltons. Larger molecules generally have reduced transfer into breast milk compared to smaller drugs, and peptides are often broken down in the infant's gastrointestinal tract, potentially limiting systemic absorption. However, these theoretical considerations do not override the regulatory guidance, and without clinical studies confirming safety, healthcare professionals must follow the SmPC recommendation.
It's also important to note that women planning pregnancy should discontinue Ozempic at least 2 months before a planned conception due to its long half-life. For breastfeeding mothers with type 2 diabetes, the priority is achieving safe and effective glycaemic control while minimising any risk to the infant. Women currently taking Ozempic who wish to breastfeed, or those who become pregnant while on treatment, should discuss their options with their GP or diabetes specialist well in advance to ensure a smooth and safe transition.
For breastfeeding mothers with type 2 diabetes, several well-established treatment options are considered safer alternatives to Ozempic, with more extensive evidence supporting their use during lactation.
Metformin is widely regarded as the first-line oral medication for type 2 diabetes and is generally considered compatible with breastfeeding. It is excreted into breast milk in small amounts, but numerous studies have shown no adverse effects in breastfed infants. Metformin works by reducing hepatic glucose production and improving insulin sensitivity, making it effective for glycaemic control without significant risk to the nursing baby. The BNF and UK Drugs in Lactation Advisory Service (UKDILAS) both support its use during lactation.
Insulin therapy remains the gold standard for managing diabetes in pregnancy and breastfeeding. Insulin does not pass into breast milk in clinically significant amounts due to its large molecular size and rapid degradation in the infant's digestive system. Both short-acting (e.g., insulin aspart, insulin lispro) and long-acting insulins (e.g., insulin detemir, insulin glargine) are considered safe. Many women with gestational diabetes or type 2 diabetes continue or initiate insulin therapy postpartum to maintain optimal blood sugar control while breastfeeding.
NICE guidance (NG3) specifically recommends insulin and/or metformin for breastfeeding mothers and advises avoiding other diabetes medications. Other GLP-1 receptor agonists and newer diabetes medications such as SGLT2 inhibitors (e.g., dapagliflozin, empagliflozin) should be avoided during breastfeeding as they lack sufficient safety data.
Lifestyle modifications—including a balanced diet, regular physical activity, and weight management—remain foundational and should be optimised alongside any pharmacological treatment. A multidisciplinary approach involving GPs, diabetes specialist nurses, and dietitians can help tailor a safe and effective management plan for breastfeeding mothers.
If you are currently taking Ozempic and are planning to breastfeed, are already breastfeeding, or have recently given birth, it is essential to speak to your GP or diabetes specialist as soon as possible. As Ozempic should not be used during breastfeeding according to the manufacturer's guidance, you will need to discuss alternative treatment options.
You should contact your GP if:
You are planning a pregnancy while taking Ozempic. The medication should be discontinued at least 2 months before a planned conception due to its long half-life.
You have just discovered you are pregnant while taking Ozempic, as this will require an immediate medication review.
You are currently breastfeeding and taking Ozempic, as you will need to switch to a safer alternative.
You have been advised to stop Ozempic and need guidance on alternative diabetes treatments that are safe during lactation.
You are experiencing difficulty controlling your blood sugar levels after switching medications, or if you notice symptoms such as excessive thirst, frequent urination, fatigue, or unexplained weight loss.
Your baby shows any unusual symptoms or feeding difficulties, and you are uncertain whether your medication could be a contributing factor.
Seek urgent medical attention if you experience severe, persistent abdominal pain (with or without vomiting), which could indicate pancreatitis, or if you have signs of significant dehydration.
Your GP or diabetes care team will conduct a thorough risk-benefit assessment, taking into account your glycaemic control, overall health, breastfeeding goals, and any other medications you may be taking. They will likely recommend switching to metformin or insulin, both of which have well-established safety profiles in breastfeeding mothers.
It is important never to stop or change your diabetes medication without medical advice, as uncontrolled blood sugar can pose serious health risks to you and may indirectly affect your ability to care for your baby. Your healthcare team is there to support you in making informed decisions that prioritise both maternal and infant wellbeing, ensuring you can breastfeed safely while maintaining optimal diabetes management.
No, Ozempic should not be used during breastfeeding according to UK guidance from the MHRA and manufacturer, as there is insufficient data on whether semaglutide passes into breast milk or affects nursing infants.
Metformin and insulin are considered safe and effective options for managing type 2 diabetes during breastfeeding, with extensive evidence supporting their use and recommendations from NICE and the BNF.
You should discuss stopping Ozempic with your GP or diabetes specialist as soon as you plan to conceive or breastfeed, ideally discontinuing at least 2 months before planned conception and switching to safer alternatives before delivery.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
Unordered list
Bold text
Emphasis
Superscript
Subscript