Weight loss injections, such as semaglutide (Wegovy) and liraglutide (Saxenda), are increasingly prescribed for obesity management in the UK. However, these glucagon-like peptide-1 (GLP-1) receptor agonists are not suitable for everyone. Certain medical conditions, medications, and patient characteristics may preclude their use or require specialist assessment. Understanding who cannot take weight loss injections is essential for safe prescribing and optimal patient outcomes. This article outlines the key contraindications, precautions, and safety considerations to help patients and healthcare professionals make informed decisions about treatment suitability.
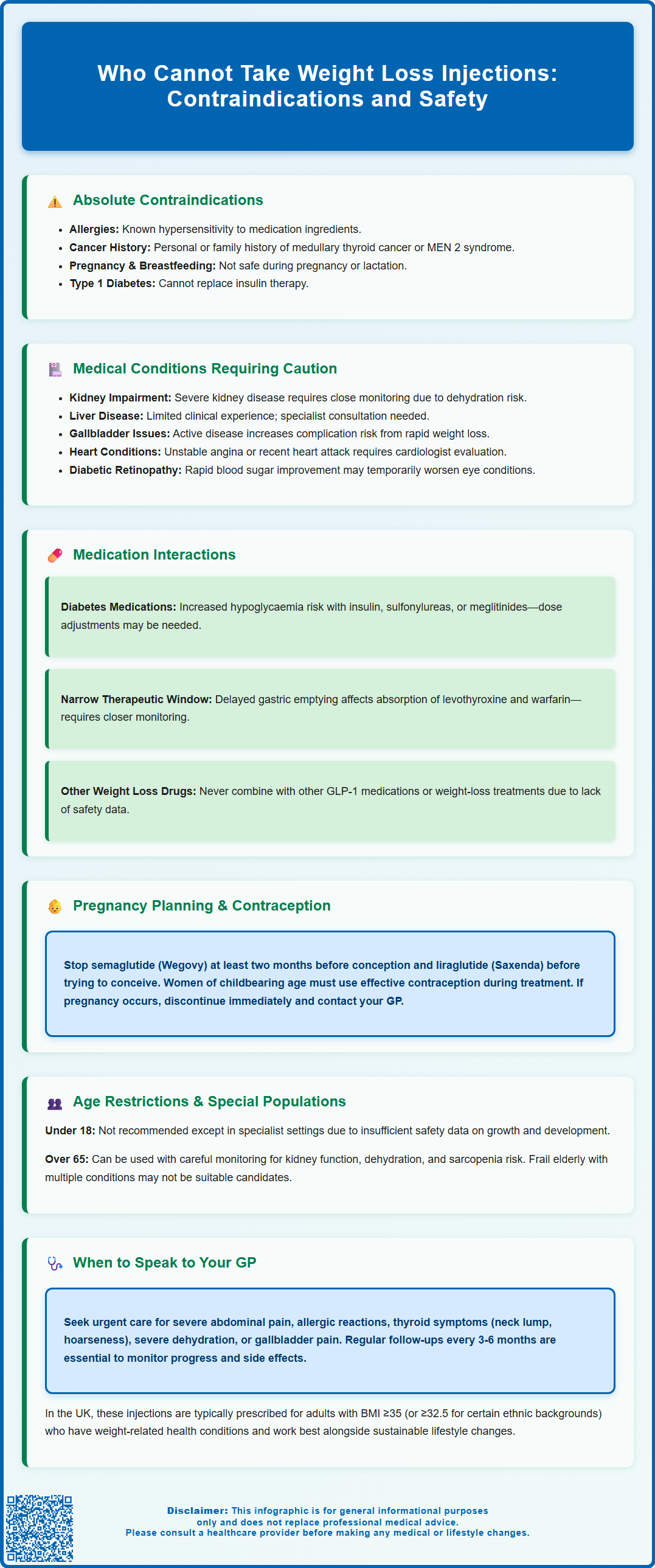
Summary: Weight loss injections such as semaglutide and liraglutide are contraindicated in individuals with hypersensitivity to the medication, personal or family history of medullary thyroid carcinoma or MEN 2, type 1 diabetes, and during pregnancy or breastfeeding.
- GLP-1 receptor agonists should not be used by people with type 1 diabetes, as they are not a substitute for insulin therapy.
- Patients with severe renal or hepatic impairment require careful assessment and specialist input before treatment initiation.
- Concurrent use with insulin or sulfonylureas increases hypoglycaemia risk and may require dose adjustments of these medications.
- Treatment must be discontinued at least two months before planned pregnancy for semaglutide and is not recommended during breastfeeding.
- Individuals with active gallbladder disease, severe gastroparesis, or unstable cardiovascular conditions require individualised risk assessment.
- Regular GP monitoring is essential to assess treatment response, manage side effects, and ensure ongoing suitability for therapy.
Table of Contents
- Who Cannot Take Weight Loss Injections
- Medical Conditions That Prevent Use of Weight Loss Injections
- Medications That Interact With Weight Loss Injections
- Pregnancy, Breastfeeding and Weight Loss Injections
- Age Restrictions and Safety Considerations
- When to Speak to Your GP About Weight Loss Injections
- Frequently Asked Questions
Who Cannot Take Weight Loss Injections
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for weight management in the UK. However, these medications are not suitable for everyone. Understanding who cannot take these injections is essential for patient safety and treatment efficacy.
These medications should not be used by individuals with hypersensitivity to the active ingredient or any excipients, which may cause severe allergic reactions (anaphylaxis or angioedema). Weight loss injections should not be used during pregnancy or breastfeeding.
Patients with a personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN 2) should discuss these conditions with their healthcare provider, as GLP-1 receptor agonists have been associated with thyroid C-cell tumours in animal studies. Your doctor will advise you to be vigilant for symptoms such as a lump in the neck, persistent hoarseness, or difficulty swallowing.
Weight loss injections are not appropriate for people with type 1 diabetes, as these medications are specifically designed for type 2 diabetes and obesity management. They should not be used as a substitute for insulin therapy. Individuals with diabetic ketoacidosis or those in a hyperosmolar hyperglycaemic state require immediate medical intervention rather than weight management treatment.
Certain patient groups require careful assessment before initiation. Those with severe gastroparesis may experience worsening symptoms due to the medications' effects on gastric emptying. Liraglutide is not recommended for people with inflammatory bowel disease due to limited clinical experience. People with a history of pancreatitis should be evaluated thoroughly, as there is ongoing discussion regarding potential links between GLP-1 receptor agonists and pancreatic inflammation, though evidence remains inconclusive. Your prescriber will conduct a comprehensive medical assessment to determine suitability before recommending weight loss injections.
Medical Conditions That Prevent Use of Weight Loss Injections
Several medical conditions may preclude the use of weight loss injections or require significant caution and specialist input. Severe renal impairment represents an important consideration. While no routine dose adjustment is required for semaglutide or liraglutide, caution is advised in patients with severe renal impairment or end-stage renal disease. Monitoring of renal function is particularly important if gastrointestinal side effects lead to dehydration.
Hepatic impairment also warrants caution. Whilst mild to moderate liver disease may not require dose adjustments, there is limited clinical experience with severe hepatic dysfunction. Patients with severe liver impairment should be assessed by a specialist before considering these medications.
Individuals with active or recent gallbladder disease, including cholecystitis or cholelithiasis, may be at increased risk of complications. Rapid weight loss is associated with an increased risk of gallstone formation. Patients should be advised to seek prompt medical attention if they develop symptoms such as right upper abdominal pain, particularly after eating, accompanied by nausea or fever.
Cardiovascular conditions require individualised assessment. Whilst some GLP-1 receptor agonists have demonstrated cardiovascular benefits in clinical trials, patients with unstable angina, recent myocardial infarction, or severe heart failure should be evaluated by a cardiologist. The medication's effects on heart rate and potential for dehydration necessitate careful monitoring in vulnerable cardiac patients.
People with diabetes and a history of retinopathy, particularly proliferative diabetic retinopathy, should be monitored closely, as rapid glucose reduction may temporarily worsen retinal conditions. This is particularly relevant for patients on insulin therapy experiencing significant improvements in glycaemic control.
Medications That Interact With Weight Loss Injections
Weight loss injections can interact with various medications, potentially altering their efficacy or increasing adverse effect risks. Understanding these interactions is crucial for safe prescribing and patient management.
Insulin and oral hypoglycaemic agents represent the most clinically significant interaction. When GLP-1 receptor agonists are used alongside insulin, sulfonylureas (such as gliclazide), or meglitinides, there is an increased risk of hypoglycaemia. The SmPCs for these medications advise considering dose reduction of insulin or sulfonylureas when initiating weight loss injections to minimise this risk. Patients should be educated about hypoglycaemia symptoms and advised to monitor blood glucose levels more frequently during the initial treatment period. Importantly, insulin should never be abruptly reduced or stopped when starting a GLP-1 receptor agonist, as this could lead to diabetic ketoacidosis. Metformin can generally be continued without dose adjustment.
Oral medications with narrow therapeutic windows may be affected by the delayed gastric emptying caused by GLP-1 receptor agonists. For patients taking levothyroxine, thyroid function should be monitored, as semaglutide may increase T4 exposure.
Warfarin and other anticoagulants require careful monitoring, as weight loss and dietary changes can affect INR stability. More frequent INR checks may be necessary when initiating weight loss injections in patients taking warfarin.
Co-administration with other GLP-1 receptor agonists is not recommended, and there is limited experience combining these medications with other weight-loss medicines. Always inform your GP and pharmacist about all medications, including over-the-counter products and herbal supplements, before starting weight loss injections. If you experience any unusual side effects, report them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Pregnancy, Breastfeeding and Weight Loss Injections
Weight loss injections should not be used during pregnancy. For semaglutide (Wegovy), treatment should be discontinued at least two months before a planned pregnancy, while liraglutide (Saxenda) should be stopped before pregnancy (with no specific lead time stated in the SmPC). GLP-1 receptor agonists have been shown to cross the placental barrier in animal studies, and animal studies have shown potential risks to foetal development. Due to insufficient human safety data, these medications should not be used during pregnancy.
Women of childbearing potential must use effective contraception throughout treatment. If pregnancy occurs whilst taking weight loss injections, the medication should be stopped immediately, and the patient should contact their GP or maternity services promptly. The focus during pregnancy should shift to appropriate nutritional support and gestational weight management under specialist obstetric guidance rather than pharmacological weight loss.
Breastfeeding mothers should not use weight loss injections. It is unknown whether GLP-1 receptor agonists are excreted in human breast milk, but due to insufficient data and potential risks, these medications are not recommended during lactation. Women should discuss alternative weight management strategies with their healthcare provider, focusing on balanced nutrition and gradual, sustainable weight loss postpartum.
For women planning pregnancy, a comprehensive discussion with their GP is essential. This should include optimising weight before conception through lifestyle modifications, reviewing all medications for pregnancy safety, and ensuring adequate folic acid supplementation. Weight management during the preconception period may improve fertility outcomes and reduce pregnancy complications, but this should be achieved through evidence-based lifestyle interventions rather than pharmacological agents. The postnatal period offers an opportunity to reassess weight management goals once breastfeeding is complete, with weight loss injections potentially considered as part of a comprehensive approach if clinically appropriate.
Age Restrictions and Safety Considerations
Weight loss injections have specific age-related restrictions that reflect the available clinical evidence and safety data. In the UK, most GLP-1 receptor agonists for weight management are licensed for adults aged 18 years and over. Use in children and adolescents under 18 is generally not recommended outside specialist settings, though specific products may have different licensing. Always check the current SmPC for the most up-to-date information on age restrictions.
The lack of extensive paediatric data means that safety profiles, appropriate dosing, and long-term effects on growth and development remain inadequately characterised for younger populations. Adolescent obesity management should primarily focus on family-based lifestyle interventions, dietary modification, and increased physical activity, with pharmacological treatment reserved for exceptional cases under specialist care.
Older adults aged 65 and above can use weight loss injections, but require careful assessment and monitoring. Age-related physiological changes, including reduced renal function, altered drug metabolism, and increased frailty, necessitate individualised treatment approaches. Elderly patients may be more susceptible to adverse effects such as dehydration, particularly if experiencing nausea, vomiting, or diarrhoea. These gastrointestinal symptoms can lead to reduced oral intake and electrolyte imbalances, which pose greater risks in older individuals.
Sarcopenia (age-related muscle loss) represents another consideration in elderly patients. Rapid weight loss without adequate protein intake and resistance exercise may accelerate muscle mass decline, increasing fall risk and functional impairment. A comprehensive assessment of frailty, hydration status, polypharmacy, and risk of malnutrition is advisable before initiating treatment in older adults.
Frail elderly patients or those with multiple comorbidities, polypharmacy, or cognitive impairment may not be suitable candidates for weight loss injections. The complexity of self-administration, dietary management, and monitoring requirements may prove challenging. Healthcare providers should assess each patient's functional status, support network, and ability to recognise and report adverse effects before prescribing these medications to older adults.
When to Speak to Your GP About Weight Loss Injections
Consulting your GP is an essential first step if you are considering weight loss injections. Your doctor will assess your suitability through a comprehensive evaluation including your body mass index (BMI), medical history, current medications, and previous weight loss attempts. In the UK, GLP-1 receptor agonists for weight management are typically prescribed within specialist weight management services for adults with a BMI of 35 kg/m² or above (or 32.5 kg/m² for people from South Asian, Chinese, other Asian, Middle Eastern, Black African, or African-Caribbean backgrounds) who also have at least one weight-related comorbidity. Treatment duration is typically limited (e.g., 2 years for semaglutide).
You should arrange an appointment to discuss weight loss injections if you have struggled to lose weight through lifestyle modifications alone, have obesity-related health conditions such as type 2 diabetes, hypertension, or obstructive sleep apnoea, or if your weight is significantly impacting your quality of life and physical function. Your GP can provide referral to appropriate weight management services and ensure you receive comprehensive support.
Seek urgent medical advice if you experience any of the following whilst taking weight loss injections: severe, persistent abdominal pain (which may indicate pancreatitis), signs of allergic reaction including facial swelling, difficulty breathing, or widespread rash (call 999 for suspected anaphylaxis), symptoms of thyroid problems such as a lump in the neck, persistent hoarseness, or difficulty swallowing, severe dehydration with dizziness, reduced urination, or confusion, or symptoms of gallbladder disease including right upper abdominal pain, particularly after eating, accompanied by nausea or fever. Also seek prompt medical advice if you experience new or worsening depression, thoughts of self-harm, or other significant mood changes.
Regular follow-up appointments are essential for monitoring treatment response, managing side effects, and assessing ongoing suitability. Your GP or specialist will typically review your progress every three to six months, checking weight loss, tolerability, and any changes in your medical conditions or medications. If weight loss is inadequate (typically less than 5% body weight after 12 weeks at maintenance dose) or if you experience intolerable side effects, your healthcare provider will discuss alternative strategies. Remember that weight loss injections are most effective when combined with sustainable lifestyle changes, including a balanced, calorie-controlled diet and regular physical activity, supported by ongoing professional guidance.
Frequently Asked Questions
Can I take weight loss injections if I have type 1 diabetes?
No, weight loss injections such as semaglutide and liraglutide are not appropriate for people with type 1 diabetes. These GLP-1 receptor agonists are specifically designed for type 2 diabetes and obesity management and should not be used as a substitute for insulin therapy.
Are weight loss injections safe during pregnancy?
No, weight loss injections should not be used during pregnancy due to insufficient human safety data and potential risks to foetal development. Semaglutide should be discontinued at least two months before a planned pregnancy, and treatment must be stopped immediately if pregnancy occurs.
What should I do if I experience severe abdominal pain whilst taking weight loss injections?
Seek urgent medical advice if you experience severe, persistent abdominal pain whilst taking weight loss injections, as this may indicate pancreatitis. Contact your GP immediately or attend A&E if the pain is severe or accompanied by vomiting or fever.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












