Weight loss injections such as semaglutide and liraglutide have gained prominence for obesity management, but their use in people with heart failure requires careful consideration. Heart failure is a chronic condition affecting the heart's ability to pump blood effectively, and many patients also experience obesity, which can worsen cardiac function. Whilst emerging evidence suggests certain GLP-1 receptor agonists may benefit selected heart failure patients—particularly those with preserved ejection fraction—safety concerns including heart rate changes, fluid balance, and medication interactions necessitate individualised assessment. This article examines whether weight loss injections can be used safely in heart failure, the cardiovascular risks involved, alternative weight management strategies, and when to seek medical guidance.
Summary: Weight loss injections may be used cautiously in selected heart failure patients depending on heart failure type, severity, and individual clinical factors, but require specialist assessment and close monitoring.
- GLP-1 receptor agonists such as semaglutide and liraglutide work by mimicking natural hormones that regulate appetite and blood glucose levels.
- Emerging evidence suggests potential benefits in heart failure with preserved ejection fraction (HFpEF), whilst evidence in reduced ejection fraction (HFrEF) remains limited.
- These medications can cause heart rate increases, gastrointestinal side effects leading to dehydration, and potential interactions with heart failure medications including diuretics.
- Patients with severe heart failure (NYHA Class IV) or unstable cardiac conditions should generally avoid these injections until their condition stabilises.
- Regular monitoring of renal function, electrolytes, blood pressure, and heart failure symptoms is essential during treatment.
- NICE guidance emphasises that specialist cardiology input is required when considering weight loss injections in patients with significant cardiovascular disease.
Table of Contents
Understanding Weight Loss Injections and Heart Failure
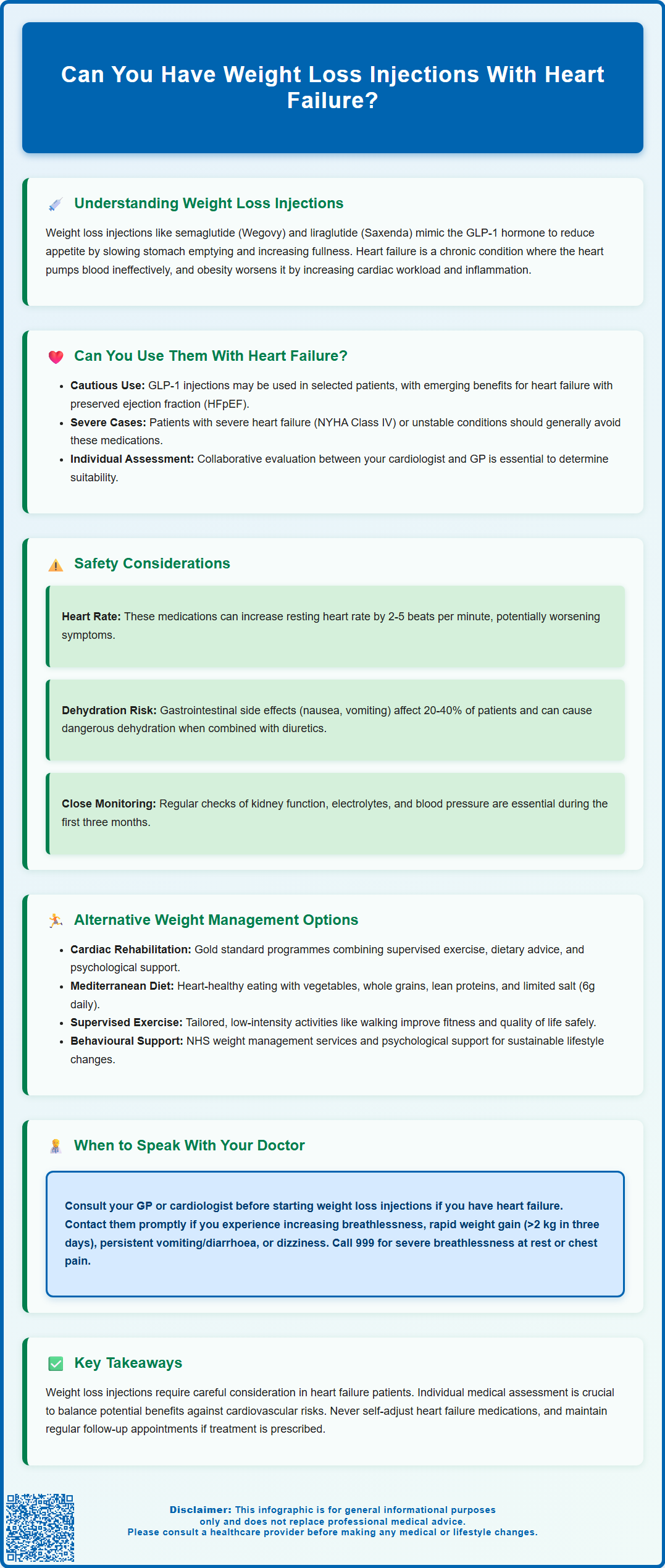
Weight loss injections, primarily glucagon-like peptide-1 receptor agonists (GLP-1 RAs) such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly popular for managing obesity. These medications work by mimicking the action of the naturally occurring hormone GLP-1, which regulates appetite and blood glucose levels. By binding to GLP-1 receptors in the brain, pancreas, and gastrointestinal tract, these injections slow gastric emptying, enhance feelings of fullness, and reduce hunger signals. This mechanism typically results in significant weight reduction when combined with lifestyle modifications.
Heart failure is a chronic condition where the heart cannot pump blood effectively to meet the body's needs. It affects a significant number of people in the UK and is classified by the New York Heart Association (NYHA) into four functional classes based on symptom severity. Heart failure is typically categorised as either heart failure with reduced ejection fraction (HFrEF) or heart failure with preserved ejection fraction (HFpEF), which has implications for treatment approaches. Common symptoms include breathlessness, fatigue, ankle swelling, and reduced exercise tolerance. Heart failure patients often experience comorbidities including obesity, type 2 diabetes, and hypertension, which can worsen cardiac function and prognosis.
The intersection of obesity and heart failure is clinically significant. Excess weight increases cardiac workload, promotes inflammation, and contributes to metabolic dysfunction. However, managing weight in heart failure patients requires careful consideration, as rapid or excessive weight loss can be detrimental, and certain medications may affect cardiovascular function. Importantly, unintentional weight loss in heart failure patients (cardiac cachexia) is a concerning sign that requires prompt medical evaluation. The decision to use weight loss injections in this population must balance potential metabolic benefits against cardiovascular safety concerns, making individualised assessment essential.
Can You Have Weight Loss Injections With Heart Failure?
The answer depends on several factors, including the type and severity of your heart failure, the specific weight loss injection being considered, and your overall clinical picture. Current evidence suggests that some GLP-1 receptor agonists may be used cautiously in selected heart failure patients, whilst others require more careful evaluation.
Recent cardiovascular outcome trials have provided reassuring data for certain GLP-1 RAs. The SELECT trial demonstrated that semaglutide reduced major adverse cardiovascular events in people with established cardiovascular disease and obesity, though this study included relatively few patients with symptomatic heart failure. For patients with heart failure with preserved ejection fraction (HFpEF), emerging evidence from the STEP-HFpEF trials suggests semaglutide may improve symptoms, physical function, and quality of life whilst promoting weight loss. However, evidence in heart failure with reduced ejection fraction (HFrEF) is more limited and mixed, with some studies showing no benefit or potential safety concerns.
Important contraindications and precautions exist. Patients with severe heart failure (NYHA Class IV) or those with unstable cardiac conditions should generally avoid initiating weight loss injections until their condition stabilises. These medications should not be used during pregnancy or breastfeeding. People with a history of pancreatitis, gallbladder disease, or severe gastrointestinal disorders require careful assessment. For people with diabetes, there is a risk of worsening diabetic retinopathy, particularly with rapid improvements in blood glucose control.
In the UK, the MHRA has licensed semaglutide and liraglutide for weight management in adults with specific BMI thresholds. However, NHS access through NICE guidance (TA875 for semaglutide, TA664 for liraglutide) is more restricted, requiring referral to specialist weight management services, with specific BMI criteria and time-limited treatment courses. NICE guidance emphasises that specialist input is essential when considering these medications in patients with significant cardiovascular disease, including heart failure. Your cardiologist and GP should work collaboratively to determine whether weight loss injections are appropriate for your specific circumstances.
Cardiovascular Risks and Safety Considerations
When considering weight loss injections in heart failure patients, several cardiovascular safety considerations require careful evaluation. Heart rate changes represent one concern: GLP-1 receptor agonists typically cause a modest increase in resting heart rate (approximately 2-5 beats per minute according to product information). Whilst this is generally well-tolerated in most patients, those with heart failure—particularly those with reduced ejection fraction—may be more sensitive to tachycardia, which can increase myocardial oxygen demand and potentially worsen symptoms.
Fluid balance and dehydration pose significant risks. The gastrointestinal side effects of GLP-1 RAs, including nausea, vomiting, and diarrhoea, occur in approximately 20-40% of patients according to clinical trials, particularly during dose escalation. In heart failure patients taking diuretics or SGLT2 inhibitors (commonly used in heart failure), these effects can precipitate dehydration, electrolyte imbalances (especially hypokalaemia and hyponatraemia), and acute kidney injury. Such complications may destabilise previously controlled heart failure and necessitate hospital admission.
Patients should be monitored for:
-
Worsening breathlessness or ankle swelling (signs of fluid retention or heart failure decompensation)
-
Dizziness or postural hypotension (particularly if taking multiple blood pressure medications)
-
Rapid weight changes (may indicate fluid shifts rather than fat loss in heart failure patients)
-
Palpitations or irregular heartbeat
-
Severe, persistent abdominal pain with or without vomiting (possible pancreatitis requiring urgent assessment)
-
Symptoms of gallstones (right upper abdominal pain, nausea)
-
Visual changes (for people with diabetes, especially those with pre-existing retinopathy)
Regular monitoring of renal function, electrolytes, and blood pressure is essential, particularly during the first three months of treatment. Heart failure patients should maintain adequate hydration and report persistent gastrointestinal symptoms promptly. Importantly, patients should not self-adjust their heart failure medications (diuretics, ACE inhibitors, angiotensin receptor blockers, etc.) without clinical guidance, even if experiencing side effects. For people with diabetes also taking insulin or sulfonylureas, dose adjustments may be needed to prevent hypoglycaemia. Any suspected side effects should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Alternative Weight Management Options for Heart Failure Patients
For heart failure patients who cannot safely use weight loss injections, or who prefer alternative approaches, several evidence-based weight management strategies exist. Cardiac rehabilitation programmes represent the gold standard for heart failure patients seeking to improve fitness and manage weight. These supervised, multidisciplinary programmes combine tailored exercise training, dietary advice, psychological support, and medication optimisation. NICE recommends offering cardiac rehabilitation to all heart failure patients (NG106), as it improves exercise capacity, quality of life, and reduces hospital admissions.
Dietary modifications specifically designed for heart failure are crucial. A heart-healthy diet emphasising vegetables, fruits, whole grains, lean proteins, and healthy fats can promote gradual weight loss whilst supporting cardiac function. The Mediterranean diet pattern has strong evidence for cardiovascular benefits. Heart failure patients should aim for a low-salt diet and not exceed 6g of salt per day (approximately 2.4g sodium) unless otherwise advised by their heart failure team. A registered dietitian with cardiology expertise can provide personalised guidance balancing weight loss goals with cardiac nutritional needs.
Structured exercise programmes adapted to individual functional capacity offer significant benefits. Even patients with moderate heart failure can safely engage in supervised aerobic exercise and resistance training, which improves exercise capacity, symptoms, and quality of life. Starting with low-intensity activities such as walking and gradually progressing under professional guidance optimises safety and adherence.
Other options include:
-
NHS-commissioned behavioural weight management services (tier 2 or tier 3 services, available through local referral pathways)
-
Orlistat (a lipase inhibitor that may be considered, though gastrointestinal side effects, potential malabsorption of fat-soluble vitamins, and interactions with medications like warfarin require careful evaluation)
-
Psychological support for emotional eating or depression, which commonly coexists with heart failure
For patients with severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities, or BMI 30-34.9 kg/m² with recent-onset type 2 diabetes) who have not responded to conservative measures, bariatric surgery may be considered following specialist multidisciplinary assessment, though thorough cardiac risk stratification and long-term follow-up are essential.
When to Speak With Your GP or Cardiologist
If you have heart failure and are considering weight loss injections, consultation with your healthcare team is essential before starting treatment. You should arrange an appointment with your GP or cardiologist to discuss whether these medications are appropriate for your specific situation. This is particularly important if you have been diagnosed with heart failure within the past six months, have recently experienced worsening symptoms, or have other significant medical conditions.
You should contact your GP or heart failure nurse promptly if you experience any of the following whilst taking weight loss injections:
-
Increasing breathlessness, especially when lying flat or during minimal exertion
-
Rapid weight gain (>2 kg in three days) or new or worsening ankle/leg swelling
-
Persistent nausea, vomiting, or diarrhoea lasting more than 24-48 hours
-
Dizziness, light-headedness, or fainting episodes
-
Chest pain, palpitations, or irregular heartbeat
-
Reduced urine output or dark-coloured urine
-
Extreme fatigue or weakness beyond your usual baseline
-
Severe, persistent abdominal pain with or without vomiting (possible pancreatitis)
-
Right upper abdominal pain or symptoms suggestive of gallstones
-
New or worsening visual symptoms if you have diabetes
Seek immediate medical attention (call 999 or attend A&E) if you develop severe breathlessness at rest, chest pain that doesn't resolve, or signs of severe dehydration such as confusion, very low urine output, or collapse.
Before your appointment, prepare by:
-
Listing all current medications including doses
-
Recording recent weight measurements and any symptom changes
-
Noting your typical exercise tolerance and any limitations
-
Writing down questions about weight management options
Your healthcare team can assess your heart failure severity, review your medication regimen, evaluate potential drug interactions, and determine the safest approach to weight management for your individual circumstances. Regular follow-up appointments are necessary if weight loss injections are prescribed, with frequency determined by your clinical needs and the medication's dosing schedule. Do not stop or change your heart failure medications without clinical advice, even if experiencing side effects from weight loss injections. Collaborative care between your GP, cardiologist, and heart failure specialist nurse ensures optimal safety and outcomes.
Frequently Asked Questions
Are GLP-1 weight loss injections safe for all heart failure patients?
No, safety depends on heart failure type and severity. Patients with severe heart failure (NYHA Class IV) or unstable cardiac conditions should generally avoid these medications, whilst those with preserved ejection fraction may benefit under specialist supervision.
What side effects should heart failure patients watch for when taking weight loss injections?
Heart failure patients should monitor for worsening breathlessness, ankle swelling, rapid weight changes, dizziness, palpitations, persistent gastrointestinal symptoms causing dehydration, and severe abdominal pain. Any concerning symptoms require prompt medical review.
What are the alternatives to weight loss injections for heart failure patients?
Alternatives include cardiac rehabilitation programmes, heart-healthy dietary modifications (such as Mediterranean diet patterns with salt restriction), supervised exercise training, NHS behavioural weight management services, and in selected cases, bariatric surgery following specialist assessment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript