Is it hard to get Ozempic in the UK? Yes, obtaining Ozempic has become significantly more difficult since 2022 due to widespread supply shortages affecting both NHS and private prescriptions. Unprecedented demand—driven largely by off-label use for weight loss—has exceeded manufacturing capacity, creating persistent availability challenges. NHS England has prioritised Ozempic for its licensed indication, type 2 diabetes, whilst supply constraints have limited access through private providers. This article examines why Ozempic shortages persist, NHS eligibility criteria, private prescription options, suitable alternatives, and practical steps if you cannot access this medication.
Summary: Yes, obtaining Ozempic in the UK has become difficult due to significant supply shortages caused by demand exceeding manufacturing capacity, affecting both NHS and private prescriptions.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK specifically for type 2 diabetes management, not weight loss.
- NHS prescribing follows NICE guideline NG28, requiring inadequate glycaemic control despite optimised therapy and specific BMI thresholds with weight-related comorbidities.
- Supply shortages since 2022 stem from off-label prescribing for weight loss, complex manufacturing processes, and global demand outpacing production.
- NHS England has issued National Patient Safety Alerts prioritising Ozempic for diabetes patients over off-label weight management use.
- Alternative GLP-1 receptor agonists include Trulicity (dulaglutide) and Victoza (liraglutide); never stop Ozempic without medical guidance to avoid glycaemic deterioration.
- The MHRA has detected counterfeit Ozempic pens in UK supply chains; obtain medication only from regulated pharmacies and registered prescribers.
Table of Contents
Why Ozempic Availability Has Become Limited in the UK
The manufacturer, Novo Nordisk, has struggled to scale production rapidly enough to meet this surge. The complex manufacturing process for GLP-1 receptor agonists requires specialised facilities and extended production timelines, meaning supply cannot be increased quickly. Additionally, global demand has created competition for available stock, with multiple countries experiencing similar shortages.
NHS England and the Department of Health and Social Care (DHSC) have issued National Patient Safety Alerts and Medicines Supply Notifications regarding these shortages. These alerts have prioritised Ozempic for its licensed indication—type 2 diabetes—rather than off-label weight management. This approach aims to ensure that patients with diabetes, who rely on Ozempic for glycaemic control, are not disadvantaged by supply constraints. While semaglutide has demonstrated cardiovascular benefits in clinical trials (SUSTAIN-6), its UK licence is specifically for glycaemic control in type 2 diabetes.
Social media and celebrity endorsements have further amplified public interest in semaglutide for weight loss, creating additional pressure on supply chains. This phenomenon has prompted healthcare regulators and professional bodies to emphasise that Ozempic should be prescribed according to evidence-based clinical need rather than cosmetic preferences. The MHRA has also issued alerts about counterfeit Ozempic pens detected in parts of the UK supply chain, highlighting the importance of obtaining medication only from regulated sources.
The supply situation remains dynamic, with periodic improvements followed by renewed shortages as demand continues to outpace production capacity. Patients and healthcare professionals should regularly check DHSC and NHS England updates for the latest information.
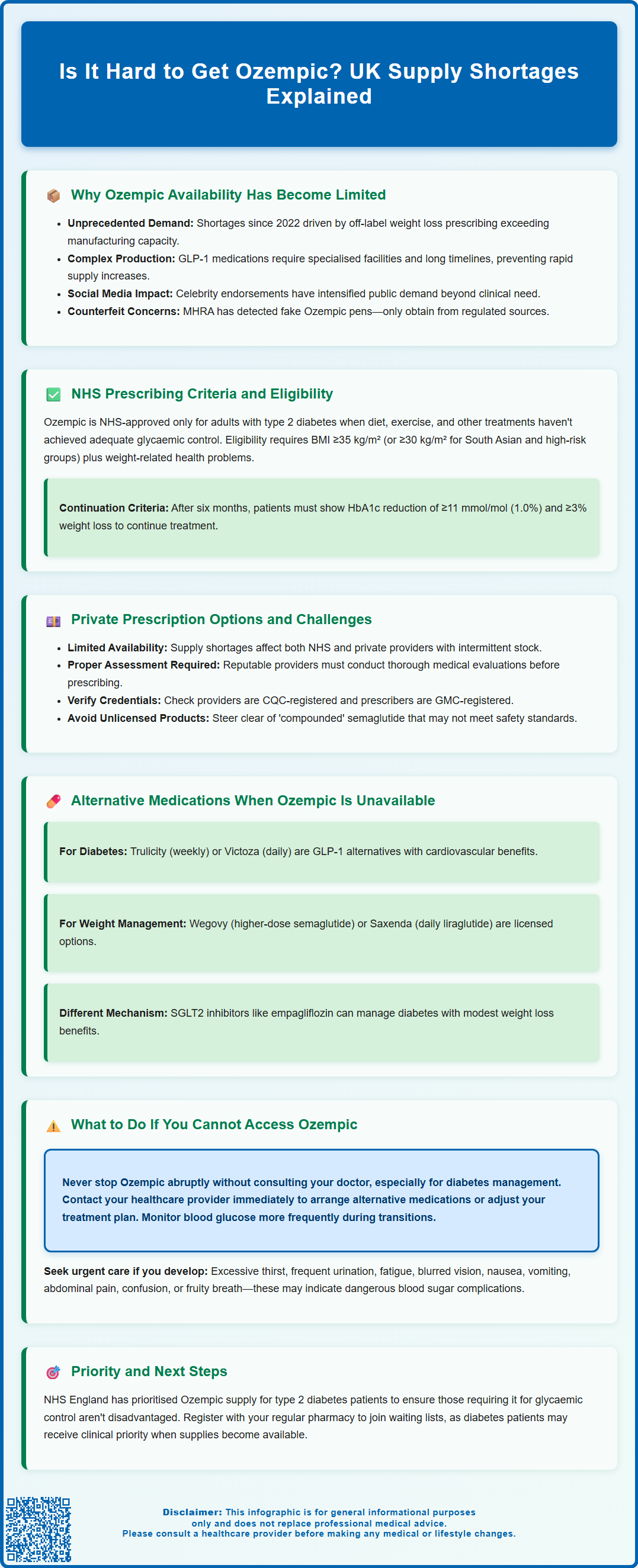
NHS Prescribing Criteria and Eligibility for Ozempic
Access to Ozempic through the NHS is governed by strict clinical criteria established by the National Institute for Health and Care Excellence (NICE). Ozempic is approved for adults with type 2 diabetes as an adjunct to diet and exercise when other treatments have proven inadequate. According to NICE guideline NG28, GLP-1 receptor agonists like Ozempic should typically be considered when:
-
Triple therapy with oral medications is not effective, not tolerated, or contraindicated
-
HbA1c remains above the person's individually agreed target despite optimised therapy
-
Body mass index (BMI) is ≥35 kg/m² in people of White European descent (with adjustment for other ethnic groups, e.g., ≥30 kg/m² for those of South Asian or other high-risk ethnic backgrounds)
-
Weight-related comorbidities are present or lower BMI thresholds apply due to occupational implications or weight-related psychological problems
Patients must also demonstrate commitment to lifestyle modification programmes. Treatment continuation on the NHS requires documented clinical benefit, typically defined as HbA1c reduction of at least 11 mmol/mol (1.0%) and weight loss of at least 3% of initial body weight at six months, as specified in NICE NG28.
It is important to note that Ozempic is not currently approved by NICE for weight management alone in people without diabetes. For obesity treatment, NICE has separately evaluated Wegovy (semaglutide 2.4mg) in technology appraisal TA875, which has different prescribing criteria. NHS England has issued additional guidance during supply shortages, reinforcing that Ozempic should be reserved for patients with type 2 diabetes and that off-label prescribing for weight loss should be avoided to protect supply for those with the licensed indication.
GP practices and diabetes specialist services follow these criteria when initiating or continuing Ozempic prescriptions, and current supply constraints have made adherence to these guidelines even more stringent.
Private Prescription Options and Current Supply Challenges
Private prescriptions for Ozempic have become increasingly sought after, particularly by individuals seeking weight management without meeting NHS criteria. However, obtaining Ozempic privately has become substantially more difficult due to the same supply constraints affecting NHS provision. Many private clinics, online prescribing services, and community pharmacies have experienced intermittent or complete unavailability of Ozempic stock.
When Ozempic is available privately, costs vary considerably depending on the dose and provider. Private prescribers should conduct thorough medical assessments before initiating treatment, including review of medical history, current medications, contraindications, and baseline measurements. Reputable private providers will follow similar clinical protocols to NHS services, ensuring appropriate patient selection and monitoring.
Different regulatory bodies oversee various aspects of private prescribing:
-
The Care Quality Commission (CQC) regulates healthcare providers, including private clinics and online services
-
The General Medical Council (GMC) oversees standards for doctors, including their prescribing practices
-
The General Pharmaceutical Council (GPhC) regulates pharmacies and pharmacists
-
The Medicines and Healthcare products Regulatory Agency (MHRA) enforces medicines legislation and monitors safety
These regulators have established standards emphasising that:
-
Clinical need should take precedence over patient preference for cosmetic weight loss
-
Prescribers must ensure adequate monitoring and follow-up arrangements
-
Patients should be informed about supply uncertainties and potential treatment interruptions
-
Alternative evidence-based options should be discussed when Ozempic is unavailable
Some online prescribing services have faced regulatory scrutiny for inadequate assessment processes or prioritising commercial interests over patient safety. Patients considering private treatment should verify that providers are registered with the CQC and that prescribers are GMC-registered. It's also essential to avoid purchasing unlicensed or 'compounded' semaglutide products, which may not meet quality standards and could pose safety risks.
During periods of shortage, even patients with established private prescriptions may experience difficulties obtaining refills, necessitating discussions with prescribers about alternative treatment options. Any changes to treatment should be clinician-led and comply with the medicine's Summary of Product Characteristics (SmPC).
Alternative Medications When Ozempic Is Unavailable
When Ozempic cannot be obtained, several alternative medications may be appropriate depending on the clinical indication. For type 2 diabetes management, other GLP-1 receptor agonists with similar mechanisms of action include:
-
Trulicity (dulaglutide): Once-weekly injection with comparable efficacy for glycaemic control; has demonstrated cardiovascular benefits in the REWIND trial
-
Victoza (liraglutide): Daily injection with an established safety profile; has shown cardiovascular benefits in the LEADER trial
-
Bydureon (exenatide extended-release): Once-weekly option, though less commonly prescribed currently
It's worth noting that these alternatives may also be experiencing supply constraints, so availability should be checked before switching. These medications work through the same physiological pathway as Ozempic—enhancing glucose-dependent insulin secretion, suppressing inappropriate glucagon release, and slowing gastric emptying. When switching between GLP-1 receptor agonists, follow SmPC and BNF guidance, as individual responses and tolerability may vary. Your diabetes specialist or GP can advise on the most suitable alternative based on your specific clinical circumstances.
For patients who were using Ozempic primarily for weight management (whether on- or off-label), alternatives include:
-
Wegovy (semaglutide 2.4mg): The higher-dose formulation specifically licensed for obesity treatment (NICE TA875), though this has also experienced supply constraints
-
Saxenda (liraglutide 3.0mg): Daily injection approved for weight management (NICE TA664)
-
Orlistat: Oral medication that reduces fat absorption, available both on prescription and over-the-counter (as Alli); has modest efficacy and specific dietary requirements
-
Structured weight management programmes: NHS or private programmes incorporating dietary modification, physical activity, and behavioural support
NICE guidance emphasises that pharmacological treatments for obesity should always be combined with comprehensive lifestyle modification programmes. For some patients, other medication classes such as SGLT2 inhibitors (e.g., empagliflozin, dapagliflozin) may be appropriate for diabetes management and can provide modest weight loss benefits, though their primary mechanism differs from GLP-1 receptor agonists.
It is essential never to abruptly stop Ozempic without medical guidance, particularly for diabetes management, as this may lead to deterioration in glycaemic control. Always consult your prescriber before making any changes to your diabetes or weight management regimen.
What to Do If You Cannot Access Ozempic
If you are currently prescribed Ozempic and cannot obtain your medication due to supply shortages, contact your prescribing healthcare professional immediately—do not simply stop treatment. Your GP or diabetes specialist can:
-
Arrange a suitable alternative medication with similar therapeutic benefits
-
Adjust your diabetes management plan to maintain glycaemic control
-
Provide guidance on monitoring your blood glucose levels during the transition
-
Review your overall treatment strategy to ensure continued metabolic control
For patients with type 2 diabetes, maintaining glycaemic control is crucial to prevent both acute complications and long-term microvascular and macrovascular damage. Your healthcare team may recommend temporarily increasing the frequency of blood glucose monitoring during any treatment transition. They might also consider adjusting existing medications, adding additional oral antidiabetic agents, or switching to alternative injectable therapies.
If you were using Ozempic for weight management, discuss evidence-based alternatives with your healthcare provider. This conversation should include:
-
Assessment of clinical need: Determining whether pharmacological treatment remains appropriate
-
Alternative medications: Exploring other licensed weight management options
-
Enhanced lifestyle interventions: Referral to specialist weight management services, dietetic support, or structured programmes
-
Realistic expectations: Understanding that sustainable weight management typically requires long-term behavioural changes rather than medication alone
When to seek urgent medical advice:
-
If you experience symptoms of hyperglycaemia (excessive thirst, frequent urination, fatigue, blurred vision) after stopping or reducing Ozempic
-
If you develop symptoms of diabetic ketoacidosis (nausea, vomiting, abdominal pain, confusion, fruity-smelling breath)—particularly if you have other risk factors such as reduced insulin production or concurrent illness
-
If you have concerns about managing your diabetes during treatment changes
For urgent concerns, contact NHS 111 or your local urgent care service. Follow any sick-day rules provided by your healthcare team, which typically include more frequent glucose monitoring and maintaining hydration.
Patients should also be aware that supply situations can change relatively quickly. Maintaining regular contact with your pharmacy and prescriber can help you access Ozempic when stock becomes available. Some pharmacies maintain waiting lists for patients with clinical priority, particularly those using Ozempic for its licensed diabetes indication. Register with your usual pharmacy to be notified when supplies arrive.
If you experience any suspected side effects from Ozempic or alternative medications, report them through the MHRA Yellow Card scheme, which helps monitor the safety of medicines in the UK.
Frequently Asked Questions
Why is Ozempic so difficult to obtain in the UK?
Ozempic shortages result from unprecedented demand—largely driven by off-label prescribing for weight loss—exceeding manufacturing capacity. Novo Nordisk has struggled to scale production quickly enough, and NHS England has prioritised supply for patients with type 2 diabetes, the medication's licensed indication.
Can I get Ozempic on the NHS for weight loss?
No, Ozempic is not approved by NICE for weight management alone. NHS prescribing is restricted to adults with type 2 diabetes who meet specific criteria under NICE guideline NG28, including inadequate glycaemic control and defined BMI thresholds with weight-related comorbidities.
What should I do if I cannot get my Ozempic prescription filled?
Contact your prescribing healthcare professional immediately—do not stop treatment without medical guidance. Your GP or diabetes specialist can arrange suitable alternatives such as Trulicity or Victoza, adjust your diabetes management plan, and provide monitoring guidance to maintain glycaemic control during the transition.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript