Metformin and Rybelsus (semaglutide) are both licensed for type 2 diabetes management in the UK, yet they differ significantly in their weight loss effects. Metformin, a biguanide, typically produces modest weight reduction through metabolic pathways, whilst Rybelsus, a GLP-1 receptor agonist, directly targets appetite regulation centres. Neither medication is currently licensed specifically for weight management in individuals without diabetes. Understanding how these medications work, their comparative efficacy, safety profiles, and NHS prescribing criteria is essential for patients and healthcare professionals considering their use in diabetes care where weight management is an important clinical consideration.
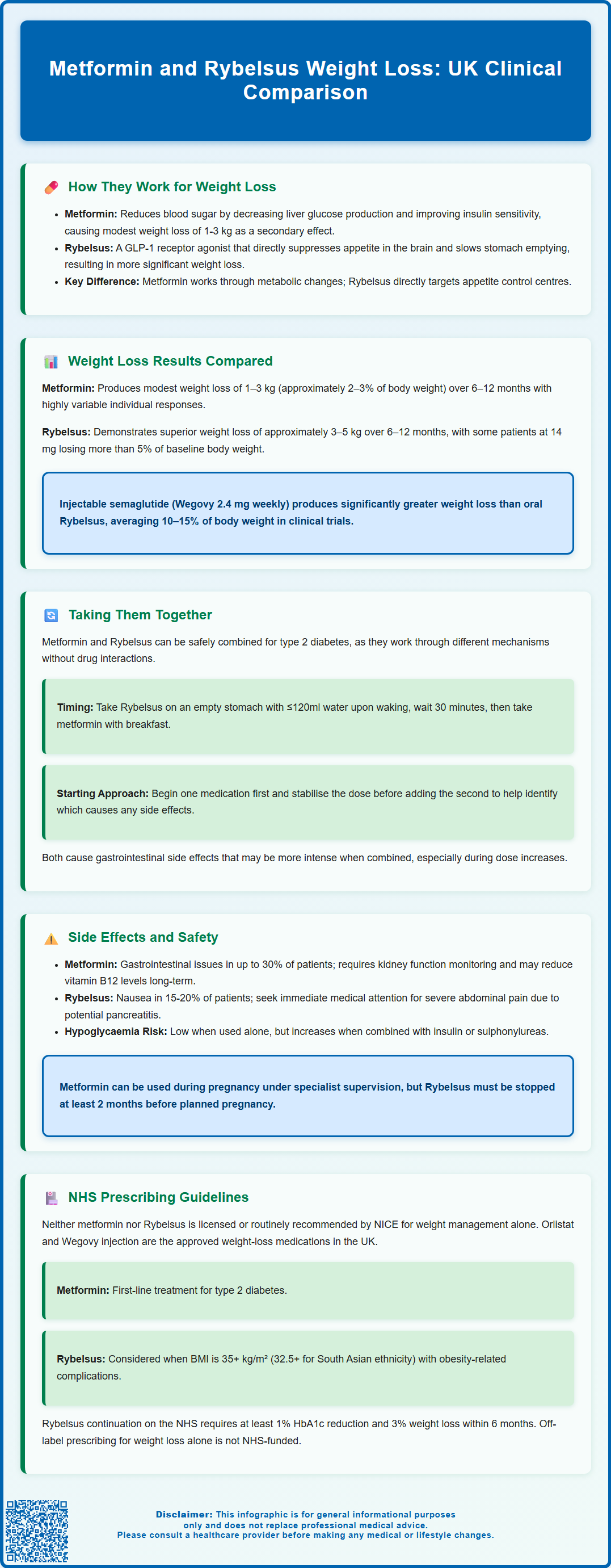
Summary: Metformin typically produces modest weight loss of 1–3 kg, whilst Rybelsus (oral semaglutide) demonstrates more substantial reductions of approximately 3–5 kg over 6–12 months in patients with type 2 diabetes.
- Metformin is a biguanide that reduces hepatic glucose production and improves insulin sensitivity, with weight loss as a secondary benefit.
- Rybelsus is a GLP-1 receptor agonist that directly targets appetite centres in the hypothalamus and slows gastric emptying.
- Combination therapy with metformin and Rybelsus is evidence-based for type 2 diabetes, with complementary mechanisms and no significant drug interactions.
- Both medications can cause gastrointestinal adverse effects; metformin requires renal function monitoring, whilst Rybelsus carries warnings regarding thyroid tumours and pancreatitis.
- Neither medication is licensed or routinely recommended by NICE for weight management in individuals without diabetes; prescribing follows type 2 diabetes guidelines (NICE NG28).
Table of Contents
How Metformin and Rybelsus Work for Weight Loss
Metformin is a biguanide medication primarily licensed for the treatment of type 2 diabetes mellitus. Its mechanism of action involves reducing hepatic glucose production, decreasing intestinal glucose absorption, and improving insulin sensitivity in peripheral tissues. Whilst weight loss is not its primary indication, metformin often produces modest weight reduction as a secondary benefit. This effect is hypothesised to occur through several pathways, potentially including effects on appetite, possible alterations in gut microbiota, and metabolic changes that may favour reduced caloric intake, though these mechanisms are not definitively established. Clinical studies typically demonstrate weight loss of approximately 1–3 kg over several months in patients with type 2 diabetes, though individual responses vary considerably.
Rybelsus (semaglutide) belongs to the glucagon-like peptide-1 (GLP-1) receptor agonist class and represents the first oral formulation of this drug type. Semaglutide works by mimicking the action of endogenous GLP-1, a hormone released from the intestine in response to food intake. It enhances glucose-dependent insulin secretion, suppresses inappropriate glucagon release, and slows gastric emptying. Crucially for weight management, GLP-1 receptor agonists act on appetite centres in the hypothalamus, producing significant reductions in hunger and food intake. Rybelsus is licensed in the UK for type 2 diabetes management and has demonstrated notable weight loss effects in clinical trials.
The weight loss mechanisms differ between these medications. Metformin primarily influences metabolic pathways and may modestly affect appetite, whereas Rybelsus directly targets appetite regulation centres and gastric motility. This distinction helps explain the more pronounced weight reduction typically observed with GLP-1 receptor agonists. Neither medication is currently licensed in the UK specifically for weight management in individuals without diabetes. In certain specialist settings, metformin may occasionally be considered for conditions such as polycystic ovary syndrome (PCOS) or prediabetes where weight management is clinically important, but this represents individualised care rather than routine practice. Patients should understand that these medications work best when combined with lifestyle modifications including dietary changes and increased physical activity.
Comparing Weight Loss Results: Metformin vs Rybelsus
Clinical trial evidence demonstrates differences in weight loss outcomes between metformin and Rybelsus. Metformin typically produces modest weight reduction, with meta-analyses suggesting an average loss of 1–3 kg over 6–12 months in patients with type 2 diabetes. Some individuals may experience greater benefits, particularly those with insulin resistance or polycystic ovary syndrome (PCOS), though responses remain highly variable. The Diabetes Prevention Programme trial showed that metformin reduced weight by approximately 2–3% of baseline body weight in individuals with prediabetes, which was less than lifestyle intervention alone.
Rybelsus (oral semaglutide) demonstrates more substantial weight loss effects. The PIONEER clinical trial programme evaluated Rybelsus at therapeutic doses (3 mg, 7 mg and 14 mg daily) in patients with type 2 diabetes. In these trials, Rybelsus showed superior weight loss compared to placebo and several active comparators including sitagliptin (a DPP-4 inhibitor), empagliflozin (an SGLT2 inhibitor), and liraglutide (an injectable GLP-1 receptor agonist). Weight reductions of approximately 3–5 kg were observed over 6–12 months, with variation across the different PIONEER studies. At the 14 mg dose, some participants experienced weight loss exceeding 5% of baseline body weight, though individual responses varied. Many participants in these trials were already taking metformin as background therapy.
It is important to note that higher-dose injectable semaglutide (Wegovy, 2.4 mg weekly) produces greater weight loss than oral Rybelsus, with the STEP trials showing average reductions of 10–15% of body weight. This formulation has specific NICE recommendations and eligibility criteria for weight management in the UK. Direct head-to-head comparisons between metformin monotherapy and Rybelsus specifically for weight loss are limited, as both medications are primarily studied and prescribed for glycaemic control in diabetes.
Patient characteristics significantly influence outcomes with both medications. Factors including baseline weight, dietary adherence, physical activity levels, genetic variations, and concurrent medications all affect individual responses. Healthcare professionals should set realistic expectations, emphasising that neither medication represents a standalone solution and that sustainable weight management requires comprehensive lifestyle modification alongside any pharmacological intervention.
Can You Take Metformin and Rybelsus Together?
Combination therapy with metformin and Rybelsus is not only possible but represents a common and evidence-based approach in type 2 diabetes management. The PIONEER clinical trial programme specifically evaluated semaglutide (Rybelsus) as add-on therapy to metformin, demonstrating both safety and enhanced efficacy for glycaemic control and weight management. There is no pharmacological contraindication to using these medications concurrently, as they work through complementary mechanisms without significant drug-drug interactions.
From a clinical perspective, combining metformin and Rybelsus may offer additive benefits for weight loss, though this combination is prescribed for diabetes management rather than weight loss alone. Metformin's effects on hepatic glucose production and insulin sensitivity complement Rybelsus's actions on appetite regulation, gastric emptying, and incretin pathways. Many patients with type 2 diabetes who achieve inadequate glycaemic control on metformin monotherapy will have a GLP-1 receptor agonist like Rybelsus added to their treatment regimen, in accordance with NICE guidance (NG28).
Practical considerations when taking both medications include timing and gastrointestinal tolerability. Rybelsus must be taken on an empty stomach with no more than 120 ml of water, waiting at least 30 minutes before eating, drinking, or taking other medications (including metformin). Metformin is typically taken with or after meals to minimise gastrointestinal side effects. Patients should establish a routine that accommodates these requirements—for example, taking Rybelsus upon waking and metformin with breakfast 30 minutes later.
Rybelsus requires careful dose titration: starting with 3 mg once daily for 30 days, then increasing to 7 mg once daily. After at least 30 days on the 7 mg dose, it may be increased to 14 mg once daily if needed for additional glycaemic control.
Both medications can cause gastrointestinal adverse effects, particularly nausea, diarrhoea, and abdominal discomfort. When used together, these effects may be more pronounced, especially during treatment initiation or dose escalation. Healthcare professionals typically recommend starting one medication and achieving stable dosing before introducing the second, allowing the body to adapt and making it easier to identify which medication may be causing any adverse effects. Patients experiencing persistent or severe gastrointestinal symptoms should contact their GP or diabetes specialist nurse for advice, as dose adjustments or alternative strategies may be necessary.
Side Effects and Safety Considerations
Metformin's side effect profile is well-established, with gastrointestinal disturbances representing the most common adverse effects. These include nausea, diarrhoea, abdominal pain, and metallic taste, affecting up to 30% of patients, particularly when treatment is initiated or doses increased. Using modified-release formulations and taking metformin with food can significantly reduce these symptoms. A rare but serious adverse effect is lactic acidosis, occurring predominantly in patients with renal impairment, severe dehydration, or acute illness. Metformin should be temporarily discontinued during acute illness or dehydration. For procedures involving iodinated contrast media, the approach depends on renal function and contrast administration route; metformin should be withheld before and for 48 hours after the procedure in higher-risk situations, with renal function reassessment before restarting. The MHRA recommends assessing renal function before starting metformin and monitoring it regularly, particularly in elderly patients or those with declining kidney function. Long-term use may reduce vitamin B12 absorption, and the MHRA advises considering periodic monitoring in at-risk patients and testing if symptoms of deficiency develop.
Rybelsus carries a different safety profile, with gastrointestinal effects again being most prominent. Nausea affects approximately 15–20% of patients, particularly during dose escalation, though this typically diminishes over time. Vomiting, diarrhoea, constipation, and reduced appetite are also common. Animal studies have shown thyroid C-cell tumours with semaglutide, though the relevance to humans is uncertain. Patients should report any symptoms such as a lump in the neck, persistent hoarseness, or difficulty swallowing. Acute pancreatitis has been reported with GLP-1 receptor agonists, and patients should seek immediate medical attention if they experience severe, persistent abdominal pain. Rybelsus may increase heart rate slightly, though GLP-1 receptor agonists generally have neutral or favourable cardiovascular profiles. Diabetic retinopathy complications may occur with rapid improvement in glucose control, particularly in patients with pre-existing retinopathy; appropriate ophthalmological monitoring should be considered. There is also an increased risk of gallbladder problems, including gallstones; patients should report symptoms such as right upper abdominal pain, fever, or jaundice.
Hypoglycaemia risk is generally low with both metformin and Rybelsus when used alone, as neither causes insulin release independent of glucose levels. However, when combined with insulin or sulfonylureas, hypoglycaemia risk increases, and dose adjustments of these other medications may be necessary. Patients should be educated about hypoglycaemia symptoms and management.
Patient safety advice includes staying well-hydrated, reporting persistent gastrointestinal symptoms, and seeking urgent medical attention for severe abdominal pain, signs of dehydration, or symptoms of lactic acidosis (muscle pain, breathing difficulties, unusual tiredness). Metformin may be continued or initiated during pregnancy under specialist supervision, whereas Rybelsus is not recommended during pregnancy and should be discontinued at least 2 months before a planned pregnancy. Women of childbearing potential should discuss contraception with their healthcare provider. Regular monitoring of renal function, HbA1c, and body weight is recommended, with medication review if weight loss plateaus or adverse effects become problematic.
Patients are encouraged to report suspected adverse reactions to any medicine via the MHRA Yellow Card Scheme.
NHS Prescribing Guidelines for Weight Management
NICE guidance for obesity (NG246) establishes a structured approach to weight management, with pharmacological interventions reserved for specific circumstances. Neither metformin nor Rybelsus is currently licensed or routinely recommended by NICE specifically for weight management in individuals without diabetes. The primary medications approved for weight management in the UK are orlistat (available over-the-counter and on prescription) and, more recently, higher-dose semaglutide injection (Wegovy) for specialist use in defined circumstances according to NICE Technology Appraisal guidance.
For type 2 diabetes management, NICE guideline NG28 provides clear recommendations. Metformin remains the first-line pharmacological treatment for most adults with type 2 diabetes, unless contraindicated. When additional therapy is required, NICE recommends considering a GLP-1 receptor agonist (such as Rybelsus) if the patient has a BMI of 35 kg/m² or higher (or 32.5 kg/m² or higher for people of South Asian or related ethnicity) and specific psychological or medical problems associated with obesity, or if BMI is lower but insulin therapy would have significant occupational implications or weight loss would benefit other obesity-related comorbidities.
Prescribing Rybelsus on the NHS requires meeting specific criteria. According to NICE NG28, GLP-1 receptor agonist treatment should only be continued if there is beneficial metabolic response (HbA1c reduction of at least 11 mmol/mol [1.0%] and weight loss of at least 3% of initial body weight at 6 months). This "continue or stop" rule ensures appropriate use of NHS resources and identifies patients who will benefit from ongoing treatment. Initiation of GLP-1 receptor agonists may occur in primary or secondary care depending on local formulary arrangements and shared care protocols.
Off-label prescribing of these medications purely for weight loss in individuals without diabetes is not supported by NHS England commissioning policies and would typically require private prescription. Some specialist weight management services may consider metformin for patients with prediabetes or PCOS where weight loss is clinically important, but this represents individualised care rather than routine practice.
Access considerations include cost differences between medications and NHS prioritisation frameworks. The NHS weight management pathway involves a tiered approach, with patients first accessing tier 1 and 2 services (lifestyle interventions, dietary advice, physical activity programmes) through their GP or local authority services. Specialist tier 3 weight management services assess suitability for pharmacological or surgical interventions in complex cases. Healthcare professionals must balance clinical benefit, cost-effectiveness, and equitable access when making prescribing decisions within NHS frameworks.
Frequently Asked Questions
Which produces greater weight loss, metformin or Rybelsus?
Rybelsus (oral semaglutide) typically produces greater weight loss than metformin, with clinical trials showing reductions of approximately 3–5 kg compared to metformin's 1–3 kg over 6–12 months in patients with type 2 diabetes. Individual responses vary considerably based on baseline characteristics and lifestyle factors.
Is it safe to take metformin and Rybelsus together?
Yes, combining metformin and Rybelsus is safe and represents common practice in type 2 diabetes management, with clinical trials demonstrating both safety and enhanced efficacy. The medications work through complementary mechanisms without significant drug interactions, though gastrointestinal side effects may be more pronounced when used together.
Can I get metformin or Rybelsus on the NHS for weight loss alone?
Neither metformin nor Rybelsus is licensed or routinely recommended by NICE specifically for weight management in individuals without diabetes. NHS prescribing follows type 2 diabetes guidelines (NICE NG28), with GLP-1 receptor agonists like Rybelsus reserved for patients meeting specific BMI and clinical criteria alongside inadequate glycaemic control on metformin.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












