Weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) have transformed obesity management in the UK, but many older adults wonder whether age restricts their eligibility. There is no absolute upper age limit for weight loss injections specified in UK product licences, though clinical experience in those aged 75 and over remains limited. Prescribing decisions for older patients must be individualised, considering factors such as frailty, comorbidities, nutritional status, and potential benefits versus risks. This article examines age-related eligibility criteria, safety considerations, NHS guidance, and alternative weight management options for older adults seeking these treatments.
Summary: There is no absolute upper age limit for weight loss injections in the UK, but clinical experience in patients aged 75 and over is limited and prescribing requires individualised assessment.
- GLP-1 receptor agonists like semaglutide and liraglutide have no specified upper age cut-off in UK product licences.
- Clinical trials underrepresented adults over 75, meaning safety and efficacy data are limited in this age group.
- Prescribing decisions should consider frailty, comorbidities, nutritional status, and functional capacity rather than chronological age alone.
- Older adults face increased risks including gastrointestinal side effects, dehydration, sarcopenia, and drug interactions with polypharmacy.
- NICE recommends semaglutide as part of specialist weight management services with no upper age restriction but emphasises individualised clinical appropriateness.
- Comprehensive geriatric assessment and shared decision-making are essential when considering weight loss injections for older patients.
Table of Contents
- Understanding Weight Loss Injections and Age Eligibility
- Is There an Upper Age Limit for Weight Loss Injections?
- Safety Considerations for Older Adults Using Weight Loss Injections
- NHS and NICE Guidance on Prescribing Weight Loss Injections by Age
- Alternative Weight Management Options for Older Adults
- Scientific References
- Frequently Asked Questions
Understanding Weight Loss Injections and Age Eligibility
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy), liraglutide (Saxenda), and the newer tirzepatide (Zepbound), have become increasingly prominent in the management of obesity in the United Kingdom. These medications work by mimicking naturally occurring hormones that regulate appetite and glucose metabolism, leading to reduced food intake and subsequent weight reduction. The mechanism involves slowing gastric emptying, enhancing satiety signals to the brain, and improving insulin secretion in response to meals.
In the UK, according to their Summary of Product Characteristics (SmPCs), these medications are licensed for adults with a body mass index (BMI) of 30 kg/m² or above, or 27 kg/m² or above in the presence of weight-related comorbidities such as type 2 diabetes, hypertension, or obstructive sleep apnoea. However, NHS access is governed by stricter NICE criteria. It's important to note that lower BMI thresholds (typically 2.5 kg/m² lower) apply for some minority ethnic groups who are at increased risk at lower BMI levels.
Regarding age eligibility, Wegovy and Zepbound are licensed only for adults (18 years and over), while Saxenda is licensed for adults and also for adolescents aged 12-17 years with obesity and body weight above 60 kg. The upper age limit is less straightforward. The decision to prescribe weight loss injections to older adults involves careful assessment of individual health status, comorbidities, frailty, and potential benefits versus risks. Healthcare professionals must consider whether weight loss will meaningfully improve health outcomes and quality of life in older patients, taking into account their overall clinical picture and life expectancy.
All these medications are contraindicated during pregnancy and breastfeeding, and women of childbearing potential should use effective contraception while on treatment.
Is There an Upper Age Limit for Weight Loss Injections?
There is no absolute upper age limit specified in the product licences for GLP-1 receptor agonist weight loss injections in the United Kingdom. The Medicines and Healthcare products Regulatory Agency (MHRA) approved formulations do not explicitly prohibit use based solely on chronological age, and no dose adjustment is required based on age alone. However, the Summary of Product Characteristics for these medications typically notes that clinical experience in patients aged 75 years and older is limited, and caution is advised in this population.
For example, the Wegovy SmPC states: "No dose adjustment is required based on age. Therapeutic experience in patients ≥75 years of age is limited and a higher risk of general adverse reactions cannot be excluded." Similar statements appear in the Saxenda and Zepbound SmPCs.
Clinical trials that led to the licensing of semaglutide and liraglutide for weight management included participants across a broad age range, though older adults, particularly those over 75 years, were underrepresented. This means that whilst there is no official upper age cut-off, the evidence base for safety and efficacy diminishes with advancing age. Prescribers must therefore exercise clinical judgement when considering these treatments for older patients, weighing the potential benefits against the increased risk of adverse effects and complications.
The decision to prescribe weight loss injections to older adults should be individualised rather than based on age alone. Factors such as functional status, frailty, nutritional state, comorbidities, polypharmacy, and the patient's goals of care are more relevant than chronological age. A fit and healthy 70-year-old with obesity-related complications may be an appropriate candidate, whereas a frail 68-year-old with multiple comorbidities and poor nutritional status may not benefit and could potentially experience harm. Healthcare professionals should conduct comprehensive geriatric assessments where appropriate to inform prescribing decisions in older adults seeking weight loss injections, documenting frailty scores (e.g., Clinical Frailty Scale) and nutritional status as part of the assessment.
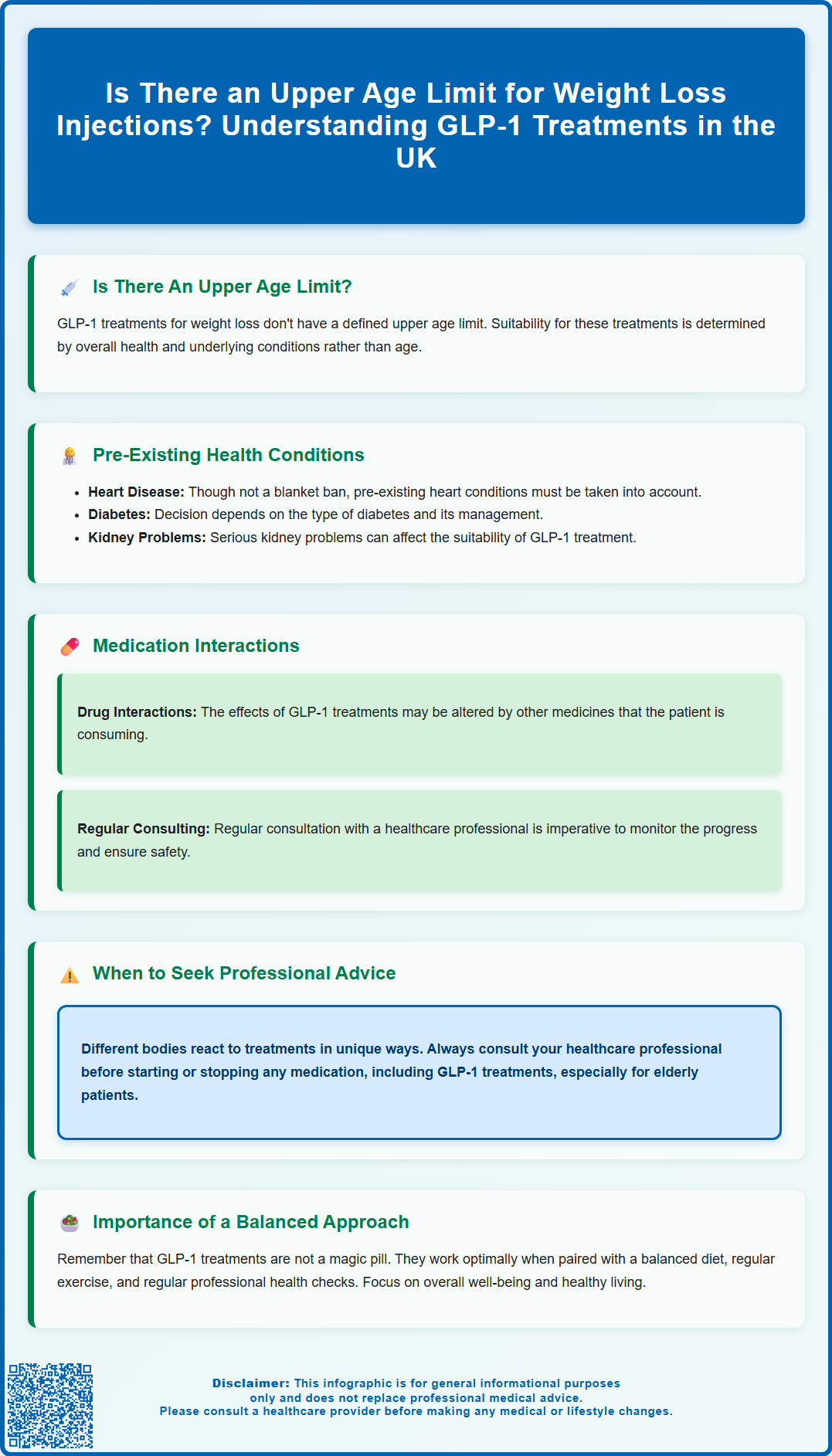
Safety Considerations for Older Adults Using Weight Loss Injections
Older adults face distinct safety considerations when using weight loss injections due to age-related physiological changes and increased vulnerability to adverse effects. Gastrointestinal side effects, including nausea, vomiting, diarrhoea, and constipation, are common with GLP-1 receptor agonists and may be poorly tolerated in older patients. These symptoms can lead to reduced oral intake, dehydration, and electrolyte imbalances, which pose greater risks in this age group. Older adults may also have reduced thirst perception and kidney function, making them more susceptible to dehydration-related complications.
Sarcopenia, the age-related loss of muscle mass and strength, represents a significant concern when prescribing weight loss medications to older adults. Rapid or excessive weight loss can accelerate muscle loss, potentially worsening functional decline and increasing fall risk. This is particularly problematic in individuals who are already frail or have limited mobility. Healthcare professionals should emphasise the importance of adequate protein intake and resistance exercise alongside any weight loss intervention to preserve lean body mass.
Older adults are more likely to be taking multiple medications, increasing the risk of drug interactions. GLP-1 receptor agonists can delay gastric emptying, potentially affecting the absorption of oral medications. However, according to the SmPCs, clinically significant effects are unlikely for most oral drugs. Particular vigilance is advised with medications that have a narrow therapeutic index (such as warfarin, where INR monitoring may be prudent) or those requiring rapid absorption. Patients with type 2 diabetes taking concurrent glucose-lowering medications, especially insulin or sulphonylureas, face increased hypoglycaemia risk, which can be particularly dangerous in older adults. Regular medication reviews and dose adjustments are essential.
For patients with type 2 diabetes using semaglutide, there is a caution regarding diabetic retinopathy complications, particularly if rapid improvement in glucose control occurs. Appropriate eye monitoring should be considered. Regarding renal function, while no dose adjustment is generally required, there is limited data in severe impairment, and renal function should be monitored, especially with significant gastrointestinal side effects.
Patients should be advised to contact their GP urgently if they experience severe abdominal pain, persistent vomiting (signs of pancreatitis), or symptoms of gallbladder disease, as these complications may present atypically in older populations.
NHS and NICE Guidance on Prescribing Weight Loss Injections by Age
The National Institute for Health and Care Excellence (NICE) provides guidance on obesity management in adults, including Technology Appraisal TA875 on semaglutide for managing overweight and obesity. NICE guidance does not specify an upper age limit for weight loss injections but emphasises that treatment decisions should be based on clinical appropriateness and individual patient circumstances.
NICE recommends that semaglutide (Wegovy) should be considered for adults with a BMI of 35 kg/m² or more, or between 30 and 34.9 kg/m² in the presence of at least one weight-related comorbidity, and who have tried standard care without achieving or maintaining adequate weight loss. Lower BMI thresholds (typically 2.5 kg/m² lower) apply for people from some minority ethnic groups. Importantly, NICE specifies that Wegovy should only be prescribed as part of a specialist weight management service (Tier 3), with ongoing support for diet, physical activity, and behavioural change, and treatment should be limited to a maximum of 2 years.
It's worth noting that liraglutide (Saxenda) is not currently recommended by NICE for routine NHS commissioning for weight management, though it may be available through local funding arrangements. Tirzepatide (Zepbound) is newly authorised but does not yet have a NICE recommendation for weight management.
For older adults, clinicians must consider whether weight loss will provide meaningful clinical benefit. In some cases, particularly in very elderly or frail patients, the risks of weight loss may outweigh potential benefits, and weight maintenance or modest weight reduction through less intensive interventions may be more appropriate.
Regarding treatment continuation, the SmPCs provide specific stop rules. Treatment may be discontinued (or should be considered for discontinuation) if < 5 % weight loss after approximately 20 weeks on 2.4 mg, in line with SmPC guidance. For Saxenda, treatment should be discontinued if patients have not lost at least 5% of their initial body weight after 12 weeks on the full dose (3.0 mg daily). NHS England commissioning guidance for specialist weight management services acknowledges that treatment plans should be individualised and that certain populations, including older adults with frailty or significant comorbidities, may require modified approaches. Shared decision-making is paramount, ensuring that older patients understand the potential benefits, risks, and alternatives to weight loss injections.
Alternative Weight Management Options for Older Adults
For older adults who are not suitable candidates for weight loss injections or who prefer alternative approaches, several evidence-based weight management strategies exist. Dietary modification remains a cornerstone of obesity management across all age groups, though approaches may need tailoring for older adults. Rather than aggressive calorie restriction, which risks malnutrition and muscle loss, a moderate energy deficit of 500-600 calories per day is generally recommended. Emphasis should be placed on nutrient-dense foods with adequate protein intake (1.0-1.2 grams per kilogram body weight daily) to preserve muscle mass during weight loss. For patients with chronic kidney disease or hepatic impairment, protein targets should be individualised with dietitian input.
Physical activity programmes designed for older adults can support weight management whilst improving strength, balance, and functional capacity. The UK Chief Medical Officers' Physical Activity Guidelines recommend that adults should aim for at least 150 minutes of moderate-intensity aerobic activity weekly, alongside muscle-strengthening activities on two or more days. For older adults, this might include walking, swimming, chair-based exercises, or tai chi, adapted to individual capabilities. Resistance training is particularly important to counteract sarcopenia and should be incorporated where possible under appropriate supervision.
Behavioural interventions, including cognitive behavioural therapy approaches, can help older adults identify and modify eating patterns, manage emotional eating, and set realistic goals. Group-based weight management programmes may provide additional social support and motivation. For some older adults with severe obesity and suitable health status, bariatric surgery may be considered according to NICE guideline CG189 criteria, though age-related surgical risks must be carefully evaluated.
Orlistat, a lipase inhibitor that reduces fat absorption, represents an alternative pharmacological option for adults with a BMI ≥30 kg/m² or ≥28 kg/m² with risk factors. Treatment should be discontinued if less than 5% of body weight is lost after 3 months. Gastrointestinal side effects can be troublesome and may be particularly problematic for older adults.
Healthcare professionals should also address underlying factors contributing to weight gain in older adults, including reduced mobility, medication side effects (such as from corticosteroids or certain antidepressants), and psychosocial factors like bereavement or social isolation. A holistic, multidisciplinary approach involving dietitians, physiotherapists, occupational therapists, and mental health professionals may be beneficial. Ultimately, the goal for older adults should focus on optimising health, function, and quality of life rather than achieving arbitrary weight targets, recognising that modest weight loss or weight stabilisation may represent successful outcomes in this population.
Scientific References
- Wegovy 0.25 mg, FlexTouch solution for injection in pre-filled pen - Summary of Product Characteristics (SmPC).
- Saxenda 6 mg/mL solution for injection in pre-filled pen - Summary of Product Characteristics (SmPC).
- Medicines containing the active ingredient tirzepatide.
- Semaglutide for managing overweight and obesity. Technology appraisal guidance TA875.
- Obesity: identification, assessment and management. Clinical guideline CG189.
Frequently Asked Questions
Can people over 75 use weight loss injections in the UK?
Yes, people over 75 can use weight loss injections, but clinical experience in this age group is limited and prescribing requires careful individual assessment of health status, frailty, and potential risks versus benefits.
What safety concerns exist for older adults using weight loss injections?
Older adults face increased risks including gastrointestinal side effects leading to dehydration, accelerated muscle loss (sarcopenia), drug interactions with multiple medications, and hypoglycaemia risk if taking diabetes medications.
Does the NHS restrict weight loss injections based on age?
No, NHS and NICE guidance do not specify an upper age limit, but treatment decisions must be clinically appropriate and individualised, considering whether weight loss will meaningfully improve health outcomes and quality of life.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












